Journal of Otolaryngology - Juniper Publishers
Keywords: Sinusitis; Antibiotics; Antibiotic allergies; Oral challenges; Bacterial rhinosinusitis
Abbreviations: CPT: Procedure Code Terminal; PPO: Preferred Provider Organization; HMO: Health Maintenance Organization; CDHP: Consumer Directed Health Plan; HDHP: High Deductible Health Plan; OR: Odds Ratios; CI: Confidence Intervals; EMR: Electronic Medical Record
Introduction
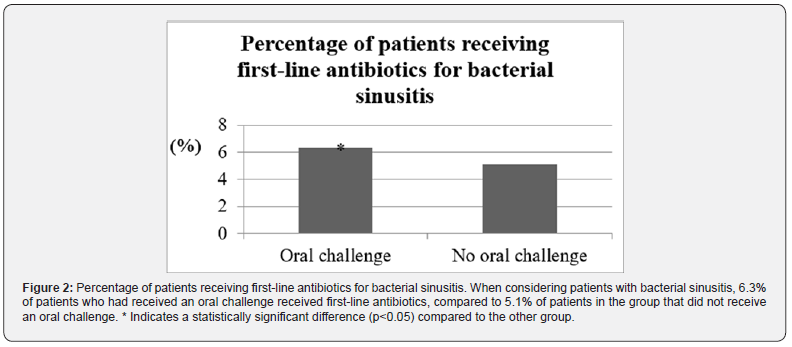
Beta-lactams, antibiotics that irreversibly inhibit the transpeptidation needed for bacterial cell wall synthesis, have been used for decades to treat a number of infections. Bacterial rhinosinusitis is most commonly caused by Streptococcus pneumoniae, Moraxella catarrhalis, and Haemophilus influenza [1]. A rhinosinusitis diagnosis requires purulent nasal discharge accompanied by facial pressure/pain/fullness and/or congestion of the nasal pathways [2]. Bacterial etiology is usually considered more likely over viral etiology if symptoms fail to improve within ten days or if there is an acute worsening of symptoms after prior improvement within the first ten days [1,2]. In the case of acute bacterial rhinosinusitis, the first-line treatment in adults is a five-to-seven-day course of high-dose amoxicillin-clavulanate [3].
Despite their broad utility for the treatment of rhinosinusitis among many other medical conditions, the use of beta-lactam antibiotics is often limited by the presence of penicillin allergy labels in patient medical records. In the United States, about 8% of the population report a penicillin allergy history; in practice, however, less than five percent of that group will acutely react to a full-dose oral challenge [4]. Several reasons may account for this over-estimated burden of penicillin allergy history. First, data shows that three-quarters of penicillin allergy labels are acquired before three years of age [5]. Many of these unnecessary labels are attributed to rashes, which are common features of many of the viral infections that affect the pediatric population [5]. Additionally, penicillin allergies tend to wane with time. Over ten years, for example, 80% of people with reaction histories to penicillin will no longer be allergic [6].
Given the prevalence of beta-lactam allergy labels and the well-defined detriments of carrying a penicillin allergy in one’s medical record, we sought to evaluate the impact of oral challenges on antibiotic prescribing practices for the treatment of acute bacterial sinusitis since first-line therapy is amoxicillin with clavulanic acid [3]. An oral challenge is a procedure commonly performed by an allergist in order to determine whether or not a patient is truly allergic to food, or medication in the case of this study. It specifically entails administering the substance in question in increasing amounts to patients while closely monitoring them for signs of an allergic reaction and is considered successful if the patient can tolerate it without difficulty. We hypothesized that drug oral challenges with subsequent antibiotic allergy delabeling increased the use of beta-lactam antibiotics for the treatment of acute bacterial sinusitis.
Methods
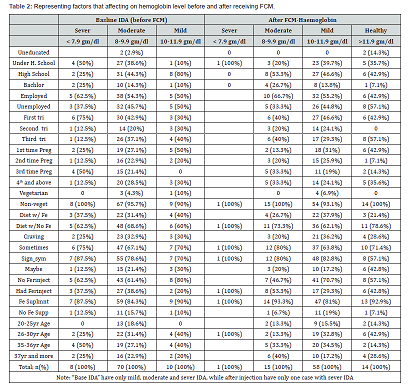
We performed a retrospective analysis using data from 2013 to 2018 from the Truven Health MarketScan Commercial Claims and Encounters database (hereby referred to as MarketScan). The database consists of reimbursed healthcare claims that include individual-level data of patients covered by diverse private insurance plans across all 50 US states and covers approximately 50 million privately insured individuals every year [7]. MarketScan (Cambridge, MA, USA) has information covering all insurance claims such as inpatient/outpatient claims, prescription drug claims, and other health care resource utilization claims. We included patients with no food allergy aged 18-64 who had at least one inpatient or outpatient medical claim for diagnosed acute sinusitis (using International Classification of Diseases, Ninth and Tenth Revision [ICD-9/ICD-10] code 461 and J01, respectively) from 2013 to 2018. Patients with food allergies were excluded because MarketScan is unable to differentiate food oral challenges from drug oral challenges.
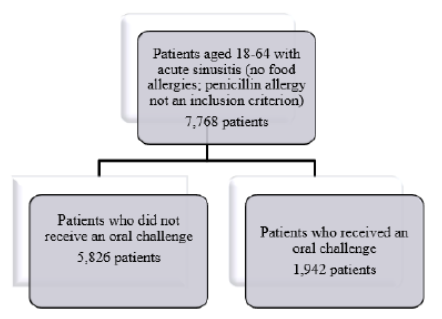
Furthermore, the presence of a penicillin allergy was not an inclusion criterion. The comparison groups were acute sinusitis patients who received oral challenge (Procedure code Terminal (CPT) 95076) compared with those who did not receive oral challenge. Each participant with oral challenge was matched to three participants without oral challenge, according to sex and year of birth (Figure 1). The main outcome of interest was the receipt of a first-line antibiotic (amoxicillin and amoxicillin/ clavulanic acid) within 30 days after the index date of an acute sinusitis diagnosis. Given the lack of statistical power caused by a small sample size, we were not able to examine other secondary outcomes such as infection with Clostridium difficile, multi-drug resistant organisms, and death. Demographic variables included age, sex, place of residence, and US regions. Another covariate of interest was insurance health plan types such as preferred provider organization (PPO), health maintenance organization (HMO), consumer directed health plan (CDHP), and high deductible health plan (HDHP).
SAS statistical software version 9.4 (SAS Institute, Cary, NC, USA) was used to conduct all statistical analysis using a two-tailed P value of < 0.05 as the significance level. We first examined the distribution of covariates between participants receiving oral challenges and those without. A multivariable analysis was conducted using conditional logistic regression models that accounted for matching variables, such as age and sex, and adjusting for place of residence (urban/rural) in US regions to estimate the adjusted odds ratios (aOR) and their 95% confidence intervals (CI). Crude OR was estimated using unadjusted conditional logistic regression that accounted for matching variables (age and sex). This study was approved by The Pennsylvania State University Institution Review Board.
Results
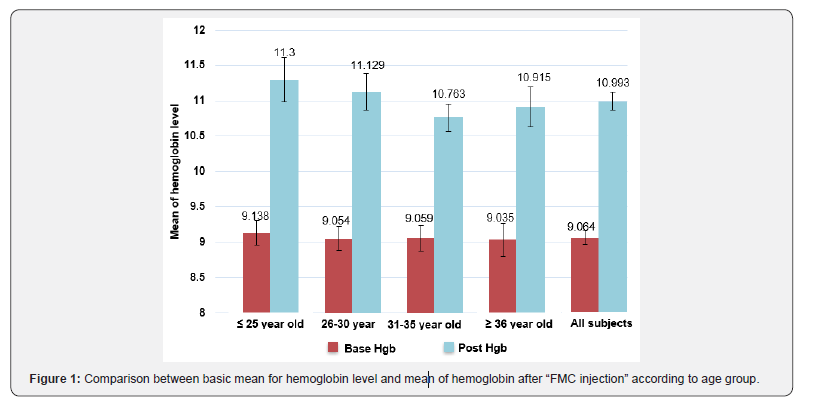
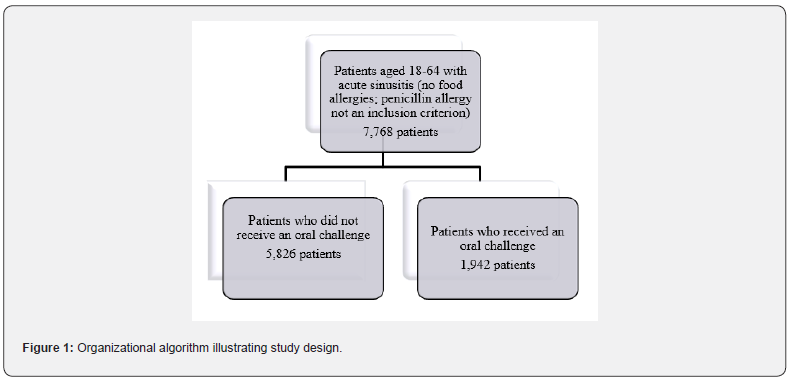
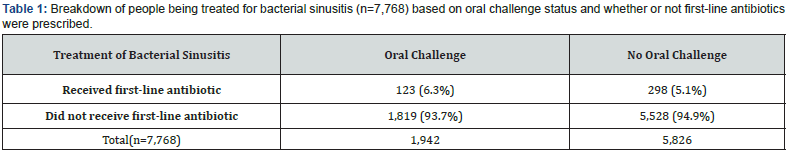
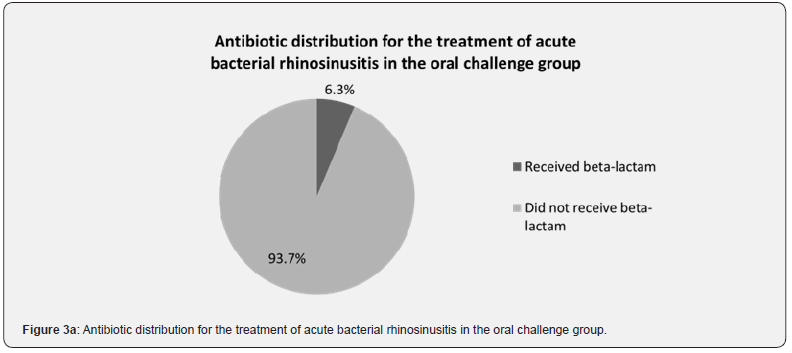
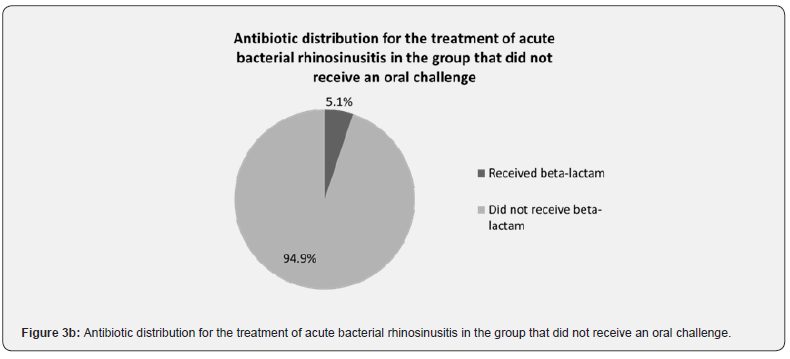
A total of 7,768 patients with bacterial sinusitis were included in the study (Table 1). Of these patients, 1,942 patients received an oral challenge, while 5,826 did not receive an oral challenge (Table 1). When considering patients who received the first-line beta-lactam-containing antibiotics, 6.3% (n=123) of the patients had received an oral challenge (Figure 2). This was significantly higher compared to the 5.1% (n=298) of patients who did not receive an oral challenge (Figure 2). When considering the converse, 93.7% (n=1,819) of patients who had received an oral challenge did not receive first-line antibiotics (Figure 3a). Additionally, 94.9% (n=5,528) of patients in the group without the oral challenge did not receive first-line antibiotics (Figure 3b).
Regardless of oral challenge status, however, an overwhelming majority of patients did not receive first-line antibiotics, which we assume is secondary to failure to remove the penicillin allergy designation versus inappropriate antibiotic prescribing practices.
Discussion
Data obtained from our research utilizing MarketScan demonstrate that patients who received an oral challenge were statistically more likely to receive the first-line beta-lactamcontaining antibiotics for the treatment of acute bacterial sinusitis compared to those who did not receive an oral challenge. Another key finding of this study was that, regardless of oral challenge status, first-line beta-lactam-containing antibiotics are not being frequently prescribed. While the data cannot provide any explanation for this finding, there may be a few reasons. First, the way a drug reaction is documented into the electronic medical record (EMR) can influence prescribing practices. A study conducted in Australia found that over 20% of reports of adverse drug reactions did not even include a description of the reaction [8]. Additionally, about 10% of the reports described as a penicillin allergy were actually more consistent with a drug intolerance, such as gastrointestinal symptoms [8].
Finally, a study conducted in a pediatric population in Saudi Arabia found that over 35% of antibiotic allergy descriptions in the EMR were “poor” [9]. From the perspective of antimicrobial stewardship, the presence of drug allergy labels, especially those that may be inaccurate, can be detrimental to both patients and to the healthcare system. Disadvantages of using alternate antibiotics include higher treatment costs, greater severity of side effects, and decreased treatment efficacy [5]. Additionally, a cohort study found that patients with a penicillin allergy label had significantly longer hospital stays and increased rates of infections with methicillin-resistant Staphylococcus aureus, Clostridium difficile, and vancomycin-resistant Enterococcus compared to those without a penicillin allergy label [10]. One study found that the presence of drug allergy labels was associated with increased use of quinolones and carbapenems and an overall increased rate of inappropriate use of antibiotics [11].
In the case of bacterial rhinosinusitis, second-line antibiotic treatments include doxycycline or respiratory fluoroquinolones (e.g., levofloxacin) [1,3]. The use of broad antibiotics such as levofloxacin can theoretically increase rates of antimicrobial resistance. Prior research found that S. pneumoniae-containing sputum samples had higher rates of antibiotic resistance (though not shown to be statistically significant) in patients with penicillin allergies compared to patients without penicillin allergies [12]. The presence of the penicillin drug allergy label in combination with a lack of meaningful reaction descriptions would likely deter clinicians from prescribing those antibiotics. The previously mentioned Australian study additionally found that the vast majority of the reaction descriptions could have warranted further evaluation and that about half of the documented histories appeared consistent with low-risk penicillin reactions [8]. Despite the demonstrated opportunities for further evaluation by allergists, the specialty is underutilized. For example, the study conducted in Saudi Arabia found that under 40% of the patients with concern for antibiotic allergies were referred for further evaluation [9].
Additional research showed that over 80% of research participants did not even know that penicillin drug allergy testing was available [13]. While these data show the potential impact of successful oral challenges, there are a number of limitations to the study. The most significant limitation was the small sample size of patients in the oral challenge group who received firstline antibiotics. A significant contributing factor to this limitation lies within the study design itself. As mentioned, the data was obtained through the use of MarketScan, which is limited to private insurance claims. As a result, the results are not directly generalizable to other kinds of insurance such as Medicare and Medicaid. Additionally, a diagnosis of food allergy was excluded from the patient population since MarketScan is unable to differentiate food oral challenges from drug oral challenges, subsequently reducing the generalizability of the provided data.
Finally, the CPT codes precluded us from being able to determine the identity of the drugs for which the oral challenges were intended or the outcomes of the oral challenges (e.g., whether or not the allergy label was removed from the medical record). Given how common beta-lactam allergies are, however, it is likely that the majority of the oral challenges were conducted for this particular class of medications. It should also be noted that MarketScan is unable to identify patients with a penicillin allergy label. Since the population studied is not definitively classified as having a penicillin allergy label, the reported difference in betalactam use for the treatment of acute bacterial rhinosinusitis between the group that has received an oral challenge versus the group that has not received an oral challenge could be an overestimation. While additional research is needed to better delineate the study population, the data interestingly highlights the lack with which these first-line antibiotics are used for acute bacterial rhinosinusitis.
Future work can focus on expanding the study population to include a broader array of insurance plans like Medicare and Medicaid. Given that most of the penicillin allergy labels are acquired during childhood, future studies might also be expanded to include the pediatric population. Such measures would likely increase sample size while broadening generalizability. Additionally, the types of antibiotics that are prescribed in place of these beta-lactams can also be examined. Finally, additional valuebased research can be conducted in order to further quantify the overall cost savings of drug oral challenges relative to the healthcare expenses associated with the use of alternative, less appropriate antibiotics.
While our study helps demonstrate the potential benefits of oral challenges, it appears that first-line antibiotics remain under-utilized even when allergy is excluded. In order to rectify this situation, further awareness (e.g., through the education of medical providers at all stages of training and practice) of the importance of penicillin allergy testing, penicillin challenges, education of the patient, and complete removal of a penicillin allergy label are crucial for promoting antimicrobial stewardship and improving health outcomes.
To Know more about Global Journal of Otolaryngology
Click here: https://juniperpublishers.com/gjo/index.php
To Know more about our Juniper Publishers
Click here: https://juniperpublishers.com/index.php