Journal of Case Studies - Juniper Publishers
Abstract
This observation shows a combination of primary multiple tumors, where one of the tumor localizations is the cervix, the other is the mammary gland, the third is the lung.
For differential diagnosis in cases of primary multiple tumors, the most informative is CT of the lungs, PET-CT, ultrasound of the pelvic organs and abdominal cavity, histological examination, immunohistochemical examination. In case of difficulties in differential diagnosis, it is possible to perform extended genetic testing of frequent somatic mutations in the TP53, GATA3, EGFR, KRAS, NRAS, ESR, PIK3CA, AKT genes, which allows you to determine the source of metastasis, and in this regard, select the necessary antitumor therapy.
Despite the progression of cervical cancer (metastases to the supraclavicular lymph nodes), the patient was not denied specialized treatment for lung cancer. The multidisciplinary approach adopted in the clinic in the diagnosis and treatment of patients made it possible to detect a malignant lung tumor at the preclinical stage and perform a radical operation, which allows us to hope for a good long-term result. At the same time, the metastatic lesion was not confirmed, the data of pathomorphological examination and immunohistochemical studies established an independent primary nature of the tumor.
Keywords: Metachronous cervical cancer; Cervical cancer; Recurrence
Introduction
Cervical cancer (CC) is the second most common cancer among women under 65 years of age and is the most common cause of death from gynecological cancer worldwide. In terms of morbidity and mortality, cervical cancer ranks fourth among all cancers. In 2020, there were 604,127 new cases of cervical cancer and 341,831 deaths worldwide. In the structure of mortality from malignant neoplasms in women under 45 years of age, cervical cancer ranks 1st. Tumors with localization in the cervix, mammary gland, lungs and other organs are not casuistry, but represent an extremely complex and not fully resolved problem of oncology. In the available literature, we did not find a combination of primary multiple cancers of the breast, lung and cervix. The frequency of metachronous tumors in women reaches 4.5%. We present to your attention an extremely rare case - the presence of primary multiple metachronous cervical cancer.
Patient S., 60 years old, applied to the Novosibirsk Regional Clinical Oncological Center in 2014 with a diagnosis of breast cancer III st T2N1M0. - radical left-sided mastectomy with lymphadenectomy.
Histological examination No. 26854-69 dated August 27, 2014. Conclusion: infiltrating ductal cancer of the left breast, maligna II with growth in the vessels, secondary changes in two lymph nodes.
Immunohistochemical study dated 09/04/2014. - ER 8, PR 6, Her2neo 1+ Ki67 - 25%. Adjuvant radiation therapy was prescribed - a dose of 46-50Gy for 23-25 fractions 5 times a week for the operated mammary gland, supra-/subclavian, ipsilateral parasternal and part of the axillary zone (as a zone of special risk) ROD 2Gy, SOD 45-50Gy.
Polychemotherapy courses - according to the FAC scheme: Cyclophosphamide 800mg, Doxorubicin 80mg, 5 fluorouracil 800mg 4 courses, hormone therapy with Tamoxifen 20mg. The patient was registered with an oncologist and regularly underwent examinations.
In 2015, cervical cancer II st T2bN0M0 was diagnosed, cervical biopsy No. 30867-79 dated 10/14/2015. - squamous cell nonkeratinizing cancer.
Courses of chemoradiation therapy, remote beam therapy in a total dose of 45-50Gy, simultaneously with chemotherapy (3 cycles of cisplatin 50mg each week) followed by brachytherapy, EBRT - 2Gy per fraction, in the irradiation mode 5 times a week, were carried out. The total dose to the focus from combined radiation therapy was 75Gy, to the lymphatic outflow path - 58Gy.
In 2017, according to the results of a histological examination dated February 21, 2017. - Metastasis of squamous cell carcinoma of the cervix to the supraclavicular lymph nodes on the left, courses of polychemotherapy Paclitaxel 175 mg/m2 IV 3 hours on the 1st day + Doxorubicin - 8 courses, completed in September 2017, palliative course of radiation therapy to the region of the supraclavicular lymph nodes on right. According to the control studies - stabilization of the process.
In February 2020, according to the results of bone scintigraphy - metastases in the bones of the spine Th8-Th10, reactive strontium therapy was prescribed, Fulvestrant 500mg 1 time in 28 days/m, continued growth of Th8-Th10, Palbociclib was added from 02.2020.
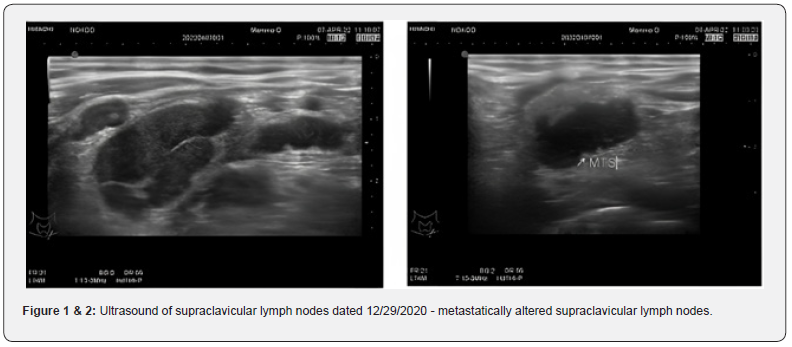
Ultrasound of the supraclavicular lymph nodes from 12/29/2020 - on the left: multiple (9) hypoechoic with clear and fuzzy contours ranging in size from 3 to 12mm (previously from 3 to 10mm) are located (Figure 1 & 2).
01/13/2021 - excisional biopsy of supraclavicular lymph nodes on the left.
01/20/2021 Histological examination of surgical material: No. 442-5/21: the histological picture and immunophenotype of tumor cells correspond to metastases of squamous cell carcinoma, taking into account the expression to p16 (Clone CINtec, Ventana) - carcinoma of the cervix.
MRI of the pelvis from 01/19/2021 - no pathology was detected.
Ultrasound of the abdominal organs from 01/29/2021 - echo signs of a liver cyst, a cyst of the left kidney, diffuse changes in the liver parenchyma, pancreas.
02/08/2021 - concilium - chemotherapy is indicated according to the scheme: Paclitaxel 175mg/m2 IV drip + Cisplatin 75mg/m2 IV drip on day 1 Cycle 1 time in 21 days, up to 6 courses with an assessment of the effect after 3 and a decision issue of radiation therapy 6 cycles of chemotherapy were performed (treatment was completed on 05/25/2021) MRI of the pelvis from 12/09/2021 - MRI signs: - abdominal infiltrate of the uterine bladder tissue with inhomogeneous contents and air with fistulas in the bladder and vagina, - post-radiation changes in the pelvis .
To clarify the process, PET-CT of the whole body was performed: - In the parenchyma of the right lung, nodular metabolically active seals in S2 - 1.2 * 0.8cm, in S6 - 0.9 * 0.8cm. Infiltration of the small pelvis.
According to PET-CT of the whole body dated 02.11.2021. - zone of tissue resorption in the region of the alveolar process of the upper jaw.
Consultation of the maxillofacial surgeon from 02.11.2021 - More evidence for osteonecrosis with bisphosphonates.
Due to difficulties in diagnosing the zone of tissue resorption in the region of the alveolar process of the upper jaw, an extended genetic testing of frequent somatic mutations in the genes TP53, GATA3, EGFR, KRAS, NRAS, ESR, PIK3CA, AKT was performed in the laboratory of pharmacogenomics of the Institute of Chemical Biology and Fundamental Medicine SB RAS: in block 26854-56, a mutation was found in the GATA3 gene (chromosome 10, position 8115971 in the assembly of the human genome No. 19) with a content of 30.4% with a coverage of 171 reads; in block 30867, a mutation was found in the TP53 gene (chromosome 17, position 757754) in the assembly of the human genome 19 with a content of 1.15% with a coverage of 783 reads, a mutation in the TP53 gene (chromosome 17, position 7577541 in the assembly of the human genome No. 19) was found in plasma with a content of 1.86% with a coverage of 22872, respectively.
Conclusion: tumor DNA corresponding to sample 30867 (cervical cancer) circulates in blood plasma Concilium at the Novosibirsk Regional Clinical Oncological Dispensary dated January 12, 2022 - given the progression of the disease, continued tumor growth is indicated for monochemotherapy: Karboplatin AUC 5 IV 1 hour on the 1st day every 3 weeks, up to 6 courses in total (with an assessment of the effect after 3 and 6 courses - CT of the chest + MRI of the small pelvis) MSCT of the chest on March 18, 2022 - no dynamics.
MRI of the pelvic organs on March 18, 2022 - no dynamics.
6 courses of monochemotherapy with Carboplatin AUC 5 IV 1 hour on the 1st day every 3 weeks were carried out, treatment was completed in May 2022.
Since August 2021, a vesico-vaginal fistula was diagnosed (Figure 3), which significantly reduced the quality of life of the patient.
Examined by a urologist in May 2022, cystoscopy was performed: - Formations: on the right side wall with a transition to the posterior multiple small bullous-solid formations - a biopsy was taken, urine was taken for atypical cells, cytological examination - no atypia. Histological examination - Moderately expressed active cystitis. Tumor growth was not detected in the preparation.
In July 2022, a set of examinations was carried out: pelvic ultrasound, abdominal ultrasound, CT of the lungs, skeletal bone scan, PET-CT, and stabilization of the process was established.
In this regard, on July 20, 2022, fistuloplasty was performed at the Avicenna clinic (Figure 4-6), the postoperative period was uneventful, without complications, and she was discharged on the fifth day. The patient notes a significant improvement in the quality of life.
In August 2022 according to the results of follow-up examinations on CT scan of the lungs, there are signs of metastatic lesions of the upper and lower lobe of the right lung, videoassisted thoracoscopic upper lobectomy on the right with atypical resection of the lower lobe is recommended (Figure 7 & 8).
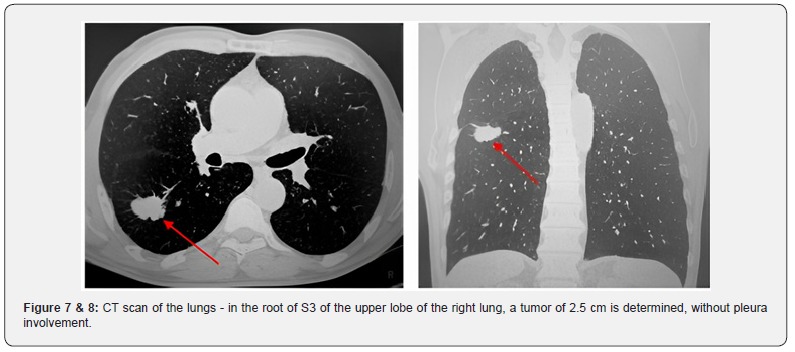
At the Institute of Oncology and Neurosurgery of the Federal State Budgetary Institution “N.N. ak. E.N. Meshalkin” 30.08.2022 - videothoracoscopic upper lobectomy on the right with atypical resection of the lower lobe. Intraoperatively: in the root of S3 of the upper lobe of the right lung, a tumor of 2.5cm was determined, without pleura involvement. In the lower lobe on the right S6, S8, S9, 3 subpleural foci are determined. Performed upper lobectomy with atypical resection of the lower lobe.
According to the pathomorphological study dated 09/02/2022. No. 10147-10168 - taking into account the morphology of the formation - the presence of a pronounced exophytic component, the tumor stem, the solidary nature of the neoplasm, the most likely primary highly differentiated keratinizing squamous cell carcinoma S3 of the bronchus of the upper lobe of the right lung, pT1cN0M0.
A revision of the pathomorphological report was performed at the Tomsk National Research Medical Center dated 09/08/2022. No. 10147-10168, where the diagnosis was also confirmed - primary highly differentiated keratinizing squamous cell carcinoma S3 of the bronchus of the upper lobe of the right lung, pT1cN0M0.
According to the ultrasound of the small pelvis, ultrasound of the abdominal cavity dated December 14, 2022. - no negative dynamics, signs of post-radiation changes.
According to CT of the chest organs dated November 22, 2022. - condition after surgical treatment of the right lung. There are no new foci, lung metastases without dynamics, metastases of Th8- Th10 bodies - without dynamics.
According to colposcopy dated 12/17/2022. - no local recurrence, post-radiation changes (Figure 9).
Conclusion
This observation shows a combination of primary multiple tumors, where one of the tumor localizations is the cervix, the other is the mammary gland, the third is the lung. Figure 7 & 8 - CT scan of the lungs - in the root of S3 of the upper lobe of the right lung, a tumor of 2.5 cm is determined, without pleura involvement.
1. For differential diagnosis in cases of primary multiple tumors, the most informative is CT of the lungs, PET-CT, ultrasound of the pelvic organs and abdominal cavity, histological examination, immunohistochemical examination.
In case of difficulties in differential diagnosis, it is possible to perform extended genetic testing of frequent somatic mutations in the TP53, GATA3, EGFR, KRAS, NRAS, ESR, PIK3CA, AKT genes, which allows you to determine the source of metastasis, and in this regard, select the necessary antitumor therapy.
2. Despite the progression of cervical cancer (metastases to the supraclavicular lymph nodes), the patient was not denied specialized treatment for lung cancer. The multidisciplinary approach adopted in the clinic in the diagnosis and treatment of patients made it possible to detect a malignant lung tumor at the preclinical stage and perform a radical operation, which allows us to hope for a good long-term result. At the same time, the metastatic lesion was not confirmed, the data of pathomorphological examination and immunohistochemical studies established an independent primary nature of the tumor.
3. In the treatment of primary multiple tumors, a multidisciplinary approach is required with the involvement of a thoracic surgeon, an oncogynecologist, an oncomammologist, a molecular oncologist, and a pathologist. The final conclusions on this issue can be obtained by accumulating a sufficient number of observations.
Therefore, each case of a primary multiple metachronous lesions should be especially carefully studied and presented in international medical literature.




No comments:
Post a Comment