Orthopedics & Rheumatology - Juniper Publishers
Summary
Introduction: Palmer and Pellegrini-Stieda disease are rare complications of traumatic rupture of the medial collateral ligament of the knee with a different behavior.
Objective: To assess the pathophysiology, clinical, radiological, arthroscopic picture, and treatment of two late complications of traumatic injury to the internal collateral ligament of the knee.
Method: The search and analysis of the information was carried out in the period from January 1 to May 31, 2023, in the PubMed, Hinari, SciELO and Medline databases using the EndNote search manager and reference manager, using Keywords: rupture, internal collateral ligament, disease, Palmer, Pellegrini-Stieda. A total of 38 articles were obtained, of which 18 from the last five years were selected for discussion.
Development: Palmer and Pellegrini-Stieda disease are late complications resulting from traumatic rupture of the internal collateral ligament but with a different behaviour, the first with intra-articular manifestations with repercussions on the functionality of the joint simulating a rupture of the internal meniscus and the second with extra-articular manifestations with ossification of the thickness of the internal collateral ligament and notable impairment of knee function.
Conclusion: Internal collateral ligament rupture, undiagnosed or insufficiently treated, can result in Palmer’s or Pellegrini-Stieda’s disease as a late complication, the treatment of which is cumbersome, hence the importance of its correct diagnosis and treatment.
Keywords: Rupture; Internal collateral ligament; Disease; Palmer; Pellegrini-Stieda
Introduction
Internal collateral ligament (LCI) injury is a common trauma in young people, especially because of both recreational and high-performance sports in contact sports such as soccer in its different variants (Figure 1) as well as activities work, it is considered exceptional in children and older adults [1,2]. According to Busto-Villarreal [3] quoting Márquez [4] in a study of 500 people with knee ligament injuries, 29% corresponded to LCI ruptures and between 13-18% combined injuries of the LCI and ACL due to what the LCI is involved between 42-47% of all ligament injuries of the knee.
The diagnosis of these lesions is basically clinical and is achieved with exhaustive questioning and a physical examination consisting of the valgus stress test or Böhler maneuver [5,6]. This maneuver can be done radiologically by subjecting the knee to stress by performing an Rx in anteroposterior (AP) view [7,8]. Other complementary tests that can be performed for the diagnosis of these lesions are Ultrasound and Nuclear Magnetic Resonance (NMR), the latter limited by not existing in all hospitals and its high cost. The treatment of traumatic injuries of the LCI is basically conservative with immobilization with an inguinopedic cast for 3-4 weeks and then starting an energetic rehabilitation program [3]. Some authors undertake ligament repair in patients with high demand on their knee using primary repair techniques and even plasties [3,7].
If the lesion is not diagnosed or an incomplete treatment is carried out, two late complications could occur: Palmer’s disease (PD) and Pellegrini-Stieda disease (PD-S), so the objective of this article is to assess these two late complications. consequence of a traumatic injury of the LCI of the knee to better understand its pathophysiology, clinical, radiological, arthroscopic picture as well as the best treatment to carry out for its solution.
Method
The search and analysis of the information was carried out in a period of five months (from January 1 to May 31, 2023) and the following words were used: Rupture, internal collateral ligament, disease, Palmer, Pellegrini-Stieda. Based on the information obtained, a bibliographic review of a total of 38 articles published in the PubMed [https://pubmed.ncbi.nlm.nih.gov/], Hinari [https://www.who .int/hinari/es/], SciELO [https://scielo.org/ es/] and Medline [https://medlineplus.gov/spanish/] through the EndNote search manager and reference manager, of which They selected 18, from the last five years, to carry out the discussion. The words selected for the search were taken from MeSH (Medical Subject Headings).
Development
Palmer’s disease
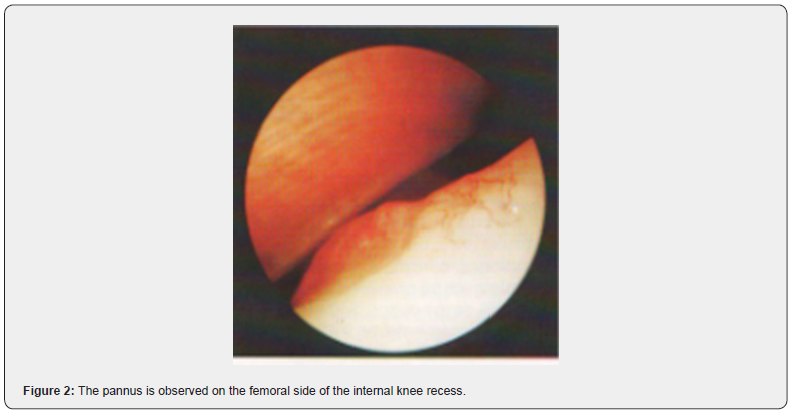
Described by the Swedish doctor Ivar Palmer in 1936, cited by Eriksson [9], it is a rare and unknown pathology that originates from traumatic rupture of the LCI in the thickness of the ligament towards the femoral insertion and whose subsequent healing with consequent retraction of the ligament originates in the internal recess of the knee towards the internal femoral condyle in arthroscopic visualization a mamelonating lesion with bulge, synovial proliferation and pannus formation (Figure 2) that also causes pain on the internal side of the knee on the joint spacing, limitation to the extension of the last few degrees and references to episodes of blockages simulating a meniscal lesion [10,11].
It generally occurs in young male patients because of practicing sports, whether recreational or high performance, between one and two years after the occurrence of a traumatic event in the knee, hence the importance of exhaustive questioning of the patient [10]. Patients complain of pain on the inside of the knee and of suspected blockages, occasionally they may present joint effusion. The physical examination reveals a limitation to the extension of the knee compared to the contralateral one. It simulates a meniscus lesion with positive Böhler, Mc Murray and Appley maneuvers [5,10]. But there is a maneuver discovered and practiced by Palmer, also known as the Wobble Test’s, brought to the present day by Carnes and Malanga [5,6] and cited by Morales et al. [10].
Palmer’s maneuver or Wobble Test’s
It consists of placing the patient in a supine position and the hip flexed between 30-45°, the performer of the maneuver standing next to the patient holds the knee with both hands and holds the leg between the thorax and the examiner’s arm, place the balls of the thumbs on the medial and lateral joint lines to gain space and sensation, then alternate valgus and varus repeatedly starting with the knee at 30° and slowly extending it. If the procedure is painful or there is apprehension, the maneuver is positive.
Mistakes that can be made.
Move the knee from front to back.
Move very fast.
Applying too much valgus and varus to the knee.
Don’t make it repetitive.
Do not make it comparative with the contralateral knee.
Meaning of the maneuver
If the ligament is lax, it is a premonitory of hyperlaxity or ligament rupture (acute phase), if there is no laxity and it is limited in relation to the contralateral knee, it is synonymous with anterior rupture, healing, and retraction of the ligament (chronic phase).
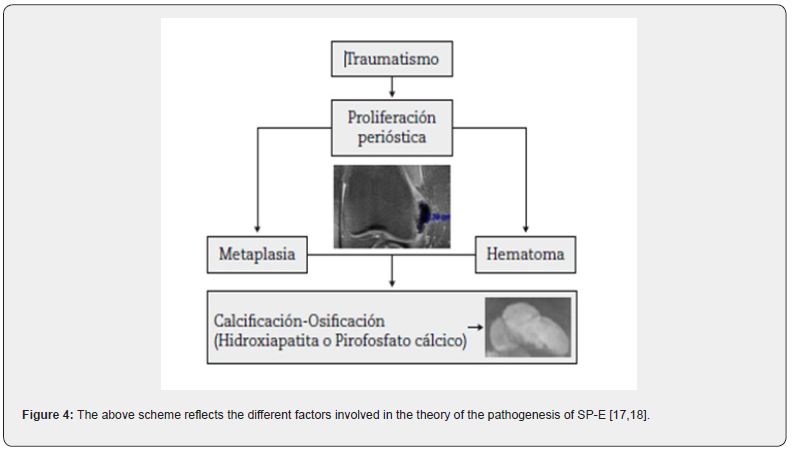
Pathophysiology
The superficial internal collateral ligament has abundant irrigation (Figure 4). When it is injured, the healing of this ligament complies with the classic model that consists of hemorrhage, inflammation, repair and remodeling. The rupture must occur in the thickness of the ligament, since if it occurs in After insertion, bleeding can be accompanied by osteogenic cells and create conditions for ossification [12-14]. Although the phenomenon occurs in the thickness of the LCI, translation is intra-articular, forming a small promontory in the internal recess of the internal face of the femoral condyle. internal surrounded by pannus and that is the cause of the supposed “blockages”.
Diagnosis
It is achieved with an exhaustive questioning, detailed physical examination where, in addition to practicing the classic knee exploration maneuvers, we must practice the Palmer or Wobble Test’s maneuver, many times the finding is accidental when performing a routine arthroscopy due to the suspicion of an injury of the internal meniscus.
Treatment
The treatment is arthroscopic and consists of the ablation of the pannus and the promontory that causes the blockages with an energetic post-surgical rehabilitation.
Pellegrini-Stieda disease
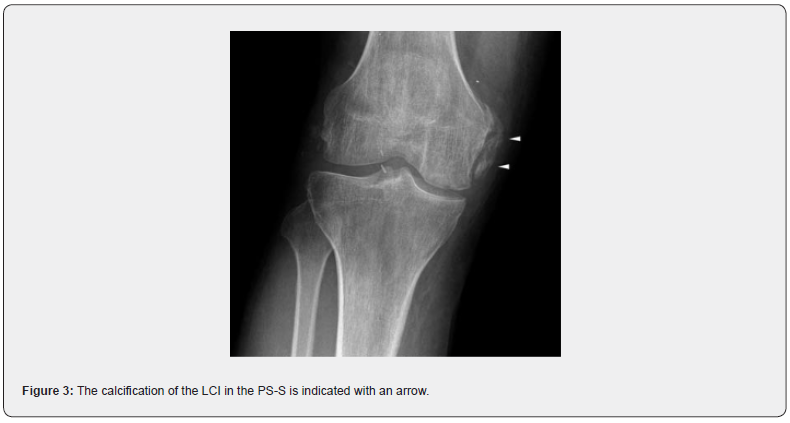
Also known as Pellegrini-Stieda Syndrome, described in 1905 by the former and 1908 by the latter [15]. It consists of calcification of the LCI (Figure 3) and occurs because of the rupture of this ligament as a result of a trauma in the femoral insertion that does not was misdiagnosed or undertreated. Mostly young patients, men who are active at work or in sports, who report a history of knee trauma and complain of pain on the inner face and present limitation mainly to knee flexion [15]. The physical examination revealed pain on the inner side of the knee with greater sensitivity in the path of the LCI and pain with some limitation to flexion. Böhler and Palmer maneuver are positive.
Diagnosis
The diagnosis is basically made by simple X-ray of the AP and lateral knee, observing the calcification of the LCI. In 2006 Mendes et al. [16] cited by Forriol [17] published a classification of the radiological characteristics of LCI calcifications characterized by:
Grade I: Peak-shaped with inferior orientation and union to the femur.
Grade II: Drop-shaped with inferior orientation and parallel to the femur.
Grade III Elongated with superior orientation.
•Grade IV: With upper and lower orientation attached to the femur.
Ultrasound and MRI are also used, the latter being more expensive and not within the reach of many. pathophysiology.
Treatment
Once the diagnosis has been established, treatment is basically conservative, aimed at eliminating calcification, using rest, NSAIDs and physiotherapy in its different variants [17,18]. Other authors recommend needle aspiration under echosonographic vision and infiltration on steroids. Surgical treatment consisting of excision of calcifications is also recommended, with the drawback that they can be reproduced [18].
Conclusion
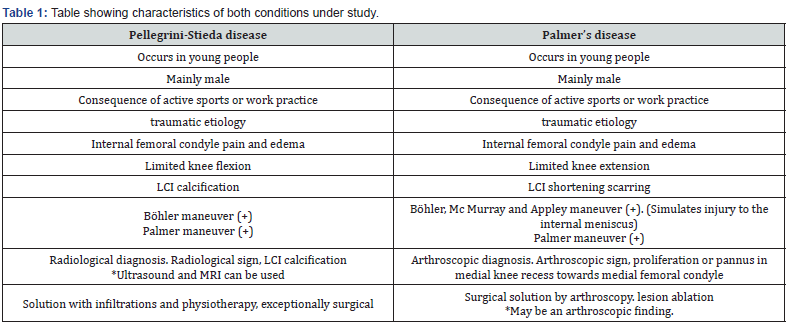
Finally, and as a conclusion, we condense in the following synoptic table the most significant characteristics of both conditions under study (Table 1).
To Know more about Orthopedics and Rheumatology
Click here: https://juniperpublishers.com/oroaj/index.php
Click here: https://juniperpublishers.com/index.php




