Otolaryngology - Juniper Publishers
Abstract
Bilateral Sudden Sensorineural Hearing Loss (BSSNHL) is a rather rare and intricate condition marked by a sudden decline in hearing ability in both ears within a 72-hour timeframe. This review delves into the uniqueness of BSSNHL in comparison to unilateral cases, exploring its various causes, diagnostic criteria, management approaches, and the influence of COVID-19 on its manifestation. The review relies on a thorough examination of existing literature, emphasizing the scarcity of specific research on BSSNHL and underscoring its challenging prognosis despite diverse treatment options. Notably, the discussion touches upon potential triggers such as idiopathic, infectious, autoimmune, vascular, and membrane rupture, shedding light on the underlying mechanisms. It further elaborates on diagnostic criteria for BSSNHL, categorizing cases based on the onset duration. The review critically assesses management strategies, ranging from steroids to hyperbaric oxygen therapy, with an emphasis on the unpredictable nature of therapeutic outcomes. The intriguing link between BSSNHL and COVID-19 is explored through a case report, narrating the experience of an 18-year-old patient with bilateral hearing loss, anosmia, and loss of taste, suggesting the virus's involvement in auditory complications. In conclusion, the review highlights the rarity of BSSNHL, outlines the challenges in prognosis, and advocates for dedicated research to enhance comprehension and advance clinical outcomes for those affected.
Keywords: Bilateral sudden sensorineural hearing loss; Unilateral hearing loss; COVID-19; Viral infections; Hyperbaric oxygen therapy
Abbreviations: BSSNHL: Bilateral Sudden Sensorineural Hearing Loss; QoL: Quality of Life; RTI: Respiratory Tract Infection; MS: Multiple Sclerosis; SSNHL: Sudden Sensorineural Hearing Loss; RCD: Red Cell Distribution; AICA: Anterior Inferior Cerebellar Artery; HBO: Hyperbaric Oxygen
Introduction
Sudden Sensorineural Hearing Loss is defined as the sudden decline in hearing ability by over 30dB1, typically across three successive frequencies during pure-tone audiometry, within a period of 72 hours. Among the cases of sudden hearing loss, 98-99% are unilateral, while only 1-2% are bilateral [1]. Therefore, Bilateral Sudden Sensorineural Hearing Loss (BSSNHL) is an extremely rare and complicated disease. As for its onset and presentation, SSNHL has an acute onset and vague presentation, substantially limiting the quality of life (QoL) due to its acute and ambiguous nature, affecting communication ability significantly [2].
Clinically, it was first described in the early 1940s as at least a 30dB of hearing loss over three successive frequencies during pure-tone audiometry in fewer than three days [3]. The reported incidence is 5 to 20 per 100,00 annually [4]. Out of all reported cases, the predominant form is unilateral (95%), commonly idiopathic [5]. Only fewer than 4.9% of cases represent the bilateral form [6]. Due to its low incidence, literature provides limited data on the bilateral form. However, available research suggests that, unlike unilateral SSNHL, the bilateral form usually manifests as a consequence of some severe systemic condition, typically absent in the case of the former [6,7].
Literature Search
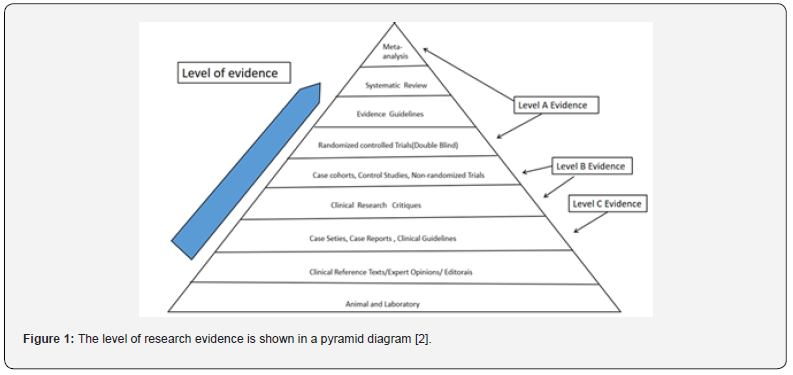
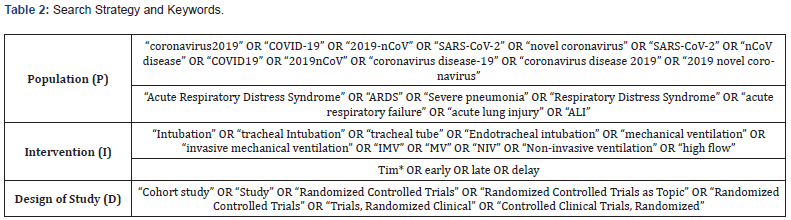
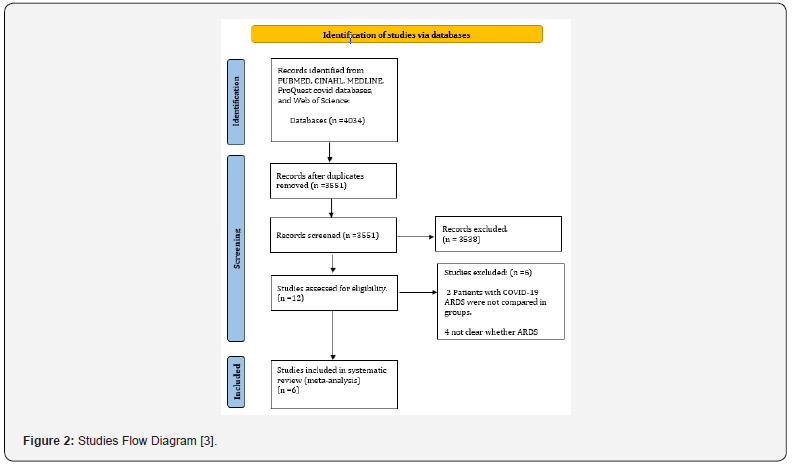
This narrative review on Bilateral Sudden Sensorineural Hearing Loss (BSSNHL) employs a non-systematic approach, summarizing relevant literature identified through keywords in reputable journals. Inclusive of various study types, we focus on English-language, peer-reviewed research from databases like PubMed, MEDLINE, Scopus, and Google Scholar, covering material from database inception to the present. Exclusions include non-English publications, non-peer-reviewed articles, and studies with unclear methodologies. Manual searches complement database findings and data extraction centers on key variables. The synthesis aims for a cohesive narrative, providing insights into BSSNHL's current understanding and identifying potential research gaps.
Causes of BSSNHL
Idiopathic
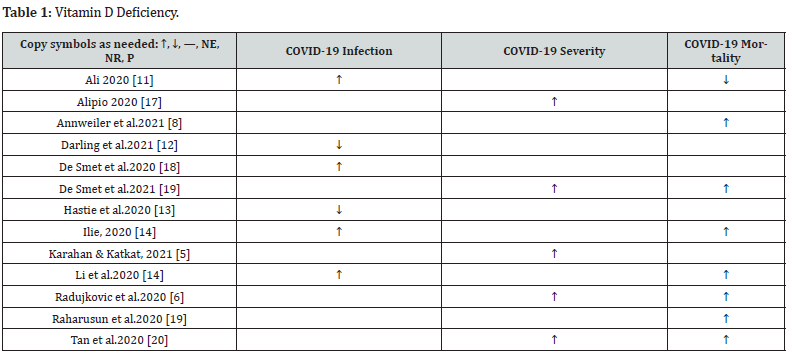
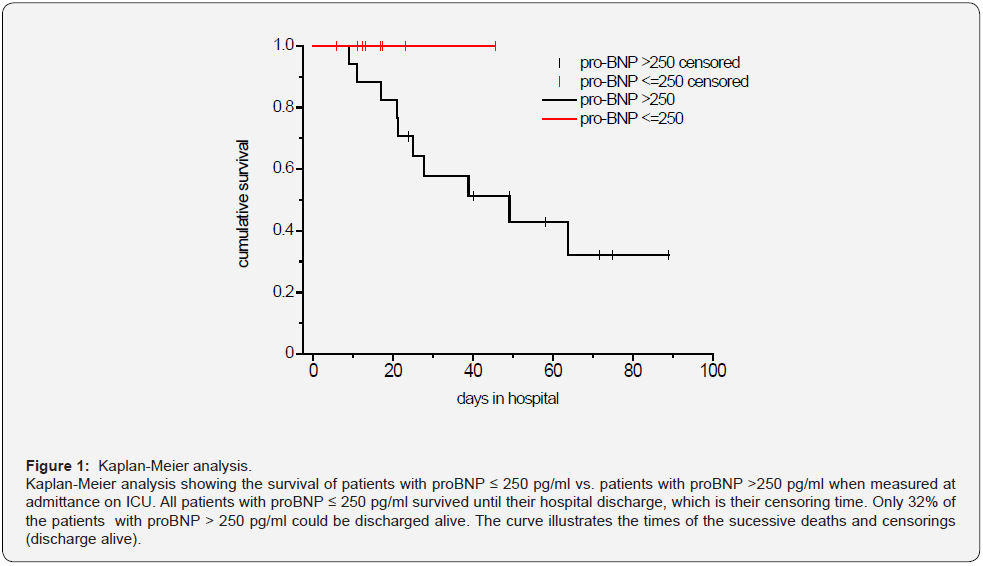
The majority of patients suffering from Bilateral Sudden Sensorineural Hearing Loss (BSSNHL) do not have an identifiable cause, leading to the classification of their condition as idiopathic BSSNHL. Only 10% of patients exhibit an identifiable cause [8]. A study revealed that some patients developed idiopathic BSSNHL after suffering from an upper respiratory tract infection (RTI) or oral herpes [9]. Another study in 2016 reported that, out of 16 BSSNHL patients, 5 had an idiopathic BSSNHL while others were observed to have different malignancies, such as neurofibromatosis, as shown in the picture below (Figure 1) [10]. BSSNHL can also result from radiotherapy in Head and neck cancer patients. A study investigated the hearing ability of 36 re-irradiated survivors of nasopharyngeal carcinoma. Among them, 91% exhibited abnormal cVEMP, 75% had abnormal oVEMP, 67% showed a reduced bone-conducted mean hearing level, and 39% had abnormal caloric tests. The study suggests that BSSNHL can occur after 10 years of radiotherapy [11]. Despite these findings, various theories on the etiology of BSSNHL are discussed below.
Infectious
Viral infections are among the most common causes of BSSNHL. According to a study by W R Wilson [12], 12 viral infections can cause Bilateral SSNHL through three mechanisms: (a) Cochleitis or Neuritis of the cochlear nerve. (b) Relapse of latent viral infection in the inner ear. (c) Indirect damage of the inner ear antigen when any distant viral infection initiates an antibody response without direct inner ear infection. However, majority of the literature supports the first two methods of BSSNHL due to viral etiology.
Among various viruses, the mumps virus is known to cause BSSNHL in rare cases. In 1992, Okamoto et al. conducted a serology study of 131 patients with sudden hearing loss suggesting that mumps was the cause in 9 out of 131 cases13. However, a couple of studies [13,14] suggest that mumps is responsible for only a small fraction (i.e., >10%) of cases of SSHL, without distinguishing between unilateral and bilateral SSNHL. Moreover, all of the eight members of the Herpes virus family (HS Type I & II, Varicella Zoster, EBV, CMV, HHV-6, 7, and 8) are known to cause SSNHL [15]. These viruses remain latent in the host even after remission and may cause SSHL upon reactivation. Besides herpes, other viruses such as adenovirus and arenavirus 14 are also known to cause BSSNHL.
In a case study by Chanmi Lee et al. [16] an HIV-infected patient with 8th cranial nerve involvement was found to suffer from BSSNHL [6]. Regarding indirect damage to the inner ear due to systemic viral infection, a 1998 study reported no elevation of MxA protein in any of their 20 patients with sudden hearing loss [16]. There have been reported cases of bilateral SSNHL after bacterial cryptococcal meningitis due to Cryptococcus neoformans. YH Chen et al. [10] studied 16 patients suffering from BSSNHL, and one patient, a 46-year-old male was suffering from cryptococcal meningitis, which was confirmed and cultured from his cerebrospinal fluid (CSF) findings. The cryptococcal infection which to the meninges and auditory canals of the inner ear, leading to BSSNHL along with vestibular loss.
Autoimmune
The concept of the immune system's involvement in inner ear pathology was first proposed by McCabe [17]. In patients with progressive Bilateral hearing loss, Harris & Sharp [18] demonstrated the presence of autoantibodies against various cochlea antigens [18]. As the majority of SSNHL cases lack a specific cause, certain assumptions regarding etiology have been suggested in order to predict the probable cause. One such assumption is autoimmunity, based on the idea that antibodies or activated T cells play a role in causing SSNHL by either cross-reaction or damaging in the inner ear, respectively [19]. Analysis of data for BSSNHL from different articles, it became apparent that the phenomenon of autoimmunity is more prevalent in females.
Research indicated the presence of underlying systemic autoimmune pathologies, such as Cogan's disease and Guillain-Barré syndrome, which manifested as BSSNHL [20]. Additionally, the suspicion of an underlying systemic autoimmune disease is raised when rapidly progressive bilateral sudden hearing loss responds positively to steroid therapy [21]. One notable autoimmune disorder is Multiple Sclerosis (MS), where 92% of cases reported SSNHL when hearing loss appeared as an early symptom, while gradual loss of hearing was present in 88% of cases during the late phase of the disease [22]. In conclusion, further studies and data collection are expected to provide a clearer understanding of the occurrence of BSSNHL in various pathologies with an autoimmune background
Vascular
In conclusion, further studies and data collection are expected to provide a clearer understanding of the occurrence of BSSNHL in various pathologies with an autoimmune background. A detailed study on the pathogenesis of BSSNHL [23] identifies three potential reasons behind the vascular etiology of BSSNHL: (a) Total and irreversible vascular occlusion, (b) Total and reversible vascular occlusion, and (c) Relative ischemia of the cochlea. Total vascular occlusion is primarily attributed to the occlusion of arteries at the base of the brain [24]. Regarding relative ischemia of the cochlea, the most widely accepted theory suggests that it results from the hyperviscosity of blood due to increased hematocrit and red cell distribution width (RCD).
In 2016, a study proposed that 5 out of 16 patients with BSSNHL had a vascular etiology [25]. This is often linked to the occlusion of the anterior inferior cerebellar artery (AICA) due to an atheromatous plaque forming in the basilar artery, leading to decreased blood flow and subsequent BSSNHL 24 However, it is crucial to note that occlusion of the basilar artery is associated with a high mortality rate and poor prognosis in survivors it may present as impending brainstem infarction. Accompanied by vertigo and nystagmus may occur before bilateral SSNHL [10].
Membrane Rupture
Membrane rupture seldom occurs spontaneously, typically arising from sudden pressure changes in the inner ear, severe head injuries, intense exercise, or deep barotrauma in the ear. A 1986 study proposed that the formation of a labyrinthine fistula leads to tiny holes between the niche of the round window and the posterior semicircular canal ampule. This, in turn, causes a rupture of the Reissner membrane, leading to a mixture of fluids and resulting in cochlear malfunction [23].
Diagnosis of BSSNHL
As stated earlier, data for the bilateral pattern for SSNHL is limited, only about 1.1% of all the patients with SSNHL came with this complaint of bilateral loss when data was evaluated of patients from 1995-2014 (i.e. total patients of SSNHL were 1459, 16 of them were there with this issue of SSNHL affecting both the ears). 10 Diagnostic criteria for BSSNHL include an additional clause to be fulfilled that SSNHL should affect both ears concomitantly within a period of 72 hours. The bilateral form of SSNHL can be categorized based on duration: simultaneous (both ears affected within 72 hours), sequential (one ear takes more than 72 hours but less than 30 days to be affected), and progressive (lacking a sudden onset, as both ears take more than 30 days to be affected)
Management of BSSNHL
Sudden Sensorineural hearing loss (SSNHL) is considered an otologic emergency and requires effective and early management [26]. According to the Clinical Practice Guidelines 2019 for SSNHL, clinicians should offer intratympanic (IT) steroid therapy for patients with incomplete recovery within 2-6 weeks after the onset of symptoms (KAS 10). Clinicians may also consider corticosteroids within the first 2 weeks of onset of SSNHL (KAS 9a). Hyperbaric oxygen therapy can be combined with steroid therapy within 2 weeks of onset (KAS 9b), or the combination can be used as salvage therapy within 1 month of the onset [27]. Historically, the management includes the use of steroids as standard therapy, which can be administered orally, intravenously, or via Intratympanic Injections. However, the therapeutic value of corticosteroids remains unpredictable [28].
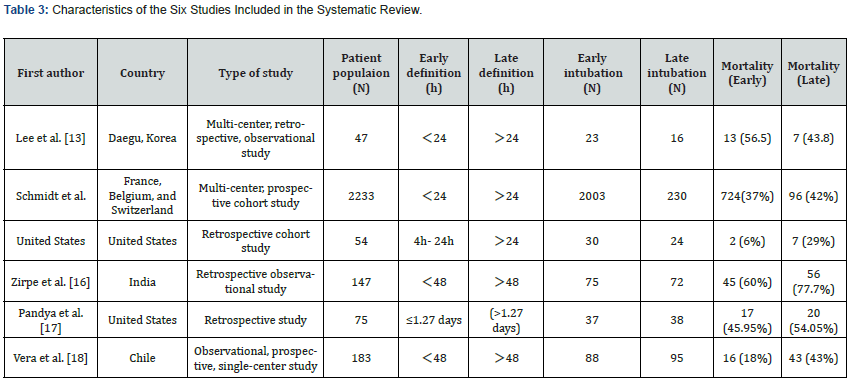
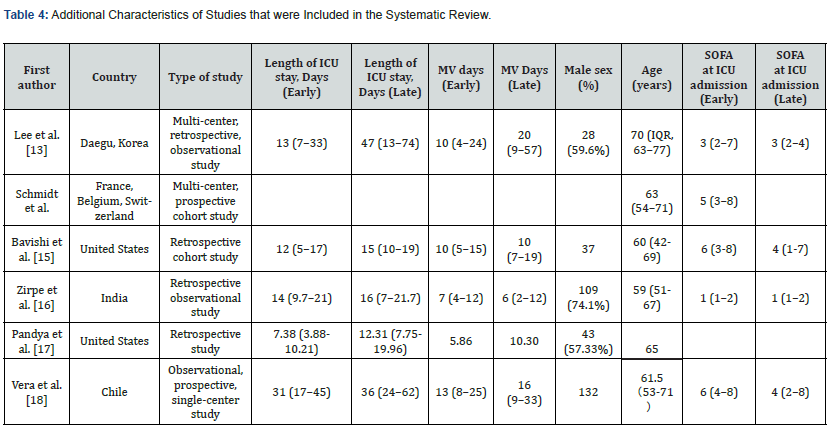
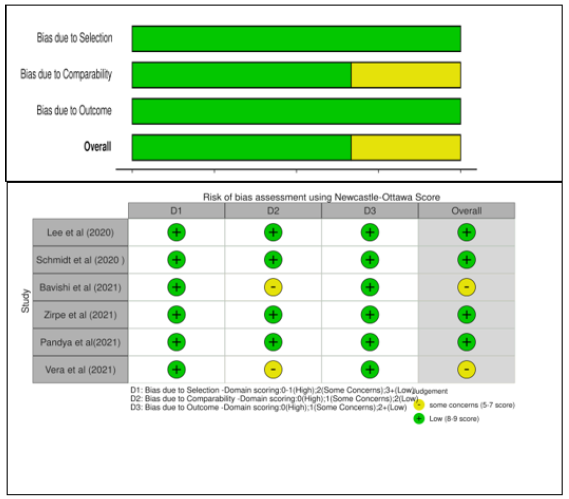
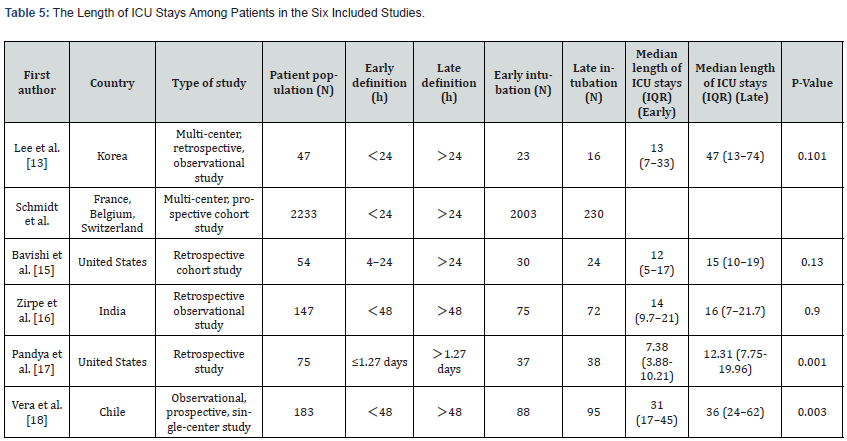
A systemic review and Meta-analysis compared Intratympanic vs Systemic Corticosteroids as the first-line treatment. The Data of 710 patients suggested no significant difference between the therapeutic effect of the two methods of administration and neither of their combinations improved the hearing outcomes more than either of the methods separately. The table below shows the crux of other studies for BSSNHL treatment outcomes [29]. In a Systematic Review and Meta-analysis conducted in 2022 with sample of 496 patients [30], with similar results were observed in terms of hearing outcomes of Intratympanic vs Systemic corticosteroids as a first line treatment. Although no significant difference was found between the two methods, the preference for Intratympanic steroids was suggested due to the observation of more serious side effects with systemic administration of dexamethasone compared to local adverse effects of Intratympanic injections [31].
In a Randomized Controlled Trial (RCT) involving 136 patients, where 66 received Hyperbaric Oxygen (HBO) therapy along with pharmacological treatment (HBO+P) and 70 received pharmacological treatment alone (P), statistically significant differences in outcomes favored HBO+P [32] Another RCT with 171 SSNHL patients indicated that the combination of HBO therapy and oral steroids was the most effective treatment when initiated two weeks after symptom onset [33]. A Systematic Review and Meta-analysis covering the period from January 2000 to April 30, 2020, with 130 participants, statistically suggested improved hearing outcomes in SSNHL patients who received HBO treatment, or its combination treatment compared to those given control therapy [34]. Alternative treatments include sound therapy combined with pharmacological treatment and adjuvant transcranial random noise stimulation with conventional treatment. The combination of sound therapy and pharmacological treatment demonstrated an improvement in noise thresholds and speech recognition, implying better recovery of hearing abilities compared to pharmacological treatment alone [35].
BSSNHL In COVID-19
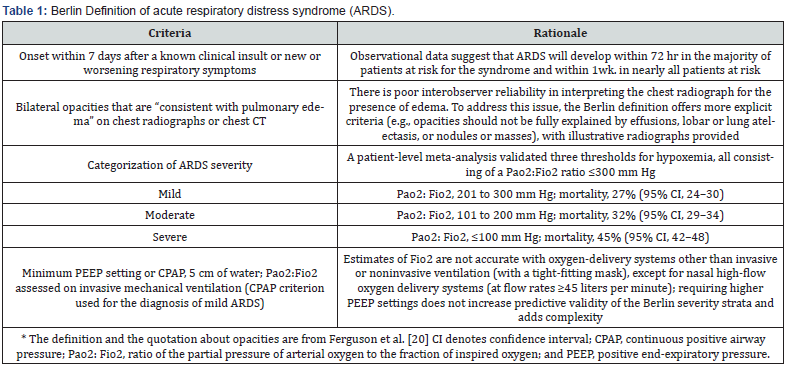
Discovered in December 2019 in China, the COVID-19 pandemic has had widespread hazardous effects globally. Nations faced significant challenges, impacting various aspects of daily life. Publicly practiced precautions included the use of face masks, handwashing, avoidance of crowded gatherings, and maintaining physical distance [36]. Clinically, COVID-19 manifests with a diverse range of symptoms, from self-limiting upper respiratory tract infection symptoms to severe consequences such as pneumonia, multi-organ system failure, and death [37]. In the context of otologic symptoms associated with COVID-19, available literature is limited. A case report highlighted an elderly patient with Sudden Sensorineural Hearing Loss (SSNHL) and a positive COVID-19 status. Unfortunately, the report lacked further findings, including audiometric or imaging studies [38].
However, a case report in 2020 focused on COVID-19 associated with Bilateral Sudden Sensorineural Hearing Loss (BSSNHL). Alexander Chern et al. [39] reported an 18-year-old female patient who presented with BSSNHL seven weeks prior. The patient also experienced loss of taste and smell, and her father tested positive for COVID-19 antibodies. Audiometric results indicated hearing loss in both ears, with the right ear having an average pure tone level (PTA) of 60dB and the left ear showing moderate to severe hearing loss with a PTA of 63dB. Word recognition scores were 88% for the right ear and 80% for the left ear. Tympanometry results were normal, indicating no middle ear issues. The patient reported no other neurological problems or family history of hearing [39]. Although the mechanism by which COVID-19 may cause dizziness is unclear, the disease does appear to be associated with individual cranial neuropathies resulting in anosmia [40]. It was concluded that COVID-19, besides its many other effects on the patient's health, can also interfere with the hearing ability of the patient leading to the expression of SSNHL.
Prognosis of BSSNHL
While the prognosis for unilateral Sudden Sensorineural Hearing Loss (SSNHL) is generally favorable, with many patients recovering fully within days to weeks, the outlook for Bilateral SSNHL (BSSNHL) is typically poor without immediate treatment [10] Abnormal caloric tests and oVEMP often signal a poor prognosis for BSSNHL, while a good prognosis is associated with a normal caloric test and oVEMP.
Conclusion
Bilateral Sudden Sensorineural Hearing Loss (BSSNHL) is a rare condition, occurring in only 1-2% of patients with Sudden Sensorineural Hearing Loss (SSNHL). Due to its rarity, there is a scarcity of studies specifically addressing the causes, management, and prognosis of BSSNHL. Traditional literature highlights various theories regarding its etiology and management; however, the condition still tends to have a poor prognosis even with oral and intratympanic steroids and hyperbaric oxygen therapy (HBOT).
To Know more about Global Journal of Otolaryngology
Click here: https://juniperpublishers.com/gjo/index.php
To Know more about our Juniper Publishers
Click here: https://juniperpublishers.com/index.php