Open Access Ophthalmology Journal Juniper Publishers
Abstract
Aims & Objectives: The main objectives of this work are, on the one hand, to know the etiopathogenesis, classification and clinical manifestations of carotid-cavernous fistulas (CCF), as well as to illustrate the radiological findings of this rare pathology that allow establishing diagnostic suspicion, confirming definitively the same or even perform the therapeutic management. To do this, the findings will be reviewed in the following imaging tests: Computed Tomography (CT), Magnetic Resonance Imaging (MRI) and cerebral arteriography.
Material & Methods: In this review, we included the eight patients with confirmed diagnosis of CCF by cerebral arteriography at the P.B.M hospital, Bikaner, Rajasthan in the period between March 2016 and May 2017. The demographic, clinical, etiopathogenic and therapeutic aspects are reviewed, as well as the findings in the different imaging tests that suggest or confirm the diagnosis: CT, MRI and arteriography.
Conclusion: The diagnosis of CCF requires a high degree of clinical suspicion. CT and MRI can suggest the diagnosis and assess unilateral or bilateral ocular involvement (engorgement of the superior ophthalmic vein, thickening of the extraocular muscles and dilatation of the affected cavernous sinus).
Keywords: Carotid; Cavernous; Diagnosis; Treatment; Imaging; MR
Introduction
The CCF is an anomalous communication between the carotid arterial system and the cavernous venous sinuses, either directly or through intradural branches of the external or internal carotid. In this way an anomalous arteriovenous shunt is generated. In general, they are unilateral, although occasionally they can have a bilateral affectation. Therefore, there are two types of CCF: direct, which are High-flow and produced by communication of the internal carotid artery with the cavernous sinus, and indirect, low-flow and in which communication is carried out by vessels dural, the so-called dural fistulas.
In any case, there are other classifications of the CCF. One of the most used is based on angiographic findings, and was described by Barrow. This classification divides the CCF into four types:
a) Type A (direct shunt between the intracavernosal internal carotid artery and the cavernous sinus).
b) Type B (arterio-venous dural fistula from the internal carotid artery).
c) Type C (dural fistula fed by the external carotid artery).
d) Type D (dural fistula fed by both internal and external carotid arteries).
Types B, C and D are considered dural or indirect CCF, and are produced by rupture, usually spontaneous, of small caliber branches of internal or external carotid. More often, they occur in perimenopausal women. Type A or direct fistulas are produced by the rupture of the internal carotid artery inside the cavernous sinus. They are high flow, present a dramatic clinical debut and often occur after trauma or rupture of an intracavernous internal carotid artery aneurysm.
Etiopathogenesis
Regarding etiopathogenesis, CCF can also be classified as spontaneous or traumatic, being the traumatic cause the most frequent, representing approximately 70 to 90% of cases. As we have been previously pointing out, the cause of the direct ones are fundamentally traumas with skull base fracture (traffic accidents are the most frequent traumatic cause, falls and penetrating wounds of the head and orbit are other causes), but also they can occur secondary to surgical procedures (carotid angioplasty procedures, endarterectomy, transsphenoidal hypophysectomy, trigeminal rhizotomies or nasopharyngeal biopsies), rupture of intracavernous aneurysms or collagenopathies. On the other hand, the indirect ones are usually spontaneous and do not have a clear etiological factor, although predisposing factors as diverse as HBP, trauma, intracranial surgery, Valsalva, pregnancy have been associated. Spontaneous CCF's are frequently associated with collagen diseases. In our cases, the most frequent cause of CCF was post-traumatic (five cases), three cases were spontaneous CCF, and one was iatrogenic he symptoms and signs of CCF are related to the size, duration, location, and route of drainage of the CCF. In cases of direct fistulas, they rarely appear in the early post-traumatic period, although large ones may have an acute onset. Typically, the CCF grows and manifests itself in days or weeks. This type of CCF usually causes a more obvious symptomatology. The clinical manifestations of indirect CCF can be very variable, from a mild conjunctival ecchymosis to a severe decrease in visual acuity. These clinical signs and symptoms are not exclusive of direct or indirect CCF, since in both cases the symptomatology varies from being practically imperceptible to causing disabling symptoms.
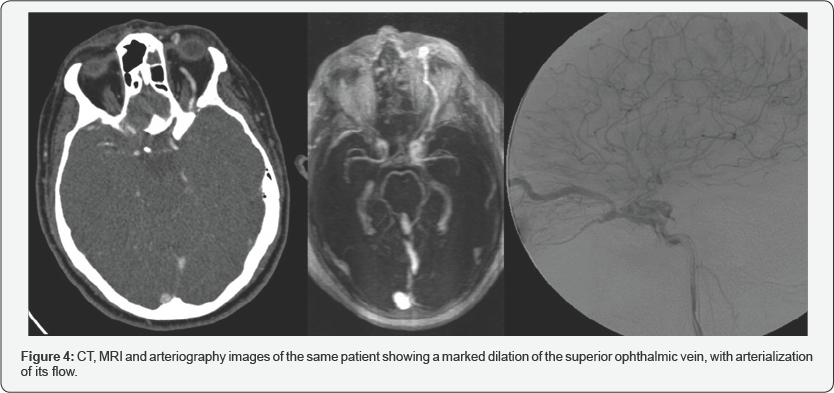
The drainage route can be multidirectional, both in the direct and in the indirect ones: anterior to the venous ophthalmic system (especially superior ophthalmic vein) as in (Figure4), posterior to the petrosal sinuses, lateral to the sphenoparietal sinus, contralateral to the cavernous sinus on the other side, or inferior to the pterygoid plexus. Thus, the manifestations may vary depending on the venous drainage route of the CCF.
The characteristic clinical trial of the CCF is pulsatile exophthalmos, conjunctival chemosis and fronto-orbital murmur (synchronous tinnitus with the pulse), although sometimes a discrete loss of visual acuity or a paralysis of cranial nerves III, IV, V and VI can be the only sign. The worsening of visual acuity occurs in 85 % of cases and vision loss in up to 25 % of patients, with multiple causes of this alteration in visual acuity: glaucoma associated with venous hypertension (increase in IOP), diplopia,proptosis with exposure and edema of the cornea, macular edema, retinopathy or ischemia of the optic nerve. Ptosis and diplopia occur early, with diplopia being the most frequent symptom produced by compression of III nerve.
The physiopathological mechanism of these manifestations is mainly due to the increase in flow that occurs when the arteriovenous communication is formed and which causes an increase in the pressure in the veins draining in this cavernous sinus. In the superior and inferior ophthalmic veins, this pressure increase that hinders normal drainage will cause orbital venous congestion with the appearance of proptosis, palpebral edema, corneal ulcerations, pulsatile exophthalmos with murmur on auscultation, conjunctival chemosis, secondary glaucoma (9 %), and commitment of the retinal perfusion in approximately 30 %. Headache is a very frequent symptom also in patients with CCF.
In large direct CCFs, the arterial steal that occurs can cause retinal hypoperfusion and ischemic neuropathy of optic nerves and cranial nerves III, IV, V and VI, as well as ischemia of large brain territories in patients with poor circulation of the polygon due to arteriosclerosis or by incomplete congenital formation of the circle of Willis.
Material & Methods
In this review, we included the eight patients with confirmed diagnosis of CCF by cerebral arteriography at the P.B.M hospital, Bikaner, Rajasthan in the period between March 2016 and May 2017, after obtaining clearance by the ethical committee attached with the Sardar Patel Medical College, Bikaner. The demographic, clinical, etiopathogenic and therapeutic aspects are reviewed, as well as the findings in the different imaging tests that suggest or confirm the diagnosis: CT, MRI and arteriography.
For this review, the clinical and demographic data of the electronic medical record of each patient have been collected and an attempt has been made to recover the images of the studies carried out from our PACS storage system.
Results

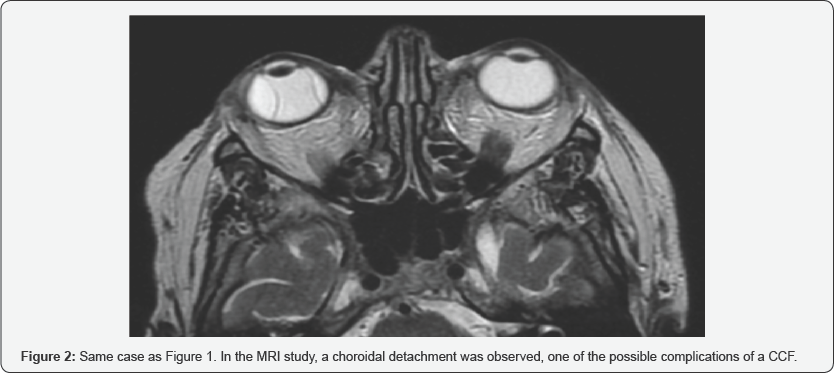
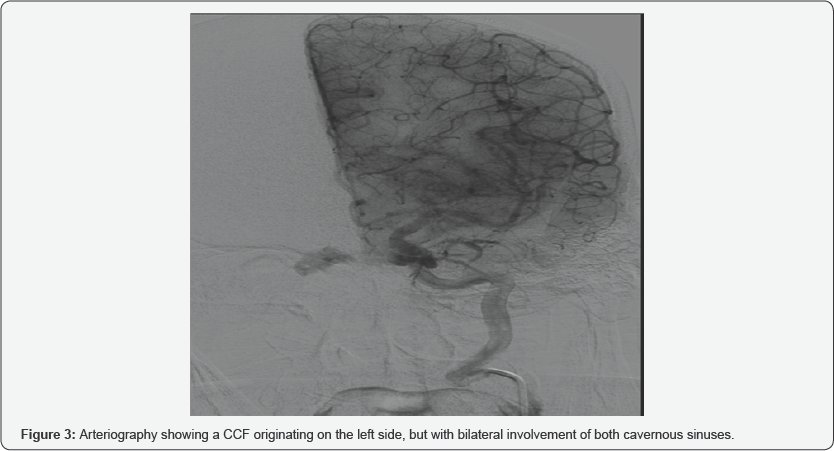
In a period of 1 year between March 2016 and May 2017, eight patients have been diagnosed and treated by CCF in our hospital. Of these eight patients, three were women and five men, with an average age of 52.9 years (range 25-77 years). All the patients in our series had exophthalmos, 62 % also associated diplopia and chemosis, and in 25 % they manifested headache or auscultate fro nto-orbital murmurs (Figure 1). In a patient with loss of visual acuity, a choroidal detachment was observed on MRI, a complication that can be associated with CCF (Figure 2). In 6 patients, the ocular symptoms were unilateral (75%): two patients with involvement of the right cavernous sinus and four patients with left involvement), being bilateral in the two remaining patients (Figure 3) [1-4].
Diagnosis
Only in three of the eight patients diagnosed, CT and MRI were performed before arteriography. The arteriography was performed in all of them and in the eight cases allowed to establish the definitive diagnosis.
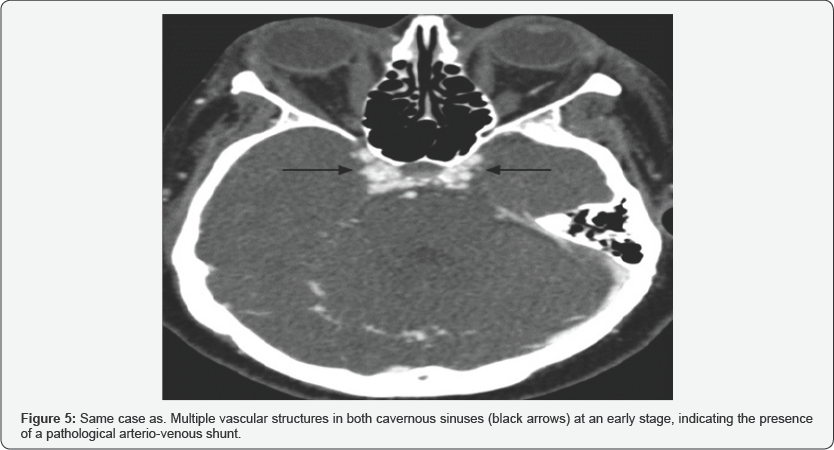
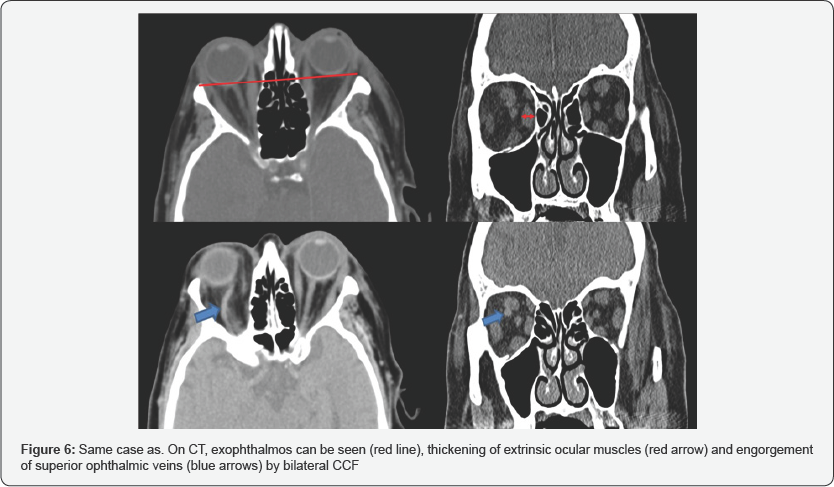
CT is usually the initial test in the CCF study. The study by helical acquisition and 3D post-processing has contributed significantly to the diagnosis of this entity. The findings that we can observe in these studies and that allow us to establish the diagnosis of CCF are fundamentally an enlarged cavernous sinus that enhances asymmetric and early with an early filling of the plexuses, venous sinuses and ophthalmic veins (Figure 5). It also allows the evaluation of orbital signs such as proptosis and thickening of the extraocular musculature (Figure 6), and in cases of direct CCF, of traumatic etiology, it allows to identify the fracture traces in the skull base [5].
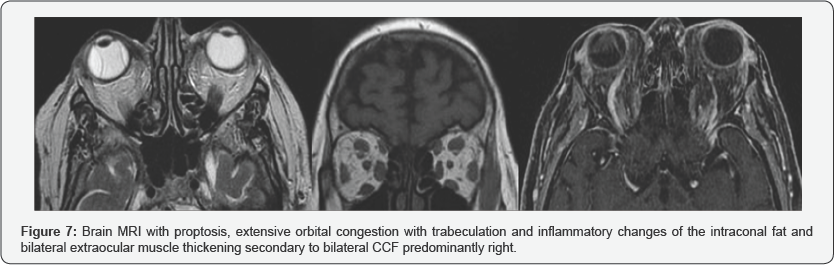
MRI angiography has been shown in several studies to be superior in the diagnosis and study of drainage. Like CT, MRI can also identify all signs of orbital involvement, such as proptosis and thickening of the extraocular musculature (Figure 7), as well as identifying cavernous sinus flow voids, which correspond to the angiographic finding of the contrast fill of the same when the contrast reaches the intracavernosal carotid. However, most authors agree that both CT and MRI cannot replace angiography at the moment of confirming the diagnosis, its classification, assessment of the type of drainage and its possible management [6-8].
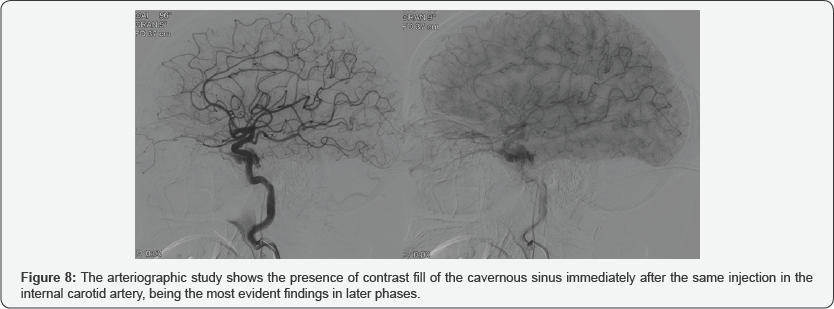
Carotid arteriography is the definitive diagnostic technique. It is the fundamental technique, not only to identify the vascular alteration and classify it, but also to plan the endovascular treatment. Angiography allows to assess the tributary vessels of the fistula, the size and location of the fistula, detect associated carotid aneurysms, classify the fistula as direct or indirect, identify the drainage pathway of the cavernous sinus, detect high-risk hemodynamic alterations such as venous drainage cortical, pseudo aneurysms or varicosities of the cavernous sinus, and identify other associated vascular lesions in posttraumatic cases (Figure 8).
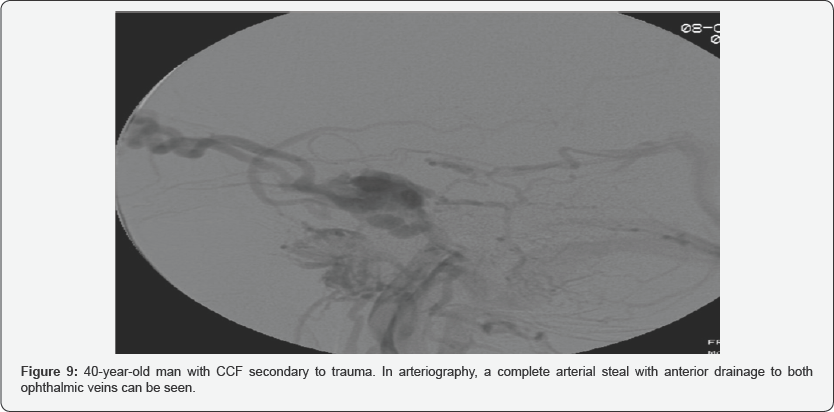
As we have just noted, in the later phase, the CCF drainage route, the direction of venous flow, and the presence of varicose veins in the cavernous sinus can be assessed (Figure 9). Dilatation of the petrosal sinuses and ophthalmic veins provides a mapping for access for transvenous embolization.
Treatment
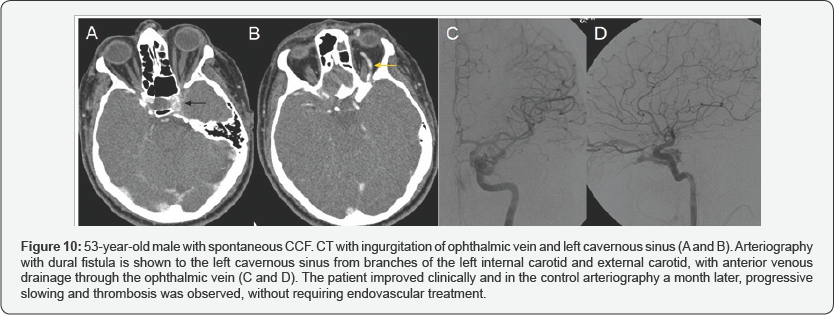
In three patients, spontaneous thrombosis occurred after arteriography was performed (Figure 10). The others required endovascular treatment, without immediate complications after performing the procedures.
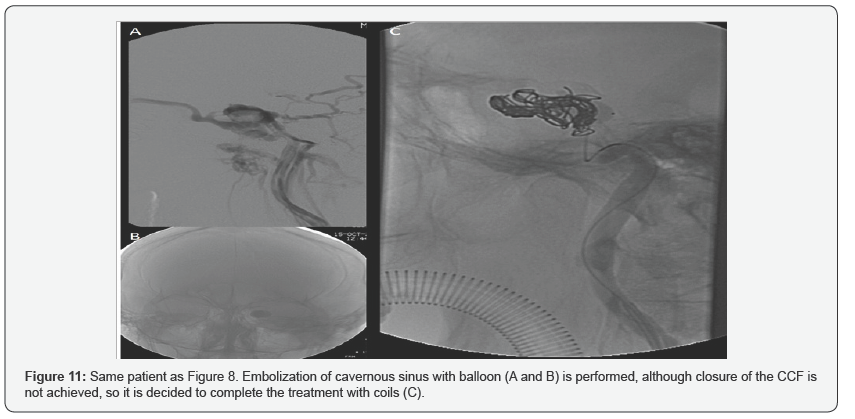
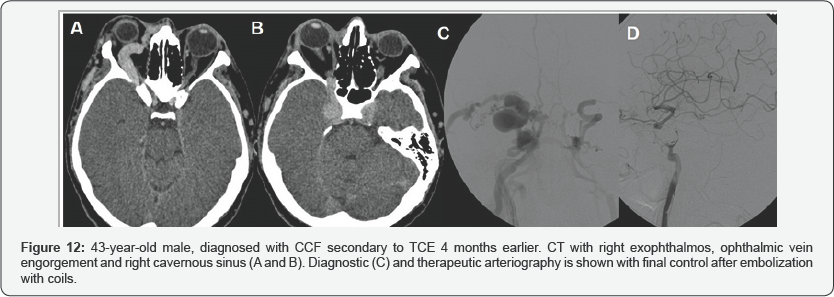
The initial treatment of three patients was balloon occlusion, requiring two of them to be closed with coils in a second time, due to the persistence of low flow CCF. In the two remaining patients, the initial treatment was with coils (Figure 11 & 12).
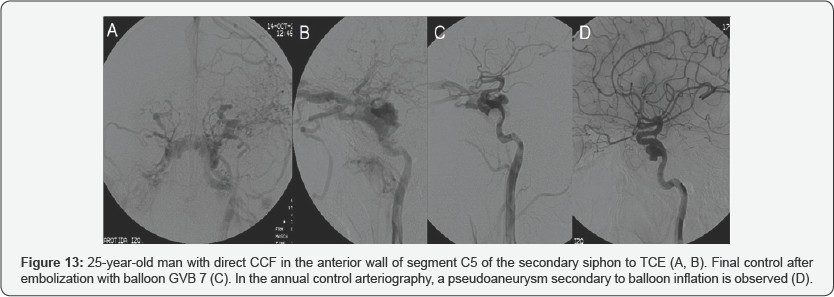
As late complications, it is worth mentioning a patient with persistent CCF after embolization with coils, with a decrease in flow and improvement of ocular symptoms, and another patient with a pseudoaneurysm after balloon embolization, which decreased in arteriography of control performed 12 and 24 months later (Figure 13).
The most established indications for treatment are: diplopia, treatment must be urgent in the following situations: acute glaucoma, intractable pain, marked proptosis and in the case neurological deficits (transient or progressive) intracranial of obstructive venous retinopathy that threatens vision. The hypertension, loss of vision and non-traumatic intracranial hemorrhage, decrease in visual acuity due to ischemia, in relation to intraocular pressure, as well as the presence of papilledema and the appearance of glaucoma.
Indirect, low-flux CCFs spontaneously close between 20 and 50 % of cases. The direct ones rarely close spontaneously and, without treatment, they cause loss of vision in 80-90 % of cases due to occlusion of the central vein of the retina or glaucoma. In addition, dural fistulas are more technically complex when there are multiple arteries feeding, especially when these originate from both carotids, internal and external.
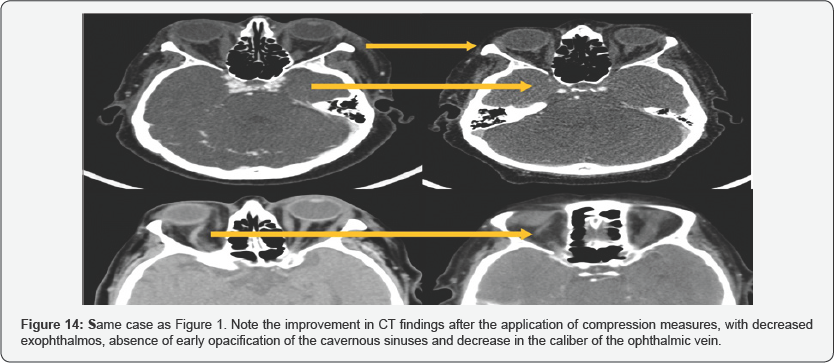
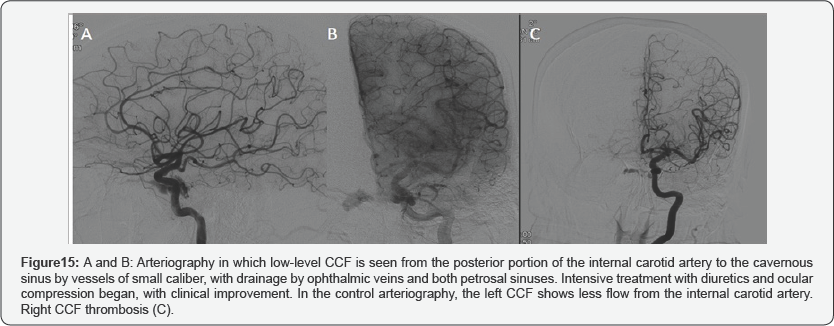
In cases of low-flow fistulas, conservative measures should be the first step of treatment. Measures such as the application of continuous pressure on the affected eyeball can be used to increase venous pressure, impede flow through the CCF and facilitate thrombosis (Figure 14 & 15). Another option used is the application of repeated massages on the internal carotid of the affected side with the contra lateral hand. In this way, if an excessive compression of the carotid is exerted, a cerebral perfusion is produced, with plethora of the contralateral hand. When the hand falls, the flow is restored. This treatment can be effective in very low flow fistulas.
When this type of low-flow fistula requires treatment for symptom progression, due to its bilateral involvement or because it does not respond to conservative treatment, endovascular treatment is the choice, with the transvenous approach with embolization of the cavernous sinus, which presents the best results and for some authors, the approach of choice. Access to the cavernous sinus can retrogradely through the cavernous sinus or anterogradely after surgical exposure of the superior ophthalmic vein.
The treatment of choice for high flow fistulas is currently the transarterial occlusion of the CCF with balloon and / or coils. It is a minimally invasive procedure with a quick recovery time post-procedure and does not require general anesthesia, which achieves 80-90% of therapeutic successes respecting carotid GGS permeability in 80% of cases. If the internal carotid artery cannot be respected and it must be occluded, an occlusion test must be performed previously to confirm that this procedure can be performed.
The materials used for the embolization of the cavernous sinus are the coils and the balloons, with similar results with both materials in the literature. Some authors have used cyanoacrylate (NBCA) combined with coils to completely seal the fistulas.
Although the morbidity derived from these techniques is minimal, the complications of these procedures exist. There is 3% of strokes and permanent neurological defects. Oculomotor paralysis occurs in 20%, and balloon inflation can be a cause of pseudoaneurysms, as occurred in one of our patients. In addition, the treatment can change the hemodynamic conditions of the patient and, as a consequence, cause hemorrhage, cerebral edema or worsening of ocular damage.
In cases where transarterial treatment cannot be performed due to carotid stenosis, tortuosity of the vessels or traumatic occlusion, venous embolization can be performed. The potential complications of this treatment are heavy bleeding due to rupture of the ophthalmic vein, damage to the trochlea or other intraorbital structures or infection. However, these complications are usually caused by attempts to channel thrombosed or nondilated veins. In none of the patients included in this review was the transvenous route used.
Conclusion
The diagnosis of CCF requires a high degree of clinical suspicion. CT and MRI can suggest the diagnosis and assess unilateral or bilateral ocular involvement (engorgement of the superior ophthalmic vein, thickening of the extraocular muscles and dilatation of the affected cavernous sinus). Cerebral arteriography remains the gold standard for the evaluation of patients with CCF, allowing endovascular treatment and performing periodic controls, if percutaneous treatment is not possible.
To Know More About Open Access Ophthalmology
Journal Please Click on:
https://juniperpublishers.com/jojo/index.php
To Know More About Open
Access Journals Publishers Please Click on: Juniper
Publishers



No comments:
Post a Comment