Head Neck & Spine Surgery - Juniper Publishers
Objective: Surgical management of cervical
instability and obtaining solid bone fusion in children is technically
challenging due to smaller
and immature anatomy besides the lack of pediatric-adapted
instrumentation. Optimizing fusion via additional bone grafting and
postoperative
HALO device application has been a topic of controversy. We describe our
experience with posterior cervical spine fusion techniques and re-visit
the role of autologous bone grafting.
Methods: We performed a retrospective chart
review of children, who underwent rigid instrumentation and/or onlay
bone graft fusion
between 2008 and 2019. The primary outcome was solid bone fusion at 2
years after surgery. Secondary outcomes were neurological outcome
and adverse events, including surgical and postoperative complications,
graded according to the Spinal Adverse Events Severity System, version
2 (SAVES-V2).
Results: Twenty-one patients had a minimum
follow up of 2 years (mean 4.65 years, range: 2.0 – 10.68 years),
including 14 males and 7
females. The mean age at surgery was 8.4 years (median 8, range 0.7 – 14
years). Indications for surgical fusion were C1/2 instability,
secondary
instability after surgery, trauma and other etiologies. Seventeen
patients underwent rigid instrumentation with application of autologous
bone
graft and 4 patients onlay bone graft fusion only. Thirteen patients
underwent postoperative HALO vest application. Final solid bone fusion
was
achieved in 19 patients, including 2 with asymptomatic hardware failure.
Nonunion and worsening junctional kyphosis required revision surgery
in 2 patients. Neurological status remained unchanged postoperatively
and at last follow-up. The surgical complication rate was 14%, the
overall
complication rate 23% respectively.
Conclusion: Variable fusion techniques of the
cervical spine can be safely performed and result in adequate fixation
in children. Autologous
bone grafting is substantially contributing to solid fusion while having
a low morbidity profile.
Keywords: Posterior cervical spine instrumentation; Pediatric; Fusion; Bone graft; Autologous
Abbreviations: BMP: Bone Morphogenetic Proteins; CT: Computer Tomography; FU: Follow Up; MEPs: Motor Evoked Potentials; MRI: Magnet
Resonance Imaging; PSIF: Posterior Spinal Instrumented Fusion; SSEPs: Somatosensory Evoked Potentials
The quality of bone fusion is one of the most critical outcomes
in the surgical management of cervical instability. It highly
contributes to the rate of revision surgeries and overall long-term
outcome [1,2]. Especially in children the surgical management
of cervical instability and achieving solid fusion is technically
challenging due to the age-dependent variation of anatomy and
the lack of pediatric-adapted instrumentation hardware and tools
[3,4].
Importantly, the different subset of etiologies resulting in
instability of the pediatric cervical spine comprise acquired,
but also congenital, syndromic and developmental disorders,
which differ from adult pathologies which are characterized by mostly degenerative and traumatic origins. Accordingly, surgical
techniques transferred from adults to pediatrics required
technical adjustments and flexibility in their application [4]. Given
the growing and immature nature of the pediatric spine additional
amendments are necessary in order to anticipate the variable
anatomy and secondary adverse effects such as adjacent segment
degeneration and reduced future growth, depending on the
levels and length of the construct [5,6]. Different instrumentation
techniques of the pediatric cervical spine have been described,
including non-rigid techniques such as external fixation (HALOvest
immobilization), variable techniques of internal fixation and
onlay bone grafting only [2,7-9].
Supplemental measures of enhancing fusion include the
postoperative application of an external HALO device as well as
autologous bone grafting or the application of bone morphogenic
protein combined with cancellous morselized allograft during
the surgery [10]. Despite their assumed benefit of optimizing
postoperative fusion, both of these techniques remain subject
of a controversial discussion in previous outcome reports with
respect to invasiveness, associated morbidity for autologous bone
grafting, compliance and necessity for the external HALO device,
respectively [11-15]. We describe our experience with posterior
cervical spine fusion techniques in children and re-visit the role of
autologous bone grafting.
We performed a single center, retrospective observational
study including pediatric patients with diagnosed cervical
instability, who underwent a first time posterior cervical
spinal instrumentation, combined anterior and posterior
instrumentation and/or onlay bone graft fusion between January
1, 2008, and December 31, 2019, at the Hospital for Sick Children
Toronto, Canada. Demographic, radiological, and clinical data
were gathered through a retrospective chart review according to
the following inclusion criteria:
a) Age <18 years at time point of surgery
b) Cervical instability (x-ray, MRI, w/wo neurological
deficit).
c) Posterior spinal instrumented fusion (PSIF) or onlay
bone graft fusion.
d) Follow-up (FU) >2 years
Exclusion criteria were a follow-up period of less than 2 years
as well as incomplete clinical and radiographic follow-up. Clinical
characteristics, indications for fusion, neurological examination
findings, and the use of external Halo traction or vest pre- and
postoperatively were reviewed. The primary outcome was defined
as presence of a solid bone fusion at 2 years after surgery on plain
and dynamic x-ray films, whereas the secondary outcomes included
type and number of revision surgeries, surgical complications and
neurological outcome. The radiographic indices for a solid fusion
were:
a) Presence of a solid fusion mass on x-ray posterior to the
fused segments.
b) Absence of motion in dynamic x-rays.
c) Absence of signs for hardware failure (breakage,
dislocation).
d) Absence of halo-sign as indicator for screw loosening.
Approval for the study was obtained from the University of
Toronto Research Ethics Board and the study was conducted in
accordance with ethics guidelines.
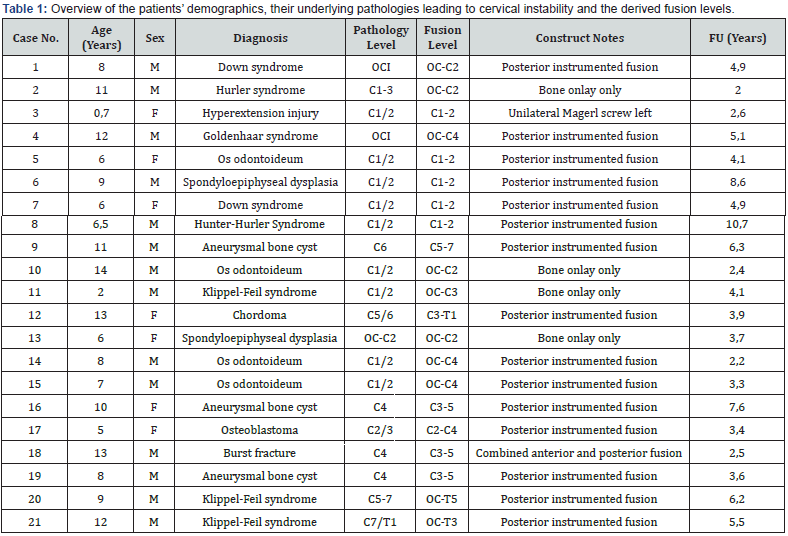
Twenty-one out of 31 patients met the inclusion criteria and
had a minimum follow up of 2 years (mean 4.65 years, range: 2.0-
10.68 years). The remaining 10 patients had not completed the
2-year follow up at the time point of study submission. The sex
distribution was 2:1, with 14 males and 7 females. The mean age
at surgery was 8.4 years (median 8 years, range 0.7-14 years).
Indications for surgical fusion were C1/2 instability (9 patients),
secondary instability after tumor surgery (5 patients), trauma
(2 patients) and other etiologies (5 patients). Importantly, most
of the treated cervical instabilities occurred in a syndromic
context (8 patients) and congenital disorders (2 patients), 48%
respectively. A detailed list of the patients’ demographic data, their
fusion levels and their pathologies are given in (Table 1).
The diagnosis of cervical instability was determined by
assessing a combination of plain and dynamic x-ray studies and
magnetic resonance images demonstrating significantly increased
mobility in one or more of the three planes of movement (flexion–
extension, axial rotation, and lateral bending. Thin-cut computer
tomography (CT) scans with 2D sagittal and coronal as well as
3D reconstructions were obtained pre-operatively for surgical
planning with respect to the optimal fusion and instrumentation
technique. Four patients underwent preoperative HALO traction
in order to obtain a closed reduction in the context of subluxation
or cervicothoracic dissociation.
Two of them underwent additional HALO vest application as
well as 2 other patients with Down syndrome for primary preoperative
stabilization. Sixteen patients were submitted to rigid
posterior instrumentation and one patient combined anterior and
posterior instrumentation, all with intraoperative application of
autologous bone graft. We performed an onlay bone graft fusion
only in 4 patients. The autologous bone graft was predominantly
harvested from the iliac crest (17 patients), followed by the rib (2
patients) and local graft from the spinous processes (2 patients).
All of the surgeries were performed with a rigid head fixation
in the Mayfield clamp and under neuromonitoring including
somatosensory evoked potentials (SSEPs) and motor evoked
potentials (MEPs).
Postoperative HALO vest application was performed in
13 patients, including 8 syndromic patients, 2 patients with a
congenital disorder as well as one trauma patient with a severe
hyperextension injury. The levels of fusion in all of these patients
were located in the upper cervical spine at C1/2 or at the
craniocervical junction, including the occiput as upper fixation
point. All patients, who underwent posterior cervical fusion with
onlay bone graft only were included in this group (Figure 1).
The time period for postoperative HALO vest application ranged
between 2 and 3 months.
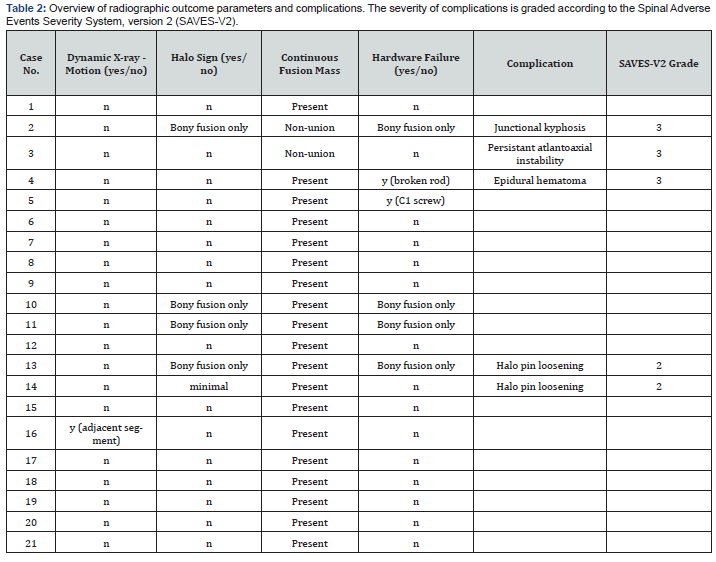
Solid bone fusion was confirmed radiographically via
dynamic x-ray and computer tomography in 19 patients (90%)
at the 2-year follow-up, including 2 patients with asymptomatic
hardware failure. One of them had a rod breakage on one side and
the other one a questionable screw loosening, however a solid
posterior bone fusion mass was present, and no motion observed
in the dynamic x-rays. Nonunion and worsening junctional
kyphosis required revision surgery in 2 patients at 5 and 6 months
postoperative follow up.
One of these patients with Hurler syndrome had a previous
bone onlay only fusion anticipating his small posterior elements,
which did not permit primary instrumentation. He required
augmentation of the autologous bone with additional grafting
from the rib. A nine-month-old female developed a non-union with
persistent atlantoaxial instability, equally requiring augmentation
of the autologous bone graft and extension of her fusion to C3 (see
case illustration, (Figure 2)). The rate of fusion failure in the early
postoperative course was 10%. Radiographic data on the fusion
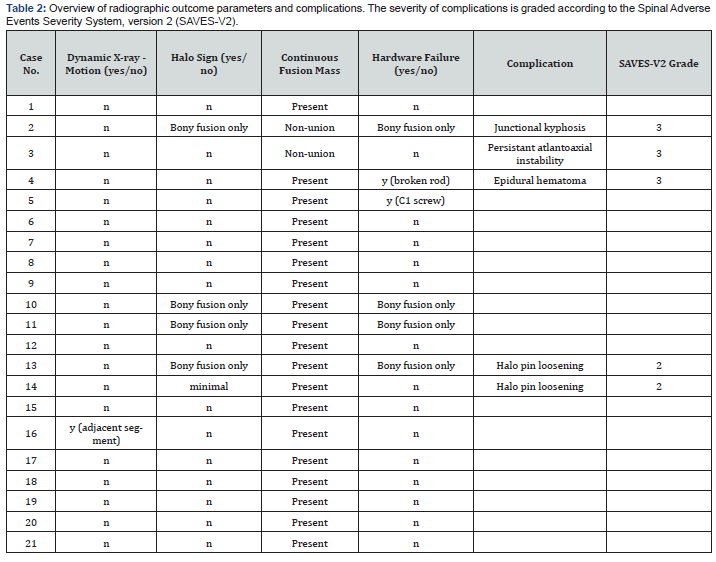
outcomes are shown in (Table 2).
The neurological status of all patients remained unchanged
postoperatively and at the last follow-up visit. There were no
transient neurological deficits observed in the early postoperative
course.
Non-fusion related complications were development of
an epidural hematoma after HALO ring application in one
patient, necessitating emergent surgical decompression. HALO
vest adjustments requiring additional sedation occurred in 2
patients. One patient developed repeat pin site infections due
to the lack of adequate care and required antibiotic treatment.
None of the patients developed a primary surgical site infection
or complications related to the bone graft site. The overall
complication rate was 23%, including the HALO vest adjustments
and complications related to its placement and positioning.
Complications and their grading according to the Spinal Adverse
Events Severity System, version 2 (SAVES-V2) are indicated in
(Table 2) [16].
We have described our experience managing cervical
instability of various etiologies in 21 children, undergoing surgical
fusion with rigid instrumentation or bone onlay grafts only. All
patients underwent autologous bone grafting during the index
procedure and 90% were confirmed with a solid fusion at the
2-year follow up. Two patients required revision surgery due to
non-union and junctional kyphosis, indicating temporary lack of
solid fusion. However, solid fusion could be achieved after revision
surgery with augmentation of the bone graft in both patients.
Multiple studies reported the use of autologous bone
grafting
and its impact on obtaining solid fusion [11,12,17,18]. Posterior
iliac crest autograft is the preferred substrate for bone graft
material, followed by rib graft in youngest children and after
multiple fusion attempts. Despite its excellent structural support
and its benefit on fusion outcome it remains controversially
discussed in regard to morbidity and surgical site complications
[2,19]. Several authors discuss a significant morbidity from the
autograft harvest site, such as donor site pain, increased blood
loss and infection risk, seroma formation, pelvic fracture, and the
risk of peripheral nerve injury.
Moreover, it was experienced as a challenge to harvest and
craft a well-fitting bone block from a small rib or thin iliac crest
in children [1,20,21]. We did not observe any of these morbidities
or complications in our cohort. From a technical perspective we
equally did not face any challenges in harvesting the bone graft,
which might be related to using autograft as a “gold-standard”
during deformity surgeries in our institution. Other authors
confirmed a clear superiority of autologous bone graft compared
to allograft or bone morphogenetic proteins (BMP) and advocate
for its continuous use [22,23].
A recent meta-analysis published by Reintjes et al. [20]
assessed the fusion rates in 604 pediatric patients undergoing
either posterior cervical or occipitocervical instrumented fusion
with additional grafting of autologous bone in 539 and in 65
patients with application of allograft. Higher overall fusion rates
were observed in the autologous compared to the allograft
group (94% vs 80%) [20]. In our study autologous bone graft
was applied to 21 patients, of which 2 demonstrated a shortterm
postoperative fusion failure (10%) resulting in a fusion
rate of 90%. These results are concordant with previous reports
and confirm the benefit of autologous bone grafting with a low
morbidity profile. Importantly, we could demonstrate overall good
fusion results in patients with bone onlay graft only.
The 4 patients were 2, 6, 11 and 14 years old, suggesting that
success of this technique is not necessarily restricted to a specific
age group or younger children. However, randomized controlled
trials are warranted in order to compare the efficiency and
outcomes of rigid instrumentation versus onlay bone graft only.
Another important point of discussion is the pre- and postoperative
use of HALO devices. They were applied in the majority of our
patients, 13 patients (62%) respectively. The reasoning was either
to achieve preoperative reduction or to facilitate postoperative
fusion.
Latter one might be particularly at risk in patients with
cerebral palsy, in syndromic and youngest patients, who might
present with abnormal movements or compromised compliance.
Furthermore, given the softer bone texture there is a higher
complication rate related to implant pull-out in these pediatric
patients. In this context HALO vest application after posterior
cervical fusion has been shown to be beneficial. Moreover, we
do think that fusions performed with onlay bone graft only
mandate postoperative external stabilization in order to facilitate
a solid bone fusion. Despite not having experienced many pin site
infections, except in one patient, we confirm a higher complication
rate in patients with HALO devices.
These are either related to readjustments, requiring most
of the time sedation and complications that occurred during
placement of the device per se. Although HALO devices are related
to a higher complication profile, they outweighed in our patient
cohort with many complex and syndromic patients the risk of
implant pull-out and nonunion. Previous studies reported similar
complications, but also an increased fusion rate in patients with
postoperative HALO vest or Minerva cast application [24,25].
Thus, the indication for HALO devices needs to be adapted to the
underlying pathology, degree of instability, levels of fusion and the
compliance of the patient, outweighing its risks and benefits in a
critical manner.
Limitations of the study are the small number of patients,
especially in the onlay bone graft group as well as the
confounding factor of not having a control group, undergoing rigid
instrumentation without additional application of autologous
bone graft.
In this study, we found that the variable fusion techniques of
the pediatric cervical spine can be safely performed and represent
an effective way to treat cervical instability in various pathologies
and patient ages. The supplemental application of autologous bone
graft increases the quality of fusion while having a low morbidity
profile with respect to the grafting site. The use of postoperative
HALO vest application can be advantageous in syndromic patients
and those, who undergo fusion of the upper cervical spine and the
craniocervical junction in order to enhance the construct stability
and fusion onset. Further studies with larger patient numbers are
required to confirm these findings.
To Know more about Head Neck & Spine Surgery
Click here: https://juniperpublishers.com/index.php