Addiction & Rehabilitation Medicine - Juniper Publishers
Abstract
Alcohol abuse is one of the genuine social issues which is quickly expanding consistently. The quickest development is being seen in the non-industrial nations of Asia, more especially in India. Drinking of alcohol makes the existence of a man truly hopeless, alcohol debases the wellbeing of the individual as well as influences his family and society. Alcohol abuse is named as Madatyaya in Ayurveda, which is one among the way of lifestyle disorder, is additionally impairing habit-forming jumble. It has expanded at a disturbing rate around the world, even in India it is an issue of concern. The ailments caused by Madya in Mithya, Atiyoga and Heenayoga can be cured by taking the Madya in proper way and proper quantity (Samayoga). The classics of Ayurveda narrate this disease Madatyaya with its types, symptoms and treatment. Excessive consumption of Madya directly affects ‘Hridaya’, which is one of the vital organs of body and it is mainly associated with the Rasavaha srotas, Manovaha Srotas and oja. So, we are trying to describe effect of Madatyaya on human body.
Keywords: Madatyaya; Alcohol; Madya; Ayurveda; Alcoholism
Introduction
In Ayurvedic text alcoholism and its withdrawal are described under the heading of Madatyaya and makes Ayurveda very much capable to treat this condition [1]. In charak samhita Madya Varga classified under one of 12 Ahara Varga. It is utilized as Ahara Dravya (Food Supplement), as Anupana (After Drink) or as aushadhi (Medication). Based on use, Madya is categorized into two kinds as medication and as beverage. In Ayurveda based on techniques and natural substances used name of different preparations are: Asava, Arishta, Sura, Varuni and Sidhu. Out of these, initial two are utilized for medication and others for refreshment.
Madya is one which produces Mada. When given in appropriate amount, in time and in proper system, it brings joy, strength, lessens dread, strain. Furthermore, act as an Amrut (Nector) for the body [2]. The patient who has tamas and rajas manas prakruti will easily habituate for alcohol than satvik manas prakriti and vice-versa. In the absence of alcohol, continuous demand of it felt which is known as Panapkrama (Alcohol Withdrawal Syndrome) [3].
Review of Literature
i.Madatyaya has been explained in 24th chapter of Charaka Samhita after VishaChikitsa, in light of the fact that Madhya is having properties like Visha (poison). Charaka clarifies the Madhya Gunas (characteristics), phases of Madatyaya (Alcoholism), liquor addiction, their signs, side effects and Chikitsa (treatment).
ii.In Sushruta Samhita, UttaraTantra 47th chapter, Acharyas portrayed with regards to Madatyaya exhaustively for the sake of Panatyaya Pratisheda.
iii.In Astanga Samgraha, Madatyaya Chikitsa has been mentioned in ninth chapter of Chikitsa Sthana. It specifies Madhya Prayoga in Madatyaya and mentioned the treatment of Mada and Murcha.
iv.In Astanga Hrudaya, Nidana (causative factors) of Madatyaya has been clarified in sixth chapter of Nidan sthana, and in seventh chapter of Chikitsasthana the treatment of Mada (inebriation), Murcha (syncope), Sanyasa (unconsciousness) including Nidana (etiology), and Chikitsa (treatment) of Dwamsaka and Vikshaya has been clarified.
v.In Chikitsastana of Kashyapa Samhita, the author has clarified impacts of Madhya in pregnant ladies and newborn children with their treatment.
vi.In Madhava Nidana, Madatyaya is explained after Krumi Nidana.
vii.In BhavaPrakash, Madatyaya is clarified in Madyama Khanda after Murcha, Bhrama, Nidra,Tandra and Sanyas Adhikarna, trailed by DahaAdhikarana.
viii.Yogaratnakar has clarified a different chapter as Madatyaya Adhikara after Murchadhikara [4].
Effect of Madya
Madya incorporates Tridosha, Rasa and Rakta as dushya and Rasavaha, Raktavaha, Sangyavaha Shrotas. Hridaya is the principle adhisthan because of which people experience the ill effects of Ojakshaya, Dhatukshaya, Sharirkampa, Pralapa, Bhrama, AgniVikar, Anidra etc.
a. Madyaavastha (Acute Intoxication)
Acute intoxication is usually a consequence of deliberate heavy drinking either small doses at short intervals, or a large dose at a time.
b. Prathama Avastha (Stage of excitement)
The individual goes overthrill, enthusiastic, appropriate appearance of the traits of food and drink, and the insight and inventiveness of music, tune, humor and stories. This outcomes in strong rest and post-waking sensations. Subsequently, this phase of inebriation is conductive to joy [5].
c. Madhyama Avastha (Stage of in-coordination)
The individual frequently recalls things and regularly fails to remember them, his voice becomes unintelligible and confounded, and he talks sense and babble simultaneously. His development, pose, drinking, eating and talking all are improper [6].
d. Antima Avastha (Stage of narcosis)
Subsequent to intersection of second stage and in the start of the third stage, people become dormant like a messed up tree with his psyche tormented with inebriating morbidities and obviousness. However alive, he looks like dead individual. He becomes unequipped for perceiving satisfying things and companions. He was deprived of all joy for which he had taken liquor. He loses every sense of qualification of legitimate, cheerful and helpful things from some unacceptable, hopeless hurtful ones separately; along these lines, no shrewd individual will at any point prefer to put himself in such a phase of inebriation. He is denounced and reproached by all people and disdained by them. As the normal result of this extravagance, he experiences agonies and infections constantly [7].
e. Chronic Intoxication
Habitual drunkards are either psychotic or neurotic and usually take alcohol as a mean to escape from the stress and strains of life. They have been taking alcohol for a long and continued period.
f. Madatyaya
Madatyaya comprises of two words Mada and Atyay. Mada implies Harsh (Sense of wellbeing) Atyay implies Atikrama (excess). The excess intake of Madya cause poisonous impacts. Poisonous impacts depend upon the prakruti and dosh of the person [8,9]. In Sharangadhara Samhita while characterizing the term Madakari, Madhya is included in the drugs having Tamoguna predominently causes insanity are known as Madakari (intoxicants) [10].
Types of Madatyaya
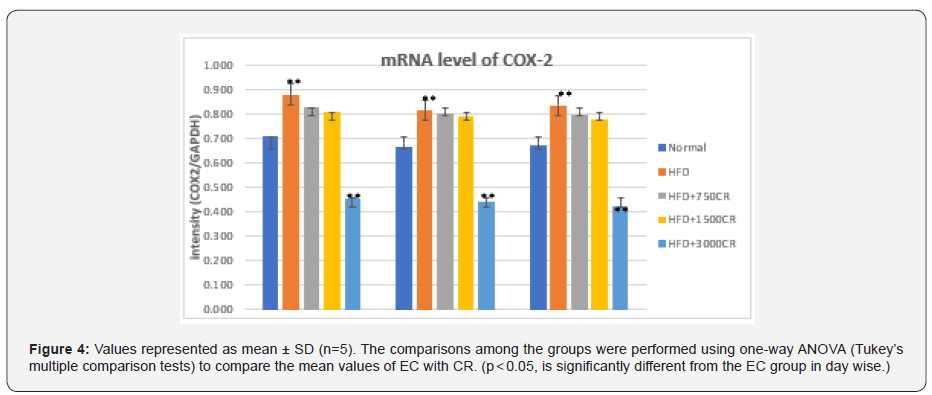
Madatyaya is Tridoshaja vyadhi. Its types named on Dosha which is dominating in presenting the symptoms. Charak explains types of Madatyaya as Vataja, Pittaja and Kaphaja and considers the disease as Tridoshaja.
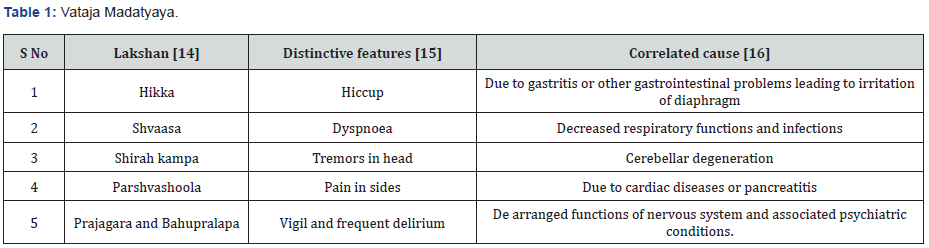
a. Vataja Madatyaya
Nidana: If a person is excessively emaciated because of Krodha, Shoka, Bhaya, Vyavaya, Chankramana, Sahasa, while eating Ruksha type of food, less quantity of food or limited quantity of food, drinks Madya at night which is excessively fermented, then this leads to the impairment of his Nidra and Vataja type of Madatyaya instantaneously develops [11].
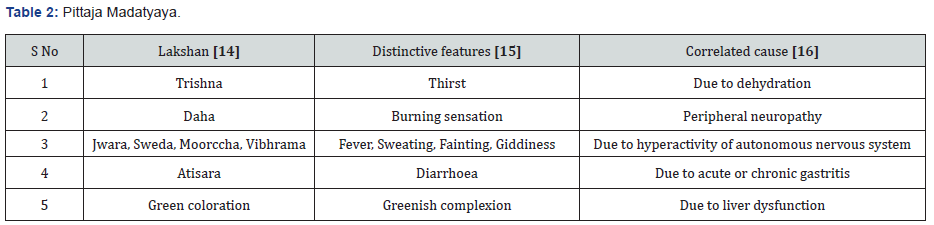
b. Pittaja Madatyaya
Nidana: If a person, indulging in food that is Amla, Ushna and Teekshņa, having wrathful disposition and having likeing for excessive exposure to the fire and sun, drinks excess quantity of Madya that is Teekshna, Ushna and Amla, then he suffers from the Pittaja type of Madatyaya [12].
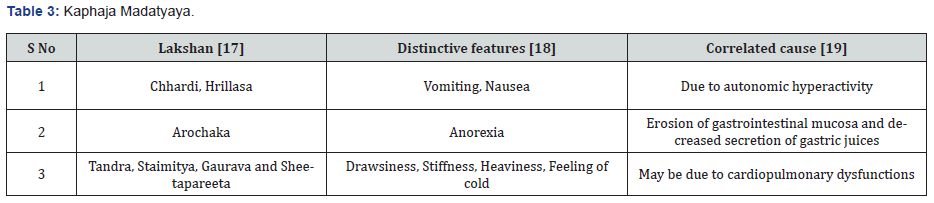
c. Kaphaja Madatyaya
Nidana: If a person who is habituated to Madhura, Snigdha and Guru Ahara, who does not perform Vyayam, who takes Diwaswapn and who indulges in Sukhaseenata, excessively drinks Madya which is not an old one or which is prepared of Guda, and Paishtika, then he immediately develops Kaphaja Madatyaya [13].
Upadrava of Madatyaya
Hikka associated with Jwara, Vamathu, Vepathu, Parshwashoola, Kasa and Bhrama [22].
Asadhya Lakshna
The following are the characteristics of Asadhya Lakshana: Heenottaraushitam, Atisheetam, Amandadaaham,Tailaprabhaasyam,Jihvaushtiha,Dantamasitam, Vaaneel and Peetanayana rudhirataa [23].
General Line of Treatment
All types of madatyaya are tridosaja.Treatment should be based on the dominant dosas.However,most of the time treatment is started for kapha dosa as pitta and vayu are manifested towards the end in most of the cases of madatyaya [24].
a. Counselling
i.Motivational counselling
ii.Group counselling
b. RelaxingTherapies: Musictherapy,Siropichu,Sirodhara,Ppadabhyang,Takradhara.
c. Padanshik Chikitsa Madya used in small amount or tapering doses.
d. Shodhana Chikitsa
i.If fit for Vamana- Sadyo vamana with Yastimadhu Phanta and Saindhava jala.
ii.If unfit for Shodhana- symptomatic treatment.
e. Shamana Chikitsa
Single drugs used
i.Brahmi
ii.Ashwagandha
iii.Bhringaraja
iv.Kushmanda
v.Jatamansi
vi.Shankhapushpi
vii.Mandukparni
viii.Guduchi
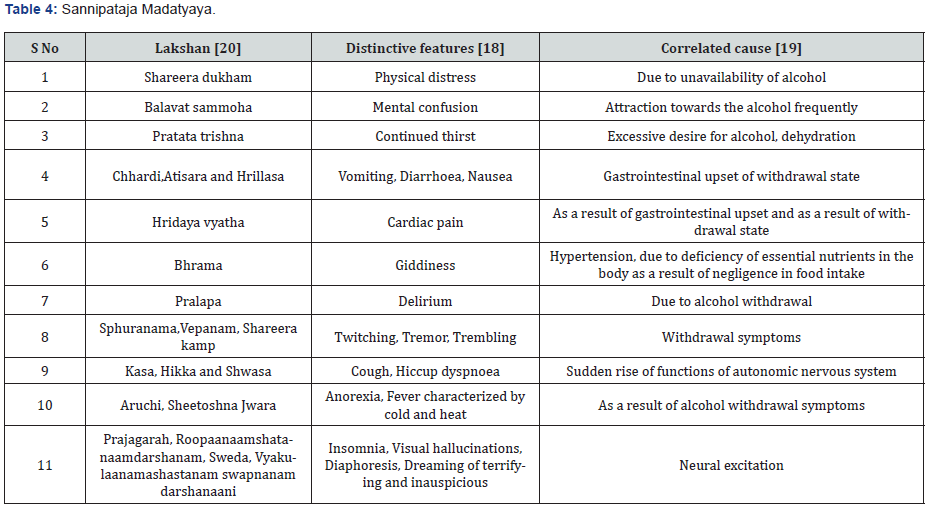
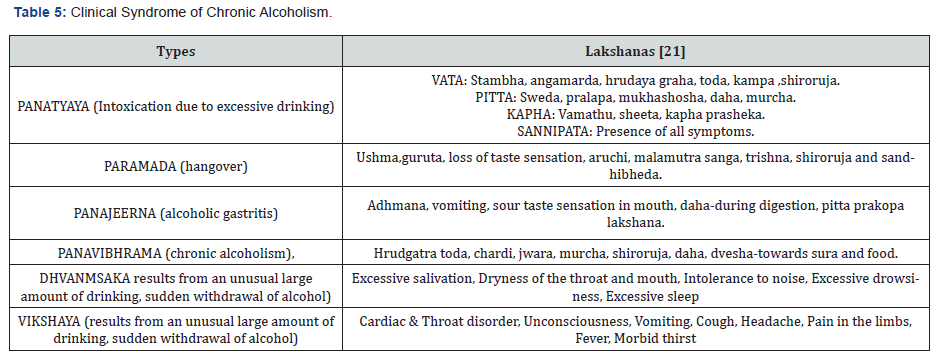
Discussion
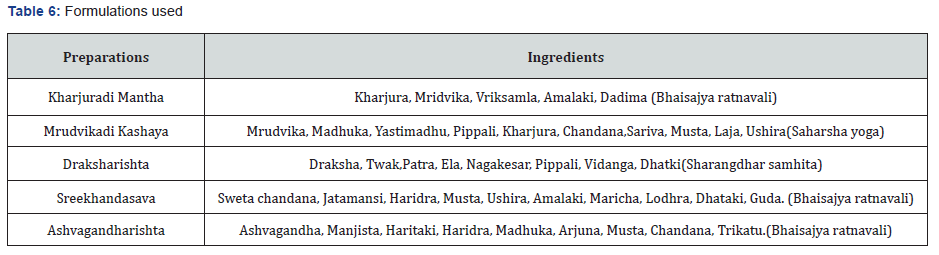
Alcohol whenever taken in appropriate way, time, with healthy food, in ideal proportion, as per own solidarity then it is pretty much as advantageous as Amrita. Generally, 80 % alcohol assimilate in small digestive system and significantly more utilized in liver that is the reason it shows its poisonous impact on liver and damages it. According to Ayurvedic texts Madatyaya has clinical manifestations like alcoholism. For any illness fundamental causative variables are unevenness of Dosha and Dushya. So, drug having Tridosha shamak impact, and which increases oja, bala, dhatu, having deepana, pachana, anulomana, yakrita uttejak, mutral, raktavardhak, raktashodhak, vishaghna, rasayan, medhya, hepatoprotective properties can be used judiciously for madatyaya.
In this way, Madatyaya described in Ayurveda can be correlated with chronic alcoholism and its complications upto some degree. Ayurveda has a unique understanding of human physiology and pathology, diagnosis and treatment. On sudden abstinence of alcohol, agni which maintains the equilibrium of the body gets altered, leading to the formation of ama. The ama causes srodhorodha (blockage of circulatory channels) and results in deficit of bala. The anulomana property of vata gets derranged and affects the functions of the body as well as mind. As we know that Madya for Madataya is the main Chikitsa Sutra mentioned in Ayurveda, play an important role in Alcohol Withdrawal, as sudden withdrawal may cause serious complication.
Madya which is used should be made up of particular medicinal herbs and given in tapering doses. Such a protocol seems safe as well as effective in the management of Alcohol withdrawal syndrome. Hence it is important to know the properties of Madya for understanding its effect on the body. It will be useful to minimize its hazardous action and in treating disease.Charaka Samhita discussed different formulations as per type of Madatyaya are Kharjooradi Mantha, Punarnavadi Ghrita, Ashtanga Lavana etc. It also quotes the Complications of untreated Madatyaya.
Conclusion
Subsequently, it is concluded that Madatyaya is well explained in Ayurveda, which helps in diagnosis and management depending on the involvement of the Dosha. Charak’s view towards alcoholism has great value because of its scientific literature study and description of physical & mental characteristic symptoms. Ayurveda also accept that it is cardiotoxic as well as dependent drug. Symptoms of pittaj madatyaya may be compared with alcoholic hepatitis. Concept of alcoholic addiction may be high lightened in terms of Dhwansaka & Vikshay. The chronic alcoholism may be compared with Pan Vibhram as mentioned. If we review & compare entire views of all Acharyas we can come to certain concrete conclusions regarding Madatyaya and its causes, symptoms, pathophysiology & excellent line of treatment that has been elaborately explained by Acharya charak and put intense light on the same, more effectively than other classical texts of ancient time.
The Ayurvedic management protocol along with the rehabilitation measures are effective in alleviating the symptoms of Alcohol withdrawal and associative conditions. Shamana therapy or even Shodhana therapy can be administered as per the severity of the condition of the affected person. One need to be careful in selection of appropriate procedure as it is based on Rogi and Roga Bala. Thus Ayurveda have ultimate and effective solution in the management and rehabilitation of madatyaya.
To Know more about Addiction & Rehabilitation Medicine
Click here: https://juniperpublishers.com/index.php