Neurology & Neurosurgery - Juniper Publishers
Abstract
Stiff person syndrome (SPS) is a rare neurological disorder characterized by stiffness and spasm of the truncal muscles and subsequent postural deformities. In this report, we present a case of a woman in her early 60s who presented to us with muscle stiffness, back pain, and frequent falls. On examination, she was found to have increased muscle tone and mild tremors. Given her age and presentation, a provisional diagnosis of Atypical Parkinson’s was made. Patient was treated with Diazepam. Because of presence of autoimmune co-morbid conditions, anti-glutamic acid decarboxylase (GAD) antibodies were tested, which were positive, and thus, diagnosis of SPS was made. Treatment with Diazepam was continued, and her symptoms significantly improved. Even though SPS is a rare disorder, our case report highlights the need to keep it in differential diagnoses when an elderly patient presents with stiffness and postural instability, as treatment for SPS and atypical Parkinson’s vary considerably.
Keywords: Stiff person syndrome; Atypical Parkinson’s; Anti-GAD antibodies; Rare disorder
Abbreviations: SPS: Stiff Person Syndrome; PD: Parkinson’s Disease; GAD: Glutamic Acid Decarboxylase
Introduction
Stiff person syndrome is a progressive neurological disease even with treatment and results in significant disability in patients affected [1]. In this case report, we will go over our patient’s presentation, the variants of SPS and the presentation of these variants. We will also discuss Atypical Parkinson’s disease and why this diagnosis was considered in our patient.
The main pathogenesis of SPS is thought to be blockade of glutamic acid decarboxylase (GAD) enzyme which is responsible for maintaining inhibitory pathways in the central nervous system. GAD blockade results in reduced levels of gamma butyric acid (GABA) producing loss of neural inhibition. GAD blockade mainly results from anti-GAD antibodies that are associated with multiple autoimmune disorders, the most commonly associated disease being type 1 diabetes mellitus [2].
There are several variants of the disease [3]. The classic variant is associated with other autoimmune disorders while the partial SPS is characterized by stiffness limited to only to one limb. Progressive encephalomyelitis with rigidity and myoclonus is another uncommon variant of the disease characterized by transient oculomotor disturbance. Another rare variant of this disease is the paraneoplastic SPS which is suspected in patients who are anti-GAD negative. These patients have antiamphiphysin antibodies and have associated underlying malignancy of the breast and lung.
Classic SPS is the most common variant of the disease and is characterised by the presence of anti-GAD antibodies and presence of autoimmune diseases. The disease presents with muscle stiffness involving the axial group of muscles, lumbar group, and the proximal limb muscles. The disease is progressive and leads to deformities. As the stiffness and rigidity in the axial muscle group progresses, patients also develop a wide based gait and tend to have frequent falls, thus predisposing them to fractures.
Atypical Parkinson’s on the other hand, are a group of neurodegenerative disorders which have features resembling Parkinson’s disease (PD) with additional features that differentiate them from PD. These include Dementia with Lewy bodies characterized by the presence of visual hallucinations and REM sleep behaviour disorder, Multi system atrophy that presents with postural instability and cerebellar findings like gait ataxia. Progressive supranuclear palsy is another subtype characterized by vertical gaze palsy, akinesia, and progressive aphasia. The last type, called corticobasilar degeneration, is relatively rare and presents with myoclonus and dystonia [4].
A common denominator among SPS and Atypical PD is the presence of rigidity and gait instability producing frequent falls. Due to the similar features in both diseases, diagnosing them clinically can be challenging, particularly in older patients. Not all individuals with Atypical Parkinson’s Disease will exhibit resting tremors, or bradykinesia during their initial presentation; some may only display muscle rigidity and postural instability.
Case Report
A 60-years-old female presented with complaints of backache and stiffness of 4 months duration which was gradual in onset and progressive in nature. She also complained of worsening of stiffness and tightness in her back since the last 2 months and also gave history of 5 episodes of falls. She also developed difficulty in getting up from squatting position. Her past medical history was significant for diabetes mellitus and hypothyroidism for which she was on regular medications. On examination, her vitals were stable. Neurological examination findings revealed increased muscle tone in all four limbs and mild tremors of the hands were noted. Deep tendon reflexes were exaggerated. Cerebellar examination did not reveal any findings. In view of progressive muscular rigidity, tremors and postural instability in an elderly patient, a provisional diagnosis of Atypical Parkinson’s was made while keeping Stiff person syndrome in the differential because of presence of autoimmune conditions diabetes mellitus and hypothyroidism. Magnetic resonance imaging (MRI) of the brain and spine were normal. A nerve conduction study was done which was normal and electromyography was inconclusive.
Serum panel to detect auto antibodies was sent to the lab. The reports came back positive for anti-GAD antibodies and thus the conclusive diagnosis of SPS was established.
During her stay in the hospital, patient was treated with tablet Diazepam 10mg three times daily, which alleviated her symptoms. Her blood sugars were controlled, and thyroid function tests were also done, which were normal. Her symptoms significantly improved following treatment with diazepam, and she was discharged in stable condition. She will be regularly followed up on out-patient basis.
A summary of her lab reports can be found in Table 1.
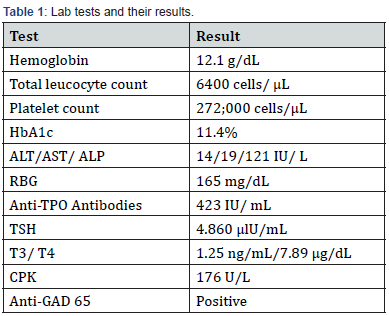
HbA1c : Glycated Haemoglobin; ALT : Alanine Transaminase; AST : Aspartate Transaminase; ALP : Alkaline Phosphatase; RBG: Random Blood Glucose; Anti-TPO Antibodies: Anti-Thyroid Peroxidase Antibodies; TSH: Thyroid Stimulating Hormone; T3/T4: Triiodothyronine/ Thyroxine; CPK: Creatinine Phosphokinase; Anti: GAD Antibodies: Anti-Glutamic Acid Decarboxylase Autoantibodies.
Discussion
The prevalence of Stiff Person Syndrome is only 1 – 2 people per million. Though the pathophysiology of the disease is unclear, neurologists find autoimmunity to be the main culprit, as majority of the cases are associated with anti-GAD positive antibodies. While their presence supports the diagnosis, their absence does not rule out the disease. The disease mainly affects people in their 2nd to 5th decade of life and affects women more than men [5].
The clinical course is progressive stiffness slowly leading to deformities and functional impairment. Intellect and memory are spared. There is no confirmatory test, although anti-GAD antibody test is widely accepted as the diagnostic test. Imaging is noncontributory, neurological testing may reveal continuous firing of action potential. Treatment is usually symptomatic and managing any co-morbid conditions. Death can result from diaphragmatic spasm [6].
Even though the disease is rare, because of its similarity in presentation with that of Atypical Parkinson’s, this differential must be kept in mind, especially in elderly patients.
Hence in elderly patients presenting with gait instability, frequent falls and muscle rigidity, physicians need to consider both SPS and atypical PD and ruling out one of them based on the past medical history and lab findings.
Conclusion
Stiff person syndrome being a rare disorder can easily be missed. It’s prognosis is guarded, and thus early recognition of the disease and initiation of treatment can slow down the functional decline in these patients. As the diseases progresses, patients lose the ability to ambulate and require walking assistance device [7]. They may also require assistance for activities of daily living, and this can have a psychological effect on these patients. Providing psychological counselling is equally crucial to ensure the wellbeing of individuals, a fact that might be disregarded by physicians primarily focused on treating the physical aspect of the disease.
To Know more about Open Access Journal of Neurology & Neurosurgery
Click here: https://juniperpublishers.com/oajnn/index.php
To Know more about our Juniper Publishers
Click here: https://juniperpublishers.com/index.php




No comments:
Post a Comment