Aims: To re-evaluate whether augmentation of
labor with oxytocin in dysfunctional labor, has a hazardous effect on
neonatal Apgar scores, umbilical cord pH or blood gases
Materials and Methods: Prospective study
where one hundred and fifty-three (153) patients in spontaneous labor
were involved in the analysis. Seventy-nine patients (Group I) with
hypo-contractile uterine activity were managed by low-dose oxytocin
protocol for labor augmentation, while 74 patients (Group II) were not
managed by augmentation of labor using oxytocin. Primary outcomes were
Apgar score at 5th minutes of birth and umbilical artery pH, while
secondary outcomes were Apgar score at 1st minute, arterial pO2, pCO2
and base deficit of all neonates.
Result: In this study, there was no
significant difference between cases and controls regarding; Apgar score
at 1st minute, Apgar score at 5th minute, mean umbilical artery pCO2
and pO2 while mean umbilical artery pH was significantly lower and
umbilical artery base deficit was significantly higher in the case group
compared to the control group. Moreover, umbilical artery pH was
negatively correlated to duration of oxytocin administration.
Conclusion: Oxytocin use to augment labor,
although affects umbilical cord blood gases, doesn’t significantly
affect neonatal outcome if used in a proper dose to produce efficient
uterine contractions
Keywords: Apgar score Augmentation Cord gases Oxytocin
Approximately 20 percent of labors involve either
protraction or arrest disorders [1]. The active management of labor was
introduced during the 1960’s at the National Maternity Hospital in
Dublin, Ireland to augment labor in nulliparous women. Proponents of
this approach have suggested that it also safely reduces the number of
Cesarean deliveries [2]. Oxytocin increases frequency of contractions,
causes initial transient increase in the base tone (incomplete
relaxation) and increases the amplitude and duration of phasic
contractions [3]. During parturition, prolonged tonic contractions might
be harmful for fetuses because an increase of the intrauterine pressure
would disturb the feto-maternal circulation and may occlude blood
vessels within the myometrium [4]. Utero-placental hypo-perfusion is the
major cause of both respiratory and metabolic acidemia, with
progression from the former to the latter over time if decreased
utero-placental blood
flow is not corrected [5], hence various studies were designed to study
the safety of using oxytocin infusion during the course of labor on
neonatal clinical and acid-base condition at delivery and the likelihood
of causing perinatal asphyxia.
The study was conducted in Ain Shams University
Maternity Hospital and El-Sahel Teaching Hospital in Cairo, Egypt, which
are two big tertiary hospitals, from January till October 2010, where
180 patients in spontaneous labor were initially enrolled in this
case-control study after informed consent and approval of the study
protocol by the institute ethics committee. Ninety patients who
fulfilled the selection criteria, were diagnosed as primary failure of
progression in labor due to hypo-contractile uterine activity and
managed by augmentation of labor using low-dose oxytocin (Syntocinon® 10
IU/ml concentrate for solution for infusion) (Group I). Another group of
ninety patients also fulfilled
the selection criteria but were not managed by augmentation of
labor using oxytocin (Group II). Participants were all aged between
18 and 45 years old, free of medical disorders, planned for vaginal
delivery having singleton pregnancy at full term admitted at
3-5cm cervical dilatation with vertex presentation of estimated
fetal weight between 2500 to 4000 grams with average amniotic
fluid volume and morphologically normal fetus, with no evidence
of fetal distress or placental insufficiency and with uncomplicated
pregnancy as detected by antenatal course.
All neonates were assessed using Apgar score at 1st and 5th
minutes by same observer and umbilical cord blood samples
were obtained from all neonates where a segment of 10-20cm of
umbilical cord was doubly clamped and excised immediately after
delivery then 1-2ml blood withdrawn in a heparinized syringe;
one from the artery and the other from the vein then kept in ice
and transported to the laboratory within 60 minutes and analyzed
using blood analyzer (i-STAT300F, Abbott Point of Care Inc., USA).
Prior to start of the study, all participants were assessed to
confirm eligibility then were consistently managed according
to the local institutional intra-partum protocol and received
proper monitoring and supportive care. Normal FHR pattern
and assessment of uterine activity were confirmed using
Cardiotocography (CTG) for 30 minutes before starting
interventions. Intermittent auscultation was used in low-risk
women while continuous electronic fetal monitoring was used
for the high-risk cases. Vaginal examination was performed two
hourlies, unless clinically indicated, to monitor progress of labor.
Artificial rupture of fetal membranes (ROM) was considered,
in women with intact membranes, if there was poor progress of
labor (cervical dilatation <1cm/hour) with inefficient uterine
contractions 2hours after ROM, the woman was assigned to Group
I, receiving low-dose oxytocin protocol using oxytocin dilution of
10mU/mL, initial dose of 2mU/min (12mL/hr), and incrementalincrease of 2mU (12 mL) every 45 minutes until adequate
contractions with the maximum dose being 16mU/min (96mL/
hr) [6]. Interpretation of intrapartum fetal heart rate pattern and
uterine contractions was done according to ACOG guidelines [7,8].
Cases of uterine hyper-stimulation, antepartum hemorrhage,
cases needed instrumental delivery or emergency Cesarean
section, as well as neonates with apparent congenital anomalies at
birth were all excluded (11 from group I and 16 from group II) and
not involved in the analysis. The primary outcomes considered
were Apgar score at 5th minute of birth and umbilical artery pH,
while secondary outcomes were Apgar score at 1st minute of birth,
umbilical artery pO2, pCO2 and base excess of all neonates.
Statistical analysis was done on a personal computer using
IBM® SPSS® Statistics version 19 (IBM® Corporation, Armonk,
NY, USA). Kolmogorov-Smirnov test of normality was applied to all
measured variables where quantitative variables were described
as mean and standard deviation (SD), number and percentage,
or median and inter-quartile range (IQR) as appropriate. The
independent sample t-test was used to compare the two groups
as regards quantitative variables in parametric data while Mann
Whitney U test was used for non-parametric data and Chi square
test was used for qualitative data. Relative risk and Odds ratio were
used to calculate likelihood of negative effect with a confidence
interval of 95%. Pearson’s correlation was used for measuring
correlation between different variables. Significance level was
always set at 0.05.
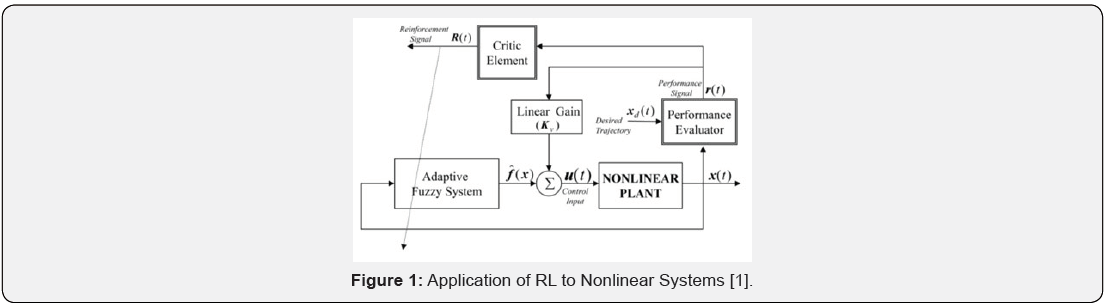
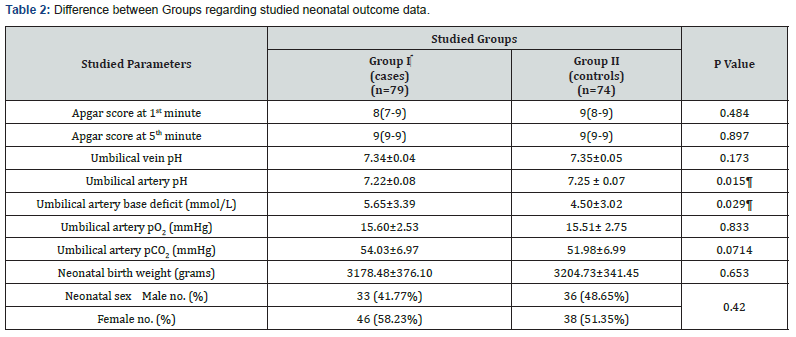
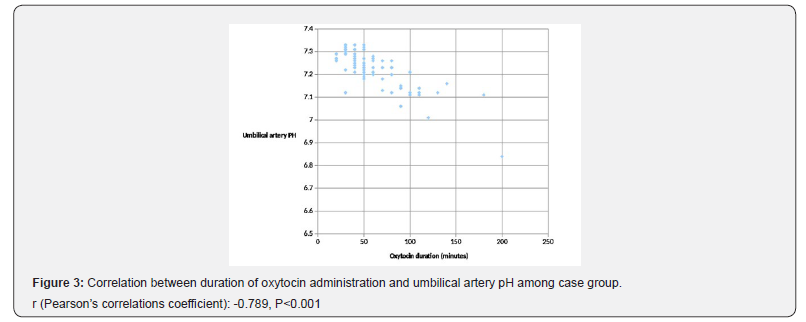
Statistical analysis included 153 patients; 79 in Group I and 74
in Group II. Table 1 shows no significant difference between cases
and controls regarding mean maternal age, BMI, gestational age,
parity and mean cervical dilatation at enrollment (P>0.05).
BMI body mass index [calculated as weight (kg) divided by squared height (m2)]
Kg, Kilograms; m2, square meters; cm, centimeters.
Analysis using independent student’s t-test or Mann Whitney U test as appropriate
Data are presented as mean ± standard deviation or median (interquartile range, IQR) as appropriate.
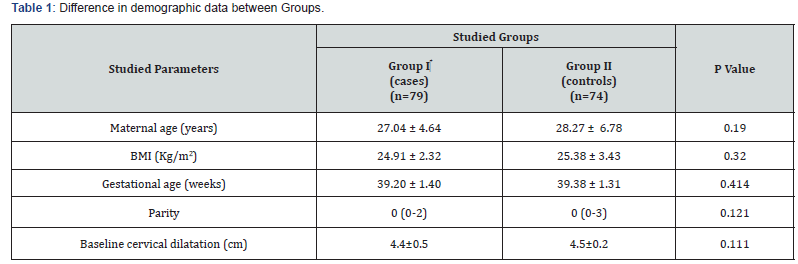
Analysis using independent student’s t-test, Chi square or Mann Whitney U test as appropriate
Data are presented as median (interquartile range, IQR), number (%) or mean ± standard deviation as appropriate.
¶ Indicates statistical significance.
Table 2 illustrates studied neonatal outcomes showing no
significant difference regarding neonatal weight, neonatal sex
distribution, Apgar score at 1st and 5th minutes, as well as mean
umbilical artery pCO2, pO2 and mean umbilical vein pH (P>0.05).
However, umbilical artery base deficit was significantly more
and pH was significantly less in case group (P=0.015; P=0.029;
respectively).
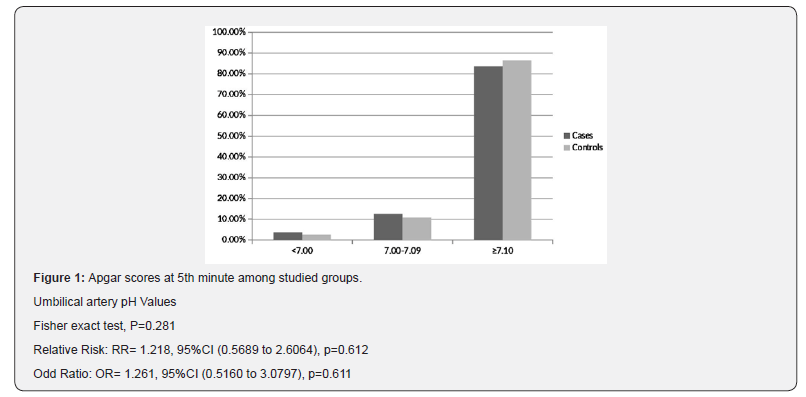
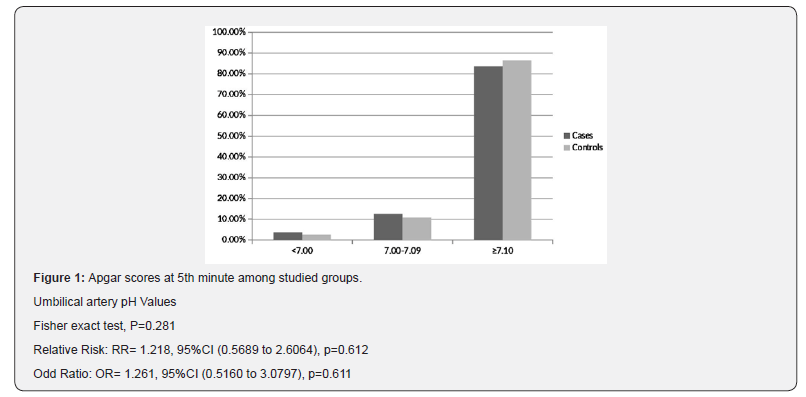
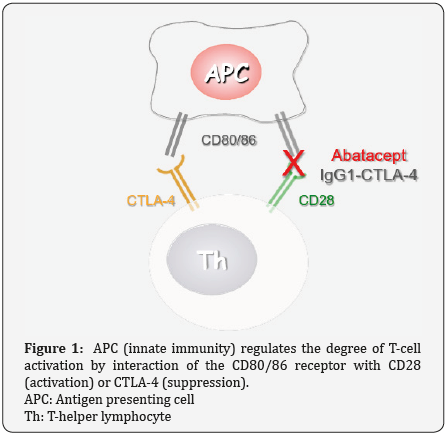
Interestingly, Figure 1 illustrates no significant difference
between cases and controls regarding number of neonates
with arterial pH less than 7.1 (13 (16.5%) versus 10 (13.5%);
respectively) (RR=1.218, P=0.612; OR=1.261, P=0.611; 95%CI),
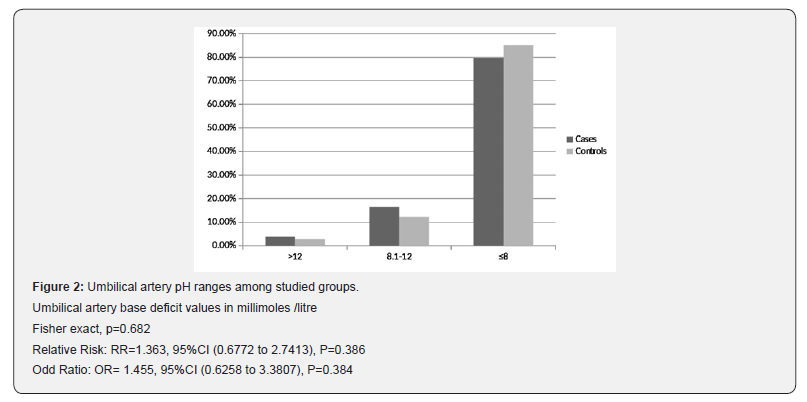
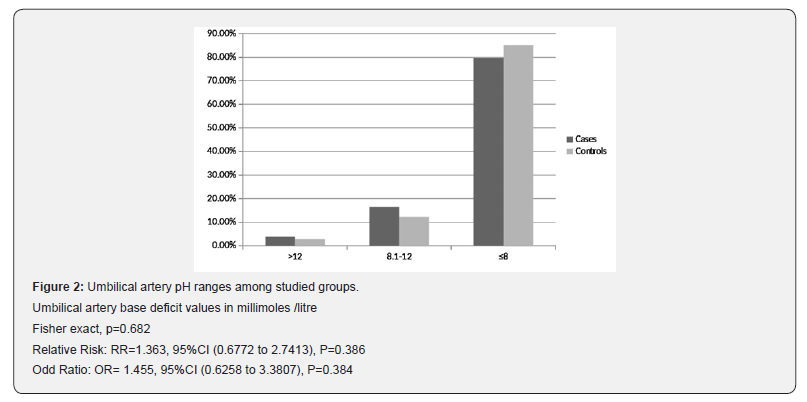
while Figure 2 shows that number of neonates with significant
impairment of arterial base deficit (>8mmol/L) didn’t show
significant difference between cases and controls (16(20.3%)
versus 11(14.9%); respectively) (RR=1.363, P=0.386; OR=1.455,
P=0.384; 95%CI).
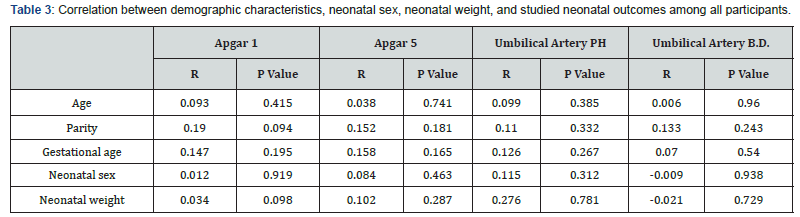
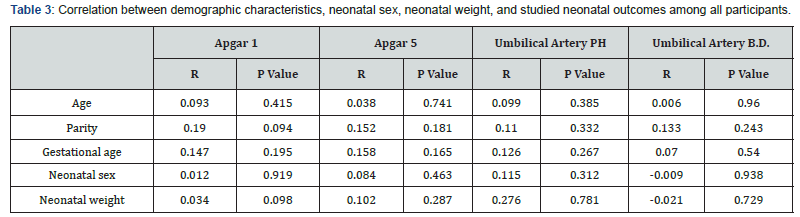
In this study, Apgar scores at 1st and 5th minute were not
correlated to any of maternal age, parity, gestational age, neonatal
sex or neonatal weight. Also, umbilical artery pH and base excess
have non-significant correlations to these variables (P>0.05; Table
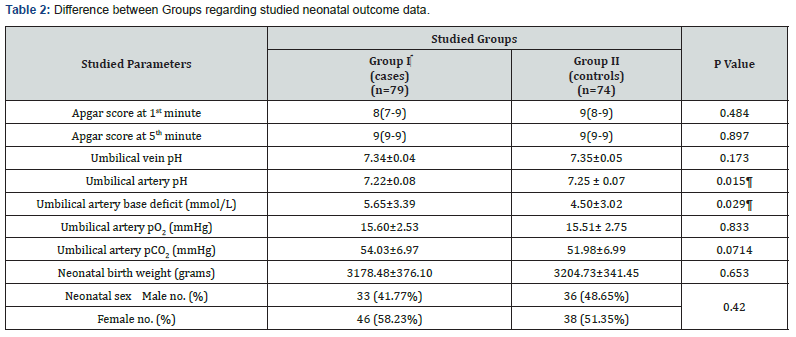
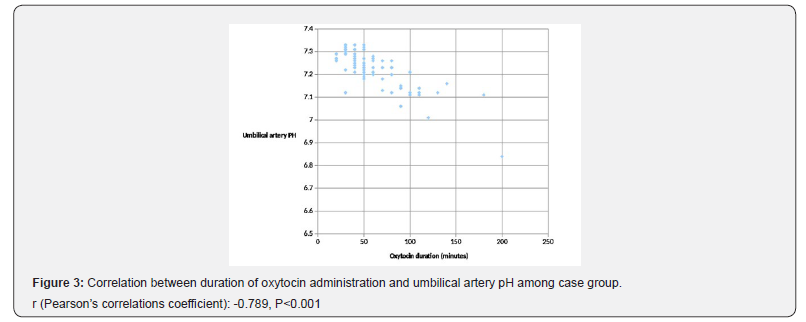
3). Figure 3 illustrates Pearson’s correlation test between duration
of oxytocin administration and umbilical artery pH among group I,
showing a significant negative correlation (P<0.001).
Although labor augmentation using oxytocin has been
investigated in few trials, most of these trials have focused on
various outcomes mainly duration of labor, rate of Cesarean
sections or instrumental deliveries and maternal experience
with few of them [9-11], have measured neonatal outcomes as a
primary outcome. The current study reported that low-dose oxytocin use is
associated with reduction of neonatal umbilical artery pH and
increase in base deficit without compromising the neonatal
clinical condition or affecting Apgar scores
Oxytocin transiently compromises fetal circulation
by increasing duration, frequency and strength of uterine
contractions where this effect was studied by Olofsson et al. [12],
through ultrasound and Doppler assessment where uterine and
umbilical artery flow resistance increased significantly during
uterine contractions reflecting rapid and exaggerated increase of
vascular resistance in both arteries.
The biochemical disturbance must be significant before Apgar
score is affected [13]. Moreover, a number of factors may influence
Apgar score, including trauma, drugs, infections, congenital
anomalies, hypovolemia, hypoxia and preterm birth. Accordingly,
it is inappropriate to use an Apgar score alone to establish the
diagnosis of asphyxia [14].
In the year 2008, oxytocin was added to the list of medications
designated as high alert by the Institute for Safe Medication,
USA [15]; such drugs are defined as those bearing a heightened
risk of harm when used in error. Not following the guidelines
regarding use of oxytocin is probably one reason for adverse
neonatal outcomes. The use of oxytocin is on the increase and it
is estimated that about 50% of nulliparous and 20% of parous
women receive oxytocin during delivery [16]. A recent Cochrane
review by Kenyon et al. involved 4 randomized trials and found
no significant difference for Apgar scores, umbilical cord blood
gases, admission to special care baby unit, or neonatal mortality
between cases managed by high-dose and those managed by lowdose
oxytocin for labor augmentation [17].
The current study found no statistical difference neither in
Apgar scores at 1st and 5th minutes nor in distribution of Apgar
score values between both groups, where 5 neonates (6.3%) of the
case group and 4 neonates (5.4%) of the control group had a score
less than 7 at 1st minute while one neonate of each group had ascore less than 7 at 5th minute. No neonatal deaths were reported
during the study. Three Neonates were diagnosed with TTN and no
special care admissions occurred for any of the neonates involved.
These results are comparable to those of Chan and To, in their
prospective study using low-dose oxytocin, who found that 6%
of the neonates of the study group had Apgar scores less than 7
at one minute, while 100% of the neonates of their study group
had Apgar scores more than 7 at 5 minutes [18]. Also, our results
agree with Merrill and Zaltnik (3.9% of the studied neonates had
Apgar score < 7 at 5 minutes) [19]. Melin et al. [20] have classified
neonatal acidemia according to umbilical artery pH at birth as
mild or pre-acidemia at 7.10 to 7.19, moderate acidemia at 7.00
to 7.09, and severe acidemia at pH less than 7.00. In a similar
context, and for the purpose of prediction of the likelihood of
neonatal encephalopathy, Low et al. [21] have classified neonatal
acidosis, as regards umbilical arterial base deficits, as mild; 4–8
mmol/L, moderate; 8-12mmol/L, and severe acidosis; greater
than 12mmol/L. Accordingly, in the current study, numbers of
neonates with pH<7.1 and those with base deficits>8 mmol/
Litre, were comparable between both groups with no significant
difference (OR=1.261 and 1.455; respectively), while, surprisingly,
the case group showed a significantly lower arterial pH and a
significantly higher arterial base deficit as compared to controls,
which emphasizes the undeniable effect of oxytocin on the arterial
acid-base status but this effect was not enough to increase the risk
of developing neonatal academia, which agrees with Merrill and
Zaltnik in their randomized double masked trial [19]. Also, Thorp
et al. [10] conducted a study on 1423 primigravid women where
43% of them received high-dose oxytocin augmentation and no
significant difference was noticed in mean arterial pH between
oxytocin and no oxytocin groups. Contradictorily, Oscarsson et al.
[16] in their massive retrospective study on 106,755 deliveries,
concluded that oxytocin use increased the risk of low Apgar score
at 5th minute and neonatal special care admission but their study
remains limited by being retrospective and hence subject to recall
bias as well as heterogeneity of population recruited from 10
different hospitals and not considering factors like uterine hyperstimulation.
In the current study, fifteen umbilical artery pH values (20.3%)
of the control group were less than 7.2 which agrees with those of
Akoury et al. [9] (20%) but they have used base deficit of 7mmol/L
as a cut-off to diagnose neonatal acidosis and hence, 29% of cases
and 27% of controls in their study were acidotic. Different modes
of delivery might be another reason for different results.
The fact of occurrence of acidemia in non-augmented labors
was explained by Yoon and Kim who concluded a normal significant
fall in umbilical artery pH and bicarbonate with the presence of
labor and increased duration of second stage of labor in healthy
term neonates [22]. The current study hasn’t considered neonates
with mild acidemia/acidosis as it is thought that mild acidosis
occurs in almost all normal labors [23].
The current study uniquely reported the significant negative
correlation between duration of oxytocin administration among
the case group and umbilical artery pH which signifies the
compromising effect of oxytocin on neonatal circulation studied
by Olofsson et al. [12] and correlates with the duration of use not
only the dose which has been studied in few trials. As oxytocin
impairs the utero-placental and umbilical circulations, there might
be a gradual accumulation of lactates or gradual affection of the
fetal ability to compensate and wash lactates out of the circulation
even in absence of uterine hyper-stimulation.
The limitation of this study is that it hasn’t studied the incidence
of meconium staining at birth and risk of meconium aspiration
as a neonatal outcome. Also, the progress of labor hasn’t been
correlated with the results. Moreover, only low-dose oxytocin was
studied and further studies are needed to evaluate effect of highdose
oxytocin compared to controls and emphasize the effect of
duration of oxytocin use on neonatal outcome with larger number
of patients and correlate it to other neonatal parameters.