Complementary Medicine & Alternative Healthcare - Juniper Publishers
Abstract
Introduction: This evidence-based review aims to explore the association between vitamin D status and the severity and mortality of COVID-19, providing insights for healthcare professionals and policymakers in managing the disease.
Methods: A systematic review process was conducted to identify relevant studies on vitamin D and COVID-19 using electronic databases and specific search terms. Thirteen studies were selected and analyzed, including quantitative research at levels III, IV, and V.
Results: The analysis revealed a significant association between vitamin D deficiency and increased severity and mortality of COVID-19. Vitamin D levels were found to be inversely related to the severity of the disease, with deficiency acting as an independent predictor of COVID-19-related mortality. Studies demonstrated a higher prevalence of vitamin D deficiency among hospitalized COVID-19 patients. Bolus doses of vitamin D supplementation were associated with improved clinical outcomes and lower mortality rates in COVID-19 patients.
Conclusion: The evidence suggests that maintaining adequate vitamin D levels may have a protective effect against the severity and mortality of COVID-19. Vitamin D supplementation, in combination with safe sun exposure education, could be a cost-effective and safe measure to mitigate the impact of the SARS-CoV-2 pandemic. However, further interventional studies are needed to evaluate the efficacy and optimal dosing regimens of vitamin D supplementation in COVID-19 patients.
Keywords: COVID-19; SARS-CoV-2; vitamin D; Severity; Mortality; Supplementation; Evidence-based practice
Introduction
Coronavirus disease 2019 (COVID-19), declared a global pandemic by the World Health Organization (WHO), presents a significant challenge to healthcare systems worldwide (WHO, 2020) [1]. In January 2022, COVID-19 ranked among the top four leading causes of death for all age groups, with older adults being particularly vulnerable [2]. Hospitalizations and mortality rates are significantly higher in adults over 65 years of age compared to those under 65 [3,4].
Between January 2020 and July 2022, there were over 562 million confirmed cases of COVID-19, resulting in approximately 6.3 million deaths worldwide (WHO, 2022). The economic impact of COVID-19 is staggering, estimated at over $16 trillion, which accounts for approximately 90% of the annual gross domestic product (GDP) of the United States [5].
Vitamin D, a hormone produced by both the kidneys and the skin, plays a crucial role in regulating blood calcium concentration and impacting the immune system. It is known by various names, including calcitriol, ergocalciferol, calcidiol, and cholecalciferol.
The two widely available pharmacologic preparations are cholecalciferol (D3) and ergocalciferol (D2). More recently, vitamin D has shown antiviral effects and plays a crucial role in the immune system [6-8]. It is being investigated for its potential in mitigating infections, enhancing immune responses, and suppressing the cytokine storm [9-11] Comparatively, vitamin D deficiency has been linked to increased susceptibility to viral infections. Research has not demonstrated a strong association between vitamin D levels and the prevention of COVID-19 infection [12-15]. However, there is a growing interest in exploring the potential role of vitamin D in relation to the severity of COVID-19 disease.
At the time of submission, COVID-19 has tragically resulted in the loss of over 6 million lives globally (WHO, 2022). Despite this significant impact, there remains limited knowledge about potential protective factors against the disease. Notably, advanced age and underlying chronic medical conditions, especially chronic pulmonary and cardiac diseases, have emerged as prominent predisposing factors for severe COVID-19 development and subsequent mortality [16,17]. This comprehensive literature appraisal aims to investigate potential associations between vitamin D status and disease severity and survival in COVID-19 patients. By analyzing the available evidence, this analysis provides a recommendation while considering the balance of benefit, harm, and cost.
Methods
This systematic review, conducted in collaboration with a faculty advisor and university librarian, examines the relationship between vitamin D and COVID-19, focusing on severity and mortality outcomes. The review process involved comprehensive searches of electronic databases, including PubMed, using key terms such as Vitamin D, Vitamin D Level, Vitamin D Deficiency, Covid, Covid-19, and Coronavirus. Inclusion criteria were limited to English-language articles published between 2020 and 2022, and excluded research proposals and protocols. A total of 20 articles were retrieved, and after reviewing the title and abstracts, 13 relevant studies were selected for appraisal using the Johns Hopkins Appraisal Tool. The levels of evidence were graded using Johns Hopkins Level of Evidence table. This review is comprised of 11 non experimental level III research articles, the highest level of evidence available to date.
Literature Review
Vitamin D levels have been found to be notably depleted among the aging population, a group that exhibits heightened vulnerability to COVID-19 [15]. Further evidence highlights the prevalence of vitamin D deficiency among hospitalized COVID-19 patients, with 59% of admitted individuals presenting vitamin D insufficiency. Vitamin Ds deficiency upon admission has demonstrated a significant association with COVID-19 severity and mortality, even after adjusting for factors such as age, gender, and comorbidity.
There is possibly a blood level dependent association between vitamin D level and COVID-19 severity. A retrospective multicentric study of 212 patients [7] found that critical COVID-19 cases had the lowest levels of vitamin D, whereas mild cases had the highest levels. Similarly, found similar results when stratifying COVID-19 patients by vitamin D level. There were two additional studies conducted by that reported weaker correlations between vitamin D levels and COVID-19 cases and mortality. Finally, there is a small body of evidence supporting the use of bolus doses of vitamin D3 supplementation administered during or shortly before the onset of COVID-19 (2020) [9] and Karahan and Katkat (2021) [5] both demonstrated a lower incidence of COVID-19 infection and improvement in COVID-19 severity with bolus dosed vitamin D.
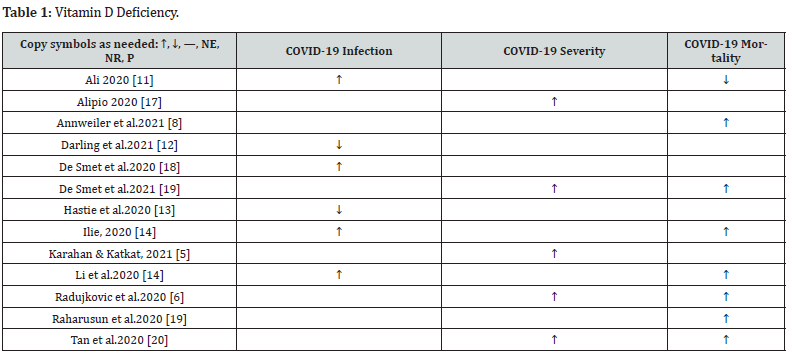
There were a few studies that failed to demonstrate a positive effect of vitamin D on COVID-19. These studies were small, completed on a younger and healthier population, and primarily studied the relationship between vitamin D level and COVID-19 infection rates, but did not study the correlation between the vitamin D level and COVID-19 severity or mortality (Table 1).
Discussion
In response to the profound burden imposed by the COVID-19 pandemic and the potential for mitigating severe disease outcomes through the exploration of protective factors, numerous researchers have established a compelling association between vitamin D deficiency and the severity of COVID-19 [18-21]. While research has failed to demonstrate that Vitamin D prevents Covid-19 infection, there is a moderate amount of research establishing that optimal vitamin D levels are associated with less severe cases of COVID-19 and conversely, low vitamin D levels have been associated with more severe cases. Furthermore, bolus dosing Vitamin D3 may provide some protection in the severity of the infection, particularly in populations at risk [22,23].
Implications for Practice
Nurse practitioners manage patients in primary care who are at risk of COVID-19. Staying up to date with the current evidence is crucial in supporting clinical practice. The evidence appraised in this review are all non-experimental research. Observational and cohort studies provide valuable insights into potential associations, and the majority of the reviewed studies indicate a positive correlation between vitamin D levels and COVID-19 outcomes. Moreover, vitamin D supplementation is generally considered safe when administered within the recommended dosage range. Although further experimental research is needed to establish a causal relationship, considering the low risk profile of vitamin D supplementation, it is the recommendation of the authors that nurse practitioners consider prescribing Vitamin D supplementation to improve the severity of COVID-19 infections and that blood levels should be monitored to achieve optimal circulating levels ranging from 75 to 100 nmol/L. As healthcare leaders, nurse practitioners have the responsibility to actively seek opportunities to educate both patients and colleagues. By doing so, we can drive practice change and promote the adoption of evidence-based approaches. Disseminating evidence-based practices is vital in improving patient outcomes and ultimately enhancing the overall quality of care.
To Know more about Journal of Complementary Medicine & Alternative Healthcare
To Know more about our Juniper Publishers





No comments:
Post a Comment