Yoga and Physiotherapy - Juniper Publishers
Abstract
Yoga and mindfulness improve the blood circulation and thereby reduces the causes of hypertension hearth attack or stroke. Complete yoga breathing has the role in oxygenating the blood and therefore assists fresh nutrients to reach all peripheral vessels and capillaries. Yoga helps to prevent various circulatory ailments and illnesses such as high blood pressure, shallow breathing, muscle tension and coronary heart disease. During moderate to intense yoga exercise hearth rate increases and as a result hearth pumps more blood, systolic blood pressure rise and blood volume increases. It provides better circulation and formation of new capillaries. The purpose of this review is to investigate the efficacy of yoga exercise on circulatory system, pulse and hearth rate, systolic and diastolic blood pressure and cardiovascular function. A review of literature was conducted from Pubmed, Research Gate, Medline and Google Scholar.
Keywords: Yoga Asana; Circulatory System; Pulse Rate; Hearth Rate; Systolic And Diastolic Blood Pressure; Cardiovascular Function
Introduction
Yoga is a mind-body technique, which combines set of physical exercises (asana) and techniques (pranayama), relaxation and meditation, and it is practiced in India for thousands of years [1]. Throughout the world, scientists have extensively studied yogasanas and have concluded that yoga increases longevity of life and has therapeutic and rehabilitative effects [2]. Namely, it has been reported that yoga exercise has an positive impact on serum lipid profile [3], heart rate variability [4], decrease in blood pressure, and even regression of atherosclerosis when combined with dietary and other lifestyle modifications [5]. Also, many studies have shown that yoga can be a very effective as a non-invasive way of reducing high blood pressure [6]. A healthy circulatory system is important for a healthy living. Yoga helps to prevent various circulatory ailments and illnesses such as high blood pressure, shallow breathing, muscle tension and coronary heart disease [7].
The blood circulatory system (cardiovascular system) delivers nutrients and oxygen to all cells in the body. The circulatory system includes the heart, blood vessels and the blood. It transports the nutrients and oxygen to the tissues and removes carbon dioxide and other waste products of metabolism from the tissues. For this purpose the blood is continuously circulated in the body by rhythmic pumping action of the heart and through a complex network of the blood vessels. The blood acts as a vehicle that carries the products of digestion from the alimentary canal and the oxygen from the lungs to the tissues. While returning to the heart, the blood brings the toxic substances or the waste products back to the heart. The kidneys, lungs and the skin eliminate these substances when the blood circulates through them. The blood, thus, communicates with all the systems and organs, regulates the water level and the temperature of the body [7,8].
Yoga’s impact on cardiovascular health is multi-dimensional. While not all yoga movements raise the heart rate to suggested aerobic levels, yoga has a positive impact on how efficiently blood moves. An asana practice can increase blood circulation and decrease levels of cortisol, a stress hormone, in the body [2]. In fact, a study conducted by Kaviraja Udupa et al.in 2003 on 24 healthy young subjects showed significant reduction in basal heart rate and systolic and diastolic blood pressure following 3 months of yoga training [9]. The lower levels of stress enjoyed by yogis has a significant impact on creating healthier blood pressure. Yoga has also been shown to reduce cholesterol levels, thus reducing the interference of blood flow. Low-impact, meditative poses can also reduce potentially artery-clogging stress hormones. Examples of such poses are like Sukhasana (Easy Pose) or Child’s Pose (Balasana). Several poses and postures in Yoga have an different effect on circulatoy system [10].
In standing poses, the lateral wall of the heart is exercised is such a manner that it becomes flexible and toned up. Standing poses helps in improving the flow of blood along the walls of the heart thus preventing heart diseases. Inverted postures in Yoga helps to prevent muscles and cell tissue degeneration due to the benefits of that the inverted poses have on the body. Inverted postures help in effective blood circulation to the brain. Moreover the lymph system in the legs and the muscles are properly rested in exercises involving inverted poses. On the other hand. blood pressure in horizontal poses is effective brought under control as the performance of horizontal postures helps in resting and rejuvenating the heart and lungs. In bending postures the body experiences improved blood supply to the cardiac muscles. This leads to a toning up of the myocardium or the heart muscles [7]. Yoga exercise benefits the entire circulatory system, beginning with the production of blood, which takes place in the marrow of the long bones in the thighs. It has been showed that daily yoga stretching exercises are helping to rejuvenate the blood. Yoga exercises stretch the body’s major blood vessels, keeping them free-flowing and elastic [11]. Furthermore, improved circulation will improve the alertness, memory, and mood. Vital organs are by yoga receiving a steady supply of the nutrients they need for optimal functioning [2]. However, studies on the effect of yoga training on circulatory system are limited. In view of this, the present study was planned with an objective to determine the effect of yoga training on healthy circulatory system in the body.
Methods
Authors independently conducted literature searches to identify studies on the effect of yoga exercise on circulatory system. The databases searched included Pubmed, Research Gate, Medline and Google Scholar. The following search terms were used: yoga asana, circulatory system, systolic and diastolic blood pressure, cardiovascular function.
Inclusion criteria were:
a. randomized control trial (RCT); the study contained at least two groups where there are two different intervention groups or a meditation group and a control.
b. studies that were published in English.
c. Studies with 30 participants and more.
d. Studies with participants above the age of 35 years and less than 75 years old.
e. Studies are excluded if they:
I. They were not written in English.
II. Non-RCT study.
III. Studies with less than 30 participants and with adolescents.
A total of 118 articles were originally found through the database searches. Of those, 102 were excluded based on review of the title and abstract. The remaining 16 articles were carefully evaluated against the inclusion and exclusion criteria through detailed readings. Ten of 16 articles were excluded, leaving 6 to be included in the final analysis.
Result
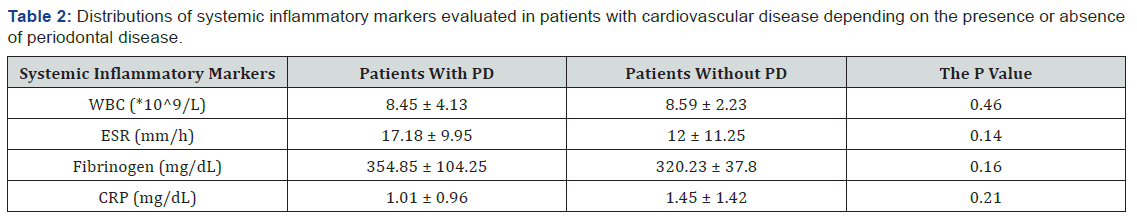
The cardiovascular diseases are much on a rise ever since the past few decades in developing countries. In our study we have analyzed the effect of yoga on circulatory system and cardiovascular function in normal adult person above the age of 40 years. Five studies examined correlation between yoga exercise and decrease in heart rate and blood pressure. Krishna et al. in their study found a significant decrease in heart rate, blood pressure and rate pressure product in yoga group compared to control group. Out of 130 heart failure patients recruited for the study, 65 patients were randomly selected to receive 12 week yoga therapy along with standard medical therapy (yoga group). Other patients have received only standard medical therapy (control group). The authors came to conclusion that twelve-week yoga therapy can significantly improve the parasympathetic activity and decrease the sympathetic activity in heart failure patients [12] Singh has in his study found that yoga practice can be used as an intervention in ageing persons to reduce the morbidity and mortality from heart circulatory diseases. This study included 50 healthy men above the age of 40 years which are performing yoga regularly.
The heart circulatory status was assessed by recording the blood pressure and pulse rate, before and after 6 months of regular yogic practice. Results have shown that mean resting systolic blood pressure (mm Hg) was lowered to a highly significant level of 120.05±3.40. The mean resting diastolic blood pressure (mm Hg) before yoga was 83.6±6.10 and reduced significantly (p<0.001) to 76.4±6.35. Stress was measured with the Stress Assessment Questionnaire, and blood pressure information was taken from medical records. The study found a significant difference between the stress scores of the experimental and control group at the conclusion of the study even though there was no baseline difference from the second to the eighth week.
Bharshankar et al. [6] have examined examine the effect of yoga on cardiovascular function in 100 subjects above 40 years of age both sexes. Pulse rate, systolic and diastolic blood pressure and Valsalva ratio were studied in 50 control subjects (not doing any type of physical exercise) and 50 study subjects who had been practicing yoga for 5 years. The mean value of pulse rate was lower in study than control group statistically to the significant extent (p<0.001). The statistical difference in the mean systolic and diastolic blood presure in between study and control group was significant (p<0.01, p<0.001 respectively) [13].
In another study by Harinath et al. the aim was to evaluate effects of Hatha yoga and Omkar meditation on cardiorespiratory performance, psychologic profile, and melatonin secretion. Hypertensive patients were randomly divided in two groups. Group 1 was conducted of 15 subjects served as control and performed body flexibility exercises for 40 minutes and slow running for 20 minutes during morning hours and played sports for 60 minutes during evening hours daily for 3 months and group 2 subjects, 15 of them, practiced selected yogic asanas (postures) for 45 minutes and pranayama. The benefit of yoga practice in terms of blood pressure reduction was modest, but statistically significant; in contrast the control group had no significant change in blood pressure. Furthermore, the results showed that yoga exercise for 3 months can result in an improvement in cardiorespiratory performance and psychologic profile.
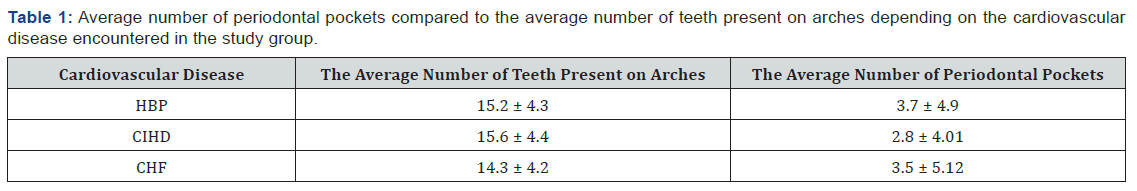
The systolic blood pressure, diastolic blood pressure and mean arterial pressure did not show any significant correlation with plasma melatonin [14]. Patel and North conducted a randomized trial of yoga practice in 34 subjects who were less than 75 years old and had a diastolic blood pressure of 110mm Hg or higher. Patients were randomized to yoga practice or to general relaxation exercises, and all were evaluated every 2 weeks for 3 months. Patients in both groups had a significant drop in systolic and diastolic blood pressures (from 168/100 to 141/84 mm. Hg in the treated group and from 169/101 to 160/96 mm Hg in the control group). The difference was highly significant. The control group was then trained in yoga relaxation, and their blood pressure fell to that of the other group (now used as controls). Murugesan et al. [15] in their study have evaluated the effect of yogic practices on the management of hypertension. The study included 33 hypertensive patients, age 35 and 65 years. The subjects were randomly assigned into three groups. The group I underwent selected yoga practices, group II received medical treatment by the physician and the control group (group III) did not participate in any of the treatment stimuli. Patients in the yoga group performed breathing exercises, Asanas as well as meditation for 1 hour every day for 11 weeks. There was a significant decrease in systolic blood pressure, heart rate and body weight and these changes were greater in subjects who practiced yoga than in the subjects who received medications alone [16]. (Table 1) is the description of included studies.
It is obvious that the regular practice of yoga, particularly when combined with other life-style modifications, can induce biochemical alterations that have a salutary effect of cardiac hemodynamics, blood lipids, blood pressure and cardiovascular function [17].
Discussion
Yoga has three elements- exercise, brathing and meditation. Experts believe that the yoga asanas are the best way to keep it fit naturally. The heart is an involuntary muscle that contracts and relaxes around 70 times a minute within a healthy individual. With asanas, the expansion and contraction of the heart is made even faster and thorough. However, overdoing yoga asanas is never preferred for it may cause damage to the heart. Padmasana considerably improves blood circulation. In this case, the pelvic region receives larger blood supply from the bifurcations of the abdominal aorta. Each drop of blood travels twice, once through the pulmonary circulation and then through the systemic circulation in the body. During the systemic circulation, pure (oxygenated) blood is pumped out forcefully from the left ventricle into the aorta. It is then carried to parts of the body [7]. During yoga session the massaging effect on the internal organs improve blood circulation. During moderate to intense yoga exercise hearth rate increases and as a result hearth pumps more blood, systolic blood pressure rise and blood volume increases. It provides better circulation and formation of new capillaries [8].
Many research studies have documented the usefulness of yoga in the treatment of various lifestyle related diseases, especially heart circulatory disease. Singh has in his study concluded that yoga has significant and healthy impact on our life style [6]. Many studies show that yoga can be a very effective and non-invasive way of reducing high blood pressure. It is particularly effective in reducing the diastolic number – which is the most important. It is suggested that people with high blood pressure should only practice certain asanas (postures), whilst acknowledging that there are other asanas that are not suitable for them. The yogic practices of meditation and pranayama (breathing exercises) are also particularly beneficial for people who suffer from high blood pressure [18].
Additionaly, environmental conditions and variety of behavioural factors such as stress, anxiety, affective and attitudinal dispositions of the individual influence the cardiovascular responses. Yogic exercise involves physical, mental and spiritual task in a comprehensive manner. It brings about the behavioural changes. Yoga in long duration affects hypothalamus and brings about decrease in the systolic and diastolic blood pressure through its influence on vasomotor centre, which leads to reduction in sympathetic tone and peripheral resistance [7]. Bharshankar and associets came to conclusion that the correlation of age with blood pressure, both systolic and diastolic is stronger in the control group than in the study group. This suggests that rise in blood pressure is not an inevitable consequence of increase in age, but is a result of the aging process which may be slower in practitioners of yoga. Also, cardiovascular parameters alters with age but these alterations are slower in persons aging with yoga [13].
Furtermore, mechanisms by which yoga might may influence hearth rate, blood pressure and heart rate variability are stil speculative. In addition to hemodynamic derangements, an increased neuro-hormonal activation through the sympathetic nervous system and the renin-angiotensin system has been implicated in the progression of heart failure [19]. Murlidhara & Ranganathan reported an improvement in cardiac recovery index after 10 weeks of yoga training in 50 young subjects [20]. A study carried out by Ray et al on the effect of yoga exercises on physical and mental health of 54 young fellowship course trainees showed significant reduction in hearth rate and systolic and diastolic blood pressure after 5 months of yoga training [21]. Tulpule and Tulpule also considered yoga as a method of relaxation after myocardial infarction [22].
Results of many studies have shown that most of the yoga asanas like Sarvangasana, Viparita karni, Hahsana, Mayurasana, few pranayamas like Ujjayi and Bhastrika Pranayama as well as uddiyan, nauli, Jalandhar bandha specially influence the blood circulation. But, the ost important thing is to learn them from an expert in order to practice them safely, without taxing the circulatory system. When the body and mind are properly relaxed, mental peace is achieved and the muscle tone is reduced. The blood vessels are also relaxed which are otherwise constricted due to tension. The heart rate is reduced and blood pressure comes to the normal level.
Further, it is through veins that the impure blood is brought back and there are such troubles as vericose veins, which cause obstructions in blood circulation. However, practising yoga asanas, the body is placed in upside-down position which enables veins to drain themselves into the heart without any effort. Finally, asanas decrease the sympathetic tone, rate pressure product and double product (DoP), and improve cardiovascular endurance and anaerobic threshold [2].
Although yoga has been associated with serious adverse events in single case reports, population-based surveys as well as clinical trials indicate that yoga is a relatively safe intervention and there is no associations with more adverse events than other forms of physical activity. Yoga can thus be considered a safe and effective intervention for managing hypertension [17].
Conclusion
A healthy circulatory system is important for a healthy living. Yoga exercise helps to prevent various circulatory ailments and illnesses such as high blood pressure, shallow breathing, muscle tension and coronary heart disease. Our findings suggest that specific poses of Yoga directly benefit and enhance the circulation of blood and body fluids throughout the body. The different organs of the body are also positively impacted due to the effective flow circulation to the various parts.
To Know more about Yoga and Physiotherapy
Click here: https://juniperpublishers.com/index.php