Case Studies - Juniper Publishers
Abstract
Background: Craniotomy is a type of surgical procedure to open the cranium to access the brain for surgical repair, and any damage to brain parts or alteration in brain function. The brain surgery is generally the first step of treatment for brain injuries and conditions. The aim of the study was early inpatient physiotherapy to improve the functional outcomes in post craniotomy patient. Functional independence measure (FIM) was the outcome scale that was used to see the progress level of the patient. The patient’s score varies from 18 points (the patient is completely dependent) to 126 points (the patient is completely independent). Derivatives of the FIM score include, FIM gain where it is the difference between discharge and admission FIM and measures absolute functional gain. FIM efficiency is the FIM gain divided by the length of stay in rehabilitation and measures the rate of functional improvement.
Case Description: A 9-year-old child admitted after a traumatic brain injury with subdural hematoma on 9th November 2017, he underwent craniotomy on 11/11/2017. His GCS level was E2V2M3 and RLA was 2 on 12/11/2017. The child had left hemopneumothorax as associated complication. Intervention done was positioning, chest care, tilt table, activities in bed, balancing, standing and walking. FIM on admission and discharge was taken. Patient was discharged on 2/3/18.
Result: The Absolute FIM gain was calculated where Discharge – Admission; 90-18= 72 and FIM efficiency was calculated where FIM gain /by length of stay i.e., 72/90 *100=80% rate of functional improvement.
Keywords: Craniotomy; FIM; Exercise protocol; Physiotherapy intervention
Background
Craniotomy is a type of surgical procedure to open the cranium to access the brain for surgical repair, and any damage to brain parts or alteration in brain function. The brain surgery is generally the first step of treatment for brain injuries and conditions. The common indications of craniotomy are Brain tumours, Cranial abscess, Cerebral oedema, Haemorrhage, Traumatic brain injury like Stroke, Aneurysm, skull fractures [1].
The postoperative period is the first part of the journey of care but, as reported by SASM, this is perceived to be an area where the need for guidance is a supreme priority to prevent complications like pain, Deep vein thrombosis, Respiratory problems due to surgery, Pressure sore, Decrease range of motion, Muscle contractures, Hypotension [2]. There may well be a “Platinum 24 Hours” (maximum 48 hours) after surgery when patients are subjected to complications and decision making is very important with the help of clinical data that is presented and treatment options that are available [3]. Inpatient physiotherapy refers to early, all stages of recovery and it begins when the patient’s emergence from anaesthesia and continues through the time required for the acute effect of anaesthetic and treatment procedures to subside. The main aim of inpatient physiotherapy is to prevent complication due to immobilization and to make the patient to achieve basic level of energy so that the functional skills are improved and retained [4]. It helps to promote return to functional levels, prevent respiratory complication, increase muscle strength and endurance, and encourage early mobility to prevent DVT, prevent bed sores, and prevent contractures. Functional independence measure (FIM) was the outcome scale that was used to see the prognosis level of the patient. Admission and discharge functional status were measured in the areas of self-care, mobility, locomotion, sphincter control, communication, and social cognition to know the level of disability [5]. As there is increase in incidence in patient undergoing brain surgery (craniotomy) early prevention of post-surgical complications and improving functional status can reduce the morbidity further reduces the length of hospital stay by giving early Inpatient physiotherapy.
Aim
Role of early inpatient physiotherapy to improve the functional outcomes in post craniotomy patient.
Case Description
A 9-year-old child admitted after a traumatic brain injury with subdural hematoma on 9th November 2017, he underwent craniotomy on 11/11/2017. His GCS level was E2V2M3 and RLA was 2 on 12/11/2017. FIM on admission and discharge was taken. The child had right hemopneumothorax as associated complication. Patient was discharged on 2/3/18. The patient’s score varies from 18 points (the patient is completely dependent) to 126 points (the patient is completely independent). Derivatives of the FIM score include, FIM gain where it is the difference between discharge and admission FIM and measures absolute functional gain. FIM efficiency is the FIM gain divided by the length of stay in rehabilitation and measures the rate of functional improvement.
Intervention
Overall treatment duration was 30mins with total frequency was 2 sessions in a day for 2weeks which was for 1 hour per Session from the post operative day to discharge day. FIM is administered on admission and discharge patient from ward (from post operative day to discharged day). The materials used are tilt table, knee brace, Incentive spirometer, crape bandage, wheel chair, walker and pillows.
a) Positioning Advice: Optimal positioning with pillows to minimize the pressure on body surface to avoid pressure sores. Positions was done with Elevation of bed up to 30 degrees to decrease ICP for (head ace), Limb elevation up to 75 degrees for 20mins with compression stockings improve circulation.
b) Tilt table: Tilt table treatment included upper limb exercises, and breathing exercises. It is a padded table with a footplate and three large Velcro straps, the patient lies on top of the table on his back. To secure the patient safety strap are strapped, and then slowly the table is elevated to 30 degrees for 10mins followed by constant monitoring and later to 70 degree for 5mins and once the vitals are stable the patient is elevated into a standing position for 20mins with constant monitoring of blood pressure and heart rate throughout the treatment.
c) Respiratory therapy: Postural drainage technique was used for 15mins depending on the lobe that was affected to prevent secretion accumulation. Incentive spirometer was used once the patient is weaned from ventilator as feedback and to gain confidence for 10 counts with rest period for every 3 counts. Thoracic expansion exercise, Diaphragmatic breathing, breathing re-education was demonstrated and practiced about 10 cycles with rest period and was instructed to do 2 hourly. This will help patient to maintain saturation level and decrease breathlessness.
d) Activities in the bed: Passive movements of upper limb and lower limb in various planes of motion for 15mins 10 repetition with 5min rest period twice a day was given to patient. Segmental rolling, Bridging (unilateral and bilateral), Pelvic rotation (hip, knee flexion) was taught and practised for 10 counts with rest period of 2mins for every 3 counts. Active movements were started once the manual muscle testing of muscle reach grade 3 which includes exercise like Scapular movement, Extension /abduction movement of arm and fingers and touching the opposite shoulder.
e) Activities out of the bed: Patient was made from Supine to sitting progressed to weight bearing activities, shoulder shrugs, hitching and hiking, knee extension, overhead activities static and dynamic strengthening exercise. Once the Sitting balance was achieved the patient was made to Stand with maximal support and progressed to independent standing by the time of discharge.
f) Ambulation: Wheelchair was used initially to get oriented to environment and surroundings, progressed to support standing and later to support waking.
g) Balance training: Static balancing exercise like shifting weight to both lower limbs, step stance training, Perturbation, trunk movements was done for 10mins with rest period with gait belt as assistive device. Dynamic balancing exercise like reaching activities, one leg standing, throwing activities was practiced. Patient was trained from sitting without support till standing independently.
h) Handgrip exercises: Exercise like reach, grasp, releasing objects were taught with different shapes object like glass, spoon, plate so that eating component is trained and patient can become independent functionally.
Overall Intensity: The program consists of 1 hour, for 2-week, therapist-assisted sessions (Figure 1-4).
Results
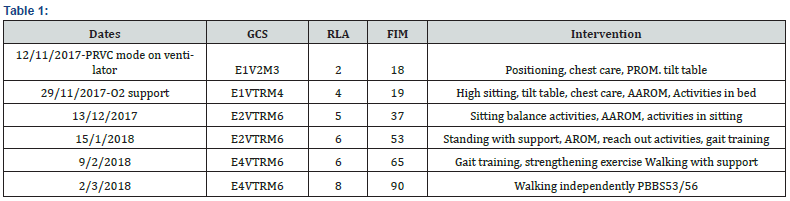
a) Absolute FIM gain: Discharge – Admission=90-18= 72.
b) FIM efficiency =FIM gain /by length of stay 72/90 *100=80% rate of functional improvement.
Discussion
Through physical stimulation, the residual neurons provide the foundation for creating new function-restoring neuronal networks. It is an “if-you-don’t-use-it-you-lose-it” system, in which paralysis-associated disuse of muscles over time results in viscous-circle. Inpatient physiotherapy is given to patient based on functional gain. (self-care, dressing, feeding, bathing, mobility, sphincter, communication). Home programme is planned to maintain the functions that are gained and improve the in patient’s social life. Do and Don’ts after craniotomy like lifting heavy weights, strenuous aerobic exercise, treadmill, cycling are explained to the patients. The program is distinguished by its intensity, continuity, and personalization [6]. Body weight supported ambulation is given for some patients depending on GCS with help of assistive device. The program believes weight bearing is essential to recovery for function because that is what the human body was designed for. The FIM is a sensitive functional status instrument that assesses the degree of dependence of rehabilitation patients. It is a good indicator to know level of burden of care and to evaluate changes during inpatients rehabilitation. Two important components are assessed; FIM gain which is the difference between discharge and admission FIM. FIM efficiency which is based on FIM gain divided by the length of stay in rehabilitation [7]. A tilt table serves as an integral part of physical therapy by providing early mobilization for patients who are too weak to stand on their own. Tilt tables are used to reintroduce patients to the vertical position. The most common reasons for inclusion of tilt table treatment are to facilitate weight bearing, prevent muscle contractures, to prevent blood clots, to prevent pulmonary embolism, improve lower limb strength and increase arousal and prevent other bed rest complication for the hospitalized patient [8,9]. Optimal positioning after surgery is first step to minimize the potential risk of abnormal amounts of pressure on relatively small parts of the body surface like occipital and heel. Positioning helps to preserve joint integrity and protect skin from breakdown due to prolonged pressure [10]. The brain controls breathing and since surgery carries with it some risk of respiratory complications it is important as a physical therapist to prevent further complication by chest manipulations [11]. Activities in the bed and passive movements in various planes of motion is integral part of therapy to reactivate and reorganize the nervous system. Brain surgery has the potential to affect a patient’s static and dynamic balance where physical therapy focused on the patent’s balancing exercise for ambulation and better functional outcomes [12]. Based on Functional Independence Scale handgrip exercises is a key element for FIM gain which decrease the dependency [13]. Thus, very few case studies were attempted on ‘Role of inpatient physiotherapy on functional outcomes in patients with post craniotomy’ to check FIM gain and FIM efficiency.
Conclusion
Early physiotherapy rehabilitation is one of the most important aspects of rehabilitation in craniotomy patients. This case report proves that functional independence is the main outcome for the patients as well as for medical and paramedical team to know the level of progress. Here by inpatient rehabilitation after 24 hrs of post craniotomy is ideal for making the patient functionally independent. This study further recommends doing RCT on patient with post craniotomy.
To Know More About Juniper Online Journal of Case Studies Please click on:
For more Open Access Journals in Juniper Publishers please click on:





No comments:
Post a Comment