Diabetes & Obesity - Juniper Publishers
Abstract
Background: Compounded errors during insulin
administration may impact the efficacy of diabetes control. Our major
objective was to quantify the various errors committed by patients
during insulin therapy.
Methods:This was a multicentric,
observational study in which participants were asked to respond to a
specific questionnaire under the supervision of a trained nurse,
addressing problems and risks of insulin self-administration. The study
included 140 individuals aged 6-75 years, with type 1 or type 2 diabetes
on insulin for more than 6 months, allocated to adults or youth groups.
Results:Comparing performance of adults vs
youth groups for withdrawal of 7 IU the rates of correct doses were
66.7%vs100% with 30U syringes (p=0.002); 70.8%vs95.0% with 50U syringes
(p=0.022); and 50.8%vs40.0% with 100U syringes (p=0.370), reflecting
poor performance in both groups. With the target dose of 22U, the rates
of correct doses were 67.5%vs100% with 30U syringes (p=0.003);
66.7%vs95.0% with 50U syringes (p=0.010); and 52.5%vs50.0% with 100U
syringes (p=0.836), again reflecting poor performance in both groups
with a higher dose. Other major errors included: improper rotation
technique in 62.5% of patients; failure to lift a skinfold in 29.2%;
premature withdrawal of the needle from injection sites in 45.8%;
totally correct injection technique was documented in 10%.
Conclusion:The results of the study point to
the urgent need for implementation of effective educational strategies
to provide patients with basic knowledge needed to minimize the
potential risks of insulin self-administration, including use of
appropriate insulin syringes according to size of injection dosage.
Keywords: Insulin therapy; insulin injection errors; insulin administration safety; diabetes treatment
Introduction
An overall assessment of glycemic control around the
world shows that only a small fraction of patients with type 2 diabetes
(DM2) achieve adequate glycemic control even after several years of
treatment [1-4]. In Brazil, 73% of patients with DM2 and no less than
90% of patients with type 1 diabetes (DM1) have poor glycemic control
(A1C > 7%), as shown by a recent Brazilian multicenter study in 6,671
patients across several diabetes care centers throughout the country
[1]. According to the Centers for Disease Control and Prevention, the
percentage of adults with diabetes in the United States with A1C>7%
reached 43% during the period of 2003-2006 [5].
The growing population of people with diabetes has
assumed epidemic proportions worldwide, with a consequent significant
increase in the number of insulin users. At the same time, wrong
information about correct techniques of insulin self-administration is
widespread and the consequences are highly worrying, since
incorrect delivery results in substantial modification of the
pharmacological action of insulin. This problem motivated a group of
leading medical experts and diabetes educators to develop New Injection
Recommendations for Patients with Diabetes, published in 2010 [6].
In patients with DM1 insulin therapy is an absolutely
requirement. On the other hand, increasing number of patients with DM2
need insulin treatment when oral therapeutic options do not lead to
desired glycemic control. However, resistance to initiating insulin
treatment is frequent among physicians and patients with DM2, which
slows or prevents the implementation of more intensive treatment
regimens, with obvious negative consequences in terms of chronic
complications of the disease. This refusal is mainly due to misbeliefs
on the part of patients, which includes fear of insulin injections. When
insulin is begun, this rejection is compounded by poor insulin
administration techniques that need to be urgently addressed and
overcome [7]. The condition known as “clinical inertia” applies when the
patient’s clinical conditions clearly indicate the need for
intensification or adjustment of the therapeutic approach, but
it is delayed-often for years in the case of insulin for DM2 [8]. A
publication by the American Diabetes Association lists the most
important myths and facts related to insulin administration [9].
The proper appreciation of the concept of “compounded
error” is essential to understanding the increased risk represented
by the combination of individual errors during insulin selfadministration.
According to the Merriam-Webster dictionary the
term “compound” refers to an error, condition or problem that
makes any outcome even worse [10]. Inadequate guidance and
patient compliance in relation to insulin self-administration are
two of the major problem areas among the education initiatives in
diabetes. In general, patients frequently receive a prescription for
insulin with little, if any basic orientation on the correct techniques
that will lead to successful treatment. The various technical errors
committed by patients in insulin self-administration are already
well-known to health care professionals but, to our knowledge,
have never been properly quantified. The Diabetes Education and
Control Group of the Kidney Hospital, Federal University of Sao
Paulo-UNIFESP promoted and coordinated a multi-center study in
order to identify and quantify the occurrence of technique errors
during insulin self-administration [11].
Material and Methods
This was an observational, non-interventional study in which
participants were asked to respond to a specific questionnaire
addressing the main problems and potential risk factors related
to insulin self-administration. In addition they were asked to
perform a practical demonstration of how they withdraw various
insulin doses from the vial into different syringes. The patients did
not have to inject the selected insulin dose.
Patients of both sexes, on insulin for more than six months,
aged 6-75 years receiving care at the Unified Health System
(SUS) in the six participating centers were chosen at random. The
study enrolled 140 individuals with type 1 or type 2 diabetes:
the coordinating center included 40 individuals and each of the
other five participating centers included 20 individuals. Patients
were allocated to two groups: adults (120 individuals) and youth
(20 children, adolescents and young adults with DM1). Nurses
responsible for implementing the study questionnaire in the
various centers received special training and were supervised
by a medical professional in each participating center. The
questionnaire contained 23 questions and practical observations
on insulin injection technique outlining errors commonly made
by patients (available at the appendix). The Study Protocol was
approved by the Research Ethics Committees (ECs) of each
participating center. The individuals included in the study or
parents or legal guardians signed consent forms in the case of
children and minors signed an informed consent to participate
in the study, which was conducted consistent with Good Clinical
Practice guidelines and the Declaration of Helsinki.
Primary objectives of the study included: to obtain information
enabling a proper mapping of insulin self-administration
practices in the public health service; to evaluate the adequacy
of self-administration techniques used by patients; to evaluate
the main problems and potential risk factors involved in insulin
self-administration which may influence clinical outcomes and
the safety of insulin treatment. Secondary objectives of the study
included: to evaluate the demographics of a sample of 140 patients
under insulin treatment; to obtain information on prescribed
doses of intermediate, long- and short-acting insulins used by
these patients.
The following parameters were evaluated by the
attending
nurse after patients’ demonstration: rotation technique was
assessed as correct or not; presence or absence of lipohypertrophy
was evaluated by clinical examination; and grading of injection
technique as correct, partially correct, or incorrect. Dose accuracy
testing (acceptable variation = prescribed insulin dose ± 1 IU) was
conducted by assessing the patient›s ability to draw the correct
doses of the prescribed insulin as directly observed by the nurse in
charge. Initially, the patient was asked to draw up a dose of 7
IU of insulin, using 30 IU (1-unit scale markings), 50 IU (1-unit
scale markings), and 100 IU syringes (2-units scale markings),
manufactured by BD, Franklin Lakes, NJ, USA. Then, the same
procedure was performed by the patient with a dose of 22 IU,
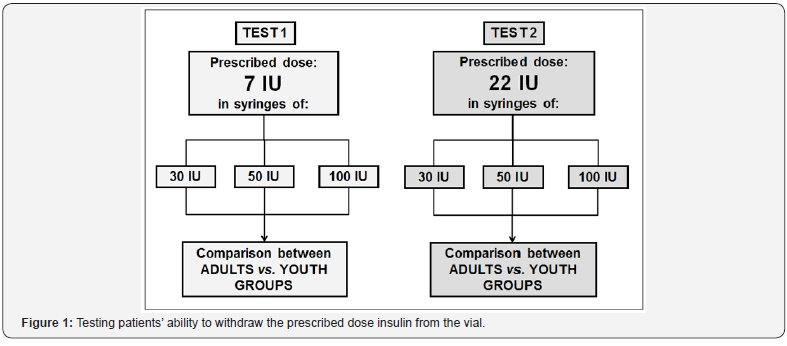
using the same syringes, as shown in (Figure 1). The 7 IU testing
dose was chosen for being a low and odd number and the 22 IU
testing dose was chosen for being a higher, even dose so that
accuracy was tested in two different situations.
Statistical Analyses
Categorical data were summarized by absolute and relative frequency of cases in relation to the total number of patients from
the adults and youth groups. Data with a normal distribution of
numeric and continuous parameters (e.g. ages) were summarized
as mean and standard deviation in each group together with
minimum, median and maximum values. Other parameters were
evaluated by median and quartile values. Adults and youth groups
were compared with respect to the percentage of patients who
had correctly withdrawn the requested insulin doses from the vial,
via the chi-square test. The statistical comparison of the number
of patients who made mistakes in the withdrawn dose with 100 IU
syringes compared to the 30 IU and 50 IU syringes was performed
using the McNemar test.
To check the characteristics of patients related to correct
and incorrect doses, the chi-square test was used on categorical
variables, and the Student’s t test in the variables with numerical
and continuous distribution. Statistical significance thresholds
were set at p <0.05. The data were obtained using the Minitab
statistical software, version 16.1.
Study Results
Patient Characteristics
(Table 1) shows the characteristics of patients with respect
to demographics, diabetes-related data and insulin delivery
practices in adults, youths, and in total group. An overview of the
study population showed that two-thirds of the adults were DM2,
with a slight preponderance of females. Adults were nearly 51
years of age on average, and youths, 15 years. Mean years since
diagnosis for more than 10 years were 2.3 times more frequent
in adults compared to youth. Considering the period of time
of >10 years adults were 1.4 times more experienced with insulin
therapy than the youth. Frequency of daily injections was higher
in youth compared to adults.
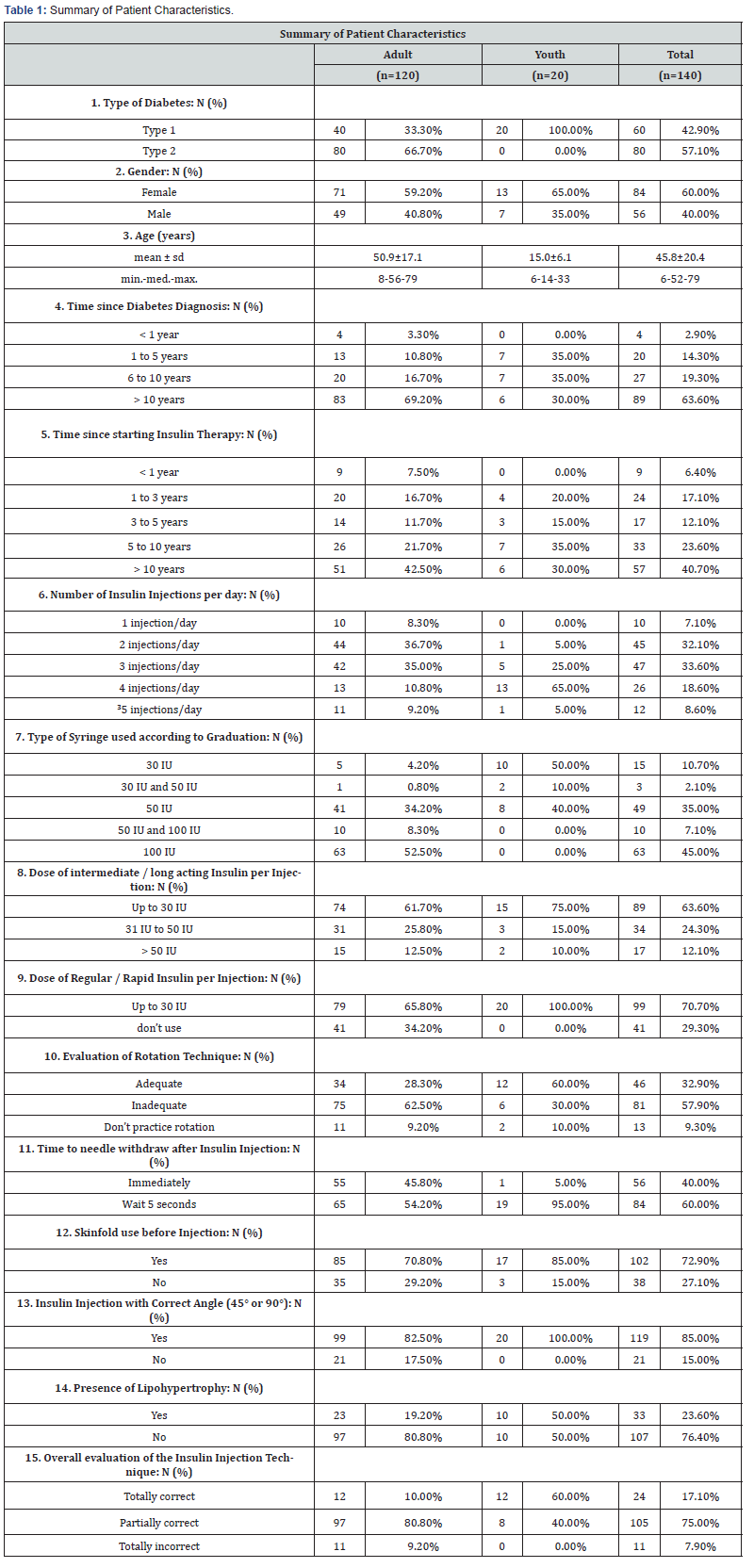
In the total group of our study population, the 100 IU syringes
were being used by 45.0% of patients, the 50 IU syringes by 35.0%
and the 30 IU by just 10.7% of patients, respectively. Either 30 IU
or 50 IU were used by 2.1% and either 50 IU or 100 IU were used
by 7.1%. Average doses up to 30 IU of intermediate/long acting
insulin and regular/rapid insulin were more frequent in both
adults and youth. Inadequate rotation technique was twice more
frequent in adults. Only 1/10 of adults and 1/10 of youth did not
practice rotation. A high percentage of adults and youth performed
skinfold before injections. Insulin injection with correct angle
(45º or 90º) was a frequent practice both by adults and youth.
Lipodystrophy was 2.6 times more frequent in youth, compared
to adults. In the overall evaluation of insulin injection technique
by the supervising nurse the percentage of youth practicing the
correct technique was 6 times higher in youth than in adults.
Correct and incorrect Insulin Doses withdrawn from the Vial
In relation to the precision in withdrawing the correct dose
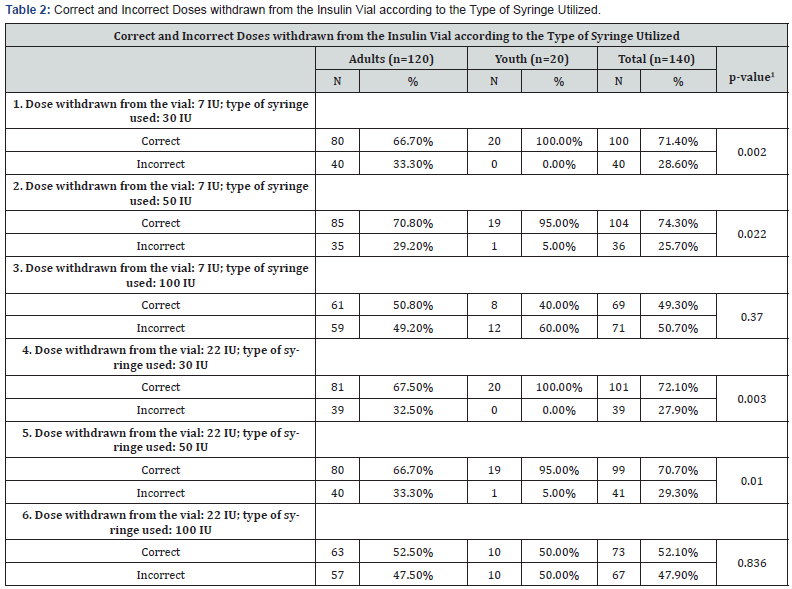
from the vial, the statistical comparison between adult and youth
groups showed that young patients make less errors than adults
when using 30 IU or 50 IU syringes, whether in drawing 7 IU dose
(p = 0.002 for 30 IU syringe; p = 0.022 for 50 syringe IU) or in
drawing 22 IU dose (p = 0.003 and p = 0.010 for 30 IU syringe and
50 IU syringe), but there is no significant difference when used
syringes of 100 IU (p=0.370 for the 7 IU dose and p=0.836 for the
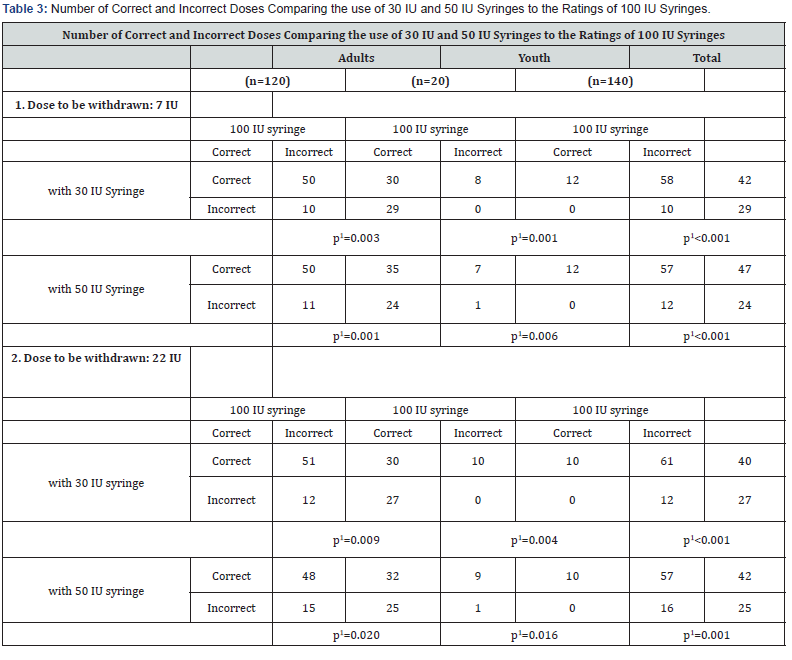
22 IU dose) (Table 2). The superiority of 30 IU and 50 IU syringe in
comparison to 100 IU syringe in terms of accuracy in withdrawing
the correct insulin dose is well stablished as seen in (Table 3).
In relation to the precision in withdrawing the correct dose
from the vial, the statistical comparison between adult and youth
groups showed that young patients make less errors than adults
when using 30 IU or 50 IU syringes, whether in drawing 7 IU dose
(p = 0.002 for 30 IU syringe; p = 0.022 for 50 syringe IU) or in
drawing 22 IU dose (p = 0.003 and p = 0.010 for 30 IU syringe and
50 IU syringe), but there is no significant difference when used
syringes of 100 IU (p=0.370 for the 7 IU dose and p=0.836 for the
22 IU dose) (Table 2). The superiority of 30 IU and 50 IU syringe in
comparison to 100 IU syringe in terms of accuracy in withdrawing
the correct insulin dose is well stablished as seen in (Table 3).
It is also observed that for the 7 IU dose the number of wrong
doses increases significantly when using 100 IU syringes both
among adults (p = 0.003 and p = 0.001, using the 30 IU and 50 IU
syringe, respectively) and among youth (p = 0.001 and p = 0.006
using 30 IU and 50 IU syringes, respectively). Similar results were
observed when the test dose of 22 IU was used (Table 3).
Characteristics of patients who scored or missed the dose to be withdrawn
Patients were classified according to their accuracy in
drawing up the correct or incorrect insulin dose from the
vial. A correct dose was defined as drawing up 7 IU ± 1 IU and
22 IU ± 1 IU, regardless of the type of syringe used (30 IU, 50 IU
and 100 IU). If any dose was drawn incorrectly, it was considered
«error» (Table 4).
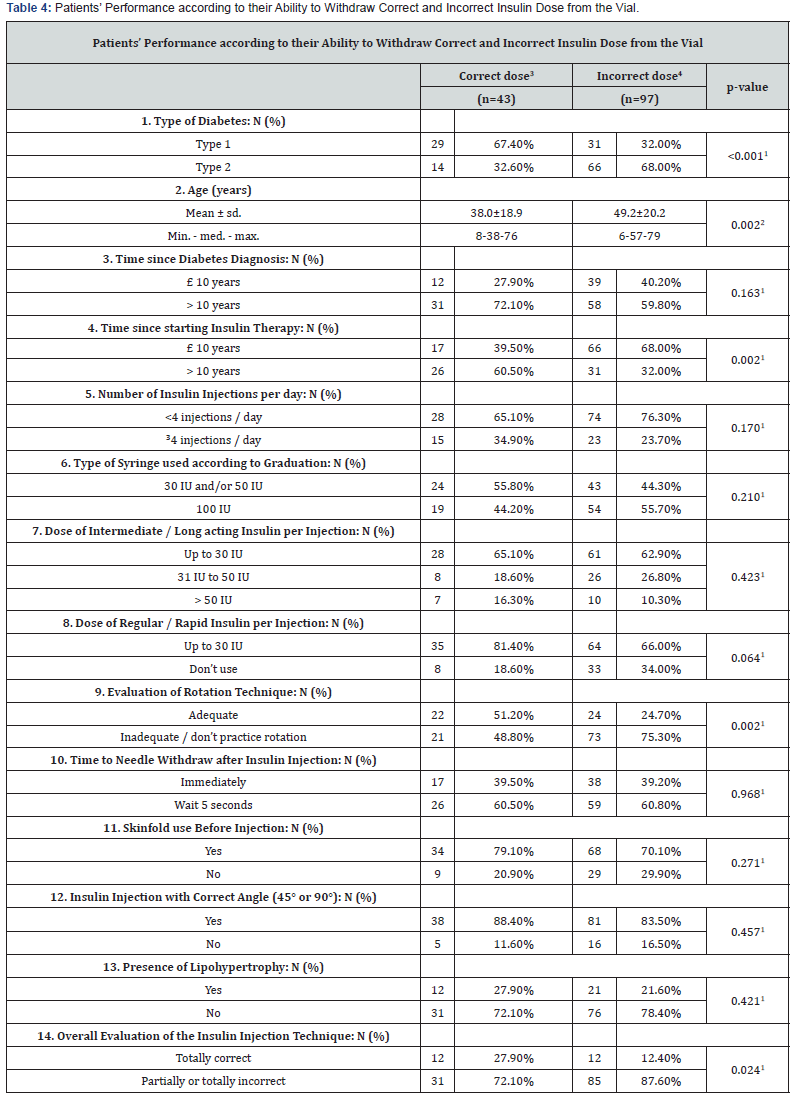
1Chi-square test ; 2Student’s t test;
3Correct dose in drawing the insulin dose from the vial (7 IU and 22
IU), with any of the syringes utilized (30 IU,
50 IU, 100 IU); 4any error in terms of dose withdrawn from the vial (7
IU and/or 22 IU), with one or more syringes (30 IU, 50 IU, 100 IU).
Discussion
Insulin self-administration is often done incorrectly, and
this can lead to risks, especially when different types of errors
occur simultaneously (compounded errors) [12,13]. These
issues, summarized in (Table 1), can substantially modify the
pharmacokinetics and pharmacodynamics of injected insulin,
greatly increasing the risk of hypo-or hyperglycemia. Among the
many errors occurring during self-administration of insulin, the
most serious and unforeseen is the incorrect drawing up of doses
from vials.
Despite rapid technological advances in insulin formulations
over recent years, injection technique has not been given much
attention in the management of injectable therapies [14]. Our
study reveals a number of critical problems related to basics of
insulin injection technique that may interfere with its expected
pharmacological profile. Many problems can be avoided by
adopting proper technique [6]. Theoretically, it should be expected
that errors in insulin administration could be more frequent in
patients who are less experienced with the disease and, more
specifically, with the practice of insulin therapy.
(Table 4) shows the characteristics of patients according to
correct or incorrect withdrawn dose. It can be observed that the
type of diabetes (DM1 or DM2), age, time since start of therapy
with insulin, the insulin administration rotation technique (proper / improper) are factors that correlate to correct or
incorrect doses in withdrawing insulin dose. Patients who
make more mistakes in withdrawing the insulin dose are older
(p = 0.002), with DM2 (p <0.001), who started insulin therapy
less than 10 years ago (p = 0.002), and that do not use proper
rotation technique or that do not rotate the insulin injection at
all (p = 0.002). Patients that were considered by the supervising
nurse as having poor insulin administration technique also made
more errors than those with a totally correct approach to insulin
injections (p = 0.024) (Table 4).
The results of the study also showed the higher performance?
of 30 IU and 50 IU syringes for the prevention of a major problem
in insulin self-administration. There is a substantial risk of
withdrawing incorrect doses when using 100 IU syringes, which
are graded by 2 IU, making it difficult the reading of syringe scale.
The replacement of the 100 IU by 30 IU or 50 IU syringes, according
to the needs of each patient, is an important preventive strategy to
avoid technical errors in insulin self-administration, particularly
for patients in the public health service who generally do not have
access to educational programs which provide adequate guidance
on the correct techniques for this procedure. To our knowledge,
no other study approached this problem with the 100 IU syringes
as a serious risk factor for in proper selection of insulin dose.
In the total group of our study population, the use of 100 IU
syringes was far more frequent than 50 IU syringes and 30 IU. If
the 100 IU syringes are the least safe option for insulin injections,
why not give preference to 30 IU or 50 IU syringes? The basic
question is the average insulin injection individual doses to make
sure that the volume of insulin utilized with the 100 IU syringes
would fit the available volumes of 30 IU or 50 IU syringes. Our
data show that a minority of our patients was using individual
doses greater than 50 IU of NPH or long acting analogs and all
of them were injecting less than 30 IU of regular or short acting
analogs or were not using short acting analogs at all. These data
indicate that the vast majority of patients could be using 30 IU or
50 IU syringes instead of 100 IU syringes. It should be noted that
patients who take both NPH and regular insulins in our service do
so with two separated injections instead of mixing in one single
injection.
The other critical finding of the study was that 67.2% of
patients utilized improper rotation technique or did not rotate
at all. The consequence of improper site rotation technique is
the increased risk of lipohypertrophy, which is also related to
increased frequency of reuse of insulin needles [15]. In our study,
lipohypertrophy affected 23.6% of the study participants, but
this may be an underestimation due to diagnostic difficulty in
identifying small lipohypertrophy nodes (Table 1). Another recent
study on the prevalence of lipohypertrophy showed that 64.4% of
patient had this complication [16].
Another potentially problematic issue was the finding that a
fair proportion of patients removed the needle immediately after
the injection, without waiting the recommended 5-10 seconds.
The purpose of this dwell-time is to avoid reflux of insulin from
the injection site. Use of skinfold and injection with a correct
angle of 45º or 90º (according the clinical situation) for insulin
administration was reported by the majority of patients.
Study Limitations
This study addressed several aspects relevant to the good
practice of insulin self-administration. However, other key issues
have not been properly surveyed, including the following:
1. The unequal distribution of participants between the
adult group (n = 120) and the youth group (n = 20) may have
an impact on the interpretation of statistical significance of
differences found between the two groups. As shown in (Table 2)
2. Frequency and clinical impact of inadequate mixing of
NPH insulin for complete resuspension. In a study of 109 patients
using NPH insulin it was recommended that they should roll and
tip the pen cartridge at least 20 times in order to get adequate
insulin resuspension but, in fact, only 9% of these patients
actually tipped and rolled the cartridges more than 10 times. As
a consequence, NPH insulin concentration ranged from 5% to
214% and varied by more than 20% in 65% of the 109 patients
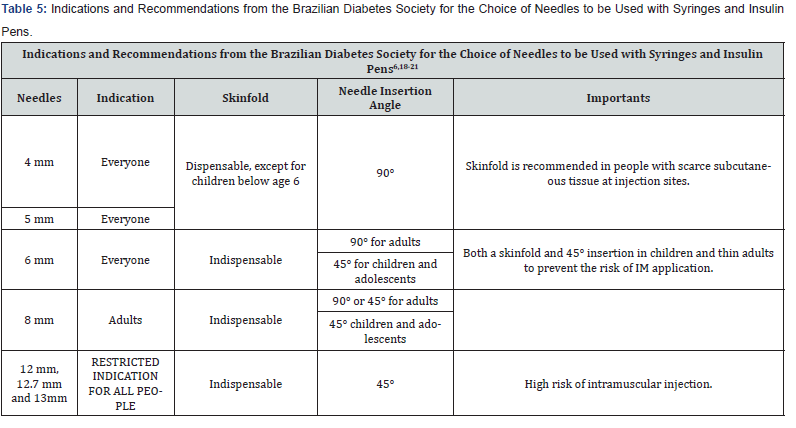
[17]. Directions and recommendations for the use of needles for
insulin syringes or pens are summarized in (Table 5), adapted
from the Brazilian Diabetes Society - 2014-2015 guidelines [18]
and other related papers [6,19-21].
Summary and Conclusion
There are several obstacles and technical errors commonly
observed in patients who practice self-administration of insulin,
significantly increasing the likelihood of unsuccessful treatments
[22-27]. The main topics that deserve full attention of the health
team responsible for guiding the diabetic patient are summarized
below:
1. Errors in insulin administration occur in clusters and in
line with the concept of “compounded errors”. Consequently,
the final negative impact is greater than the sum of
consequences of individual errors.
2. The myths that impair or impede the acceptance of
insulin by diabetic patient should receive proper attention
from health care team [28-30]. If this problem is not overcome,
it will be almost impossible to implement safe and effective
insulin therapy.
3. Although most of the study population already had
experience with diabetes and insulin therapy for more than
10 years, the frequency of important technique errors during
the study was a matter of deep concern.
4. Among all the observed problems, errors in the
withdrawing of the prescribed dose from the insulin vial
reached highly alarming proportions, since 50% of adults and
60% of younger patients drew up incorrect doses of insulin
when using a 100 IU syringes [31-33].
5. Although not included in the study objectives, it is
important to note that the 12.7 mm long needles represent
a high risk of intramuscular insulin injection and therefore
should be quickly replaced by 8 mm needles (or preferably,
6 mm) for syringe users and 4 mm or 5 mm for pen users [21].
6. Final message: the implementation of interdisciplinary
groups of diabetes education is a key strategy to overcome the
misinformation that is the biggest problem responsible for
the high rate of uncontrolled diabetes [34,35].




No comments:
Post a Comment