Anesthesia & Intensive Care Medicine - Juniper Publishers
Abstract
Introduction: The Auto-Transfusion Tourniquet (A-TT®) shifts the blood from the legs to the central circulation and blocks its return to the legs. The use of the A-TT has previously been shown to be effective during CPR and was shown in a pig study [1] to increase systolic and diastolic blood pressures, coronary perfusion pressure, cerebral perfusion and end-tidal PCO2. The present study was done to assess if using the A-TT as part of CPR protocol in pre-hospital cardiac arrest patients treated by a team of 4 caregivers interferes with the quality parameters of the CPR.
Methods: Twenty-six cardiac arrest scenarios were performed by teams of 4 paramedics-in-training where half [13] were done in the standard way and in 13 A-TT devices were applied on both legs of the training mannequin. CPR continuity, time to onset of CPR, time to first defibrillation, time to first dose of adrenaline, time to first and subsequent changes of massagers and A-TT application timing and duration were measured.
Results: in all scenarios randomized to A-TT use, it was applied correctly by one person with no difficulty. There were no statistically significant differences between the measured quality parameters of the A-TT vs. No-A-TT scenarios.
Conclusion: Placing A-TT on the legs during cardiac arrest managed by a team of 4 caregivers does not interfere with the quality of the delivered CPR.
Keywords:Cardiac Arrest; Paramedic Training; Cardiopulmonary Resuscitation; CPR Quality
Introduction
The outcome of CPR performed in order to treat patients in out-of-hospital cardiac arrest (CA) continues to be low when the AHA protocol is used (2; 3). While Return of Spontaneous Circulation (ROSC) upon hospital arrival is achievable in over 1/3rd of witnessed CA patients undergoing by-stander CPR and administration of adrenaline by paramedics, the ultimate outcome of hospital discharge in acceptable neurological functionality is very poor (~2%). The neurological outcome when adrenaline is not used is not different (~2%), despite a 70% lesser rate of ROSC upon ED arrival. It is suspected that adrenaline administration during CPR contributes to the poor neurological outcome due to constriction of the cerebral circulation leading to further diminished O2 supply to the brain [3].
In recent studies a novel exsanguination tourniquet device (Auto-Transfusion Tourniquet (A-TT®), “Hema Shock”, Oneg Ha Karmel Ltd. Tirat Carmel, Israel) has been shown to displace over 1000 cc of blood from the legs to the central circulation while blocking the re-entry of the blood into the legs [4]. The A-TT consists of two elastic rings, each wrapped by an elastic sleeve and pull-straps with handles (Figure 1a-b). The A-TT is vacuum-packed in a durable pouch. To apply, the patient’s shoes are removed, but not the pants. The A-TT is then placed on the toes and the ring is rolled up over the foot, the heel and up the leg all the way to the groin area by pulling the handles and straps along the axis of the limb. The A-TT is first placed on one leg and then, in cardiac arrest, immediately on the other. Upon achieving steady ROSC, the A-TT is removed by manually rolling it down the leg in short steps of 20-25 cm at a time. Vital signs should be monitored in each step.
Applying the A-TT caused increase in systolic and diastolic blood pressures in normal volunteers [4], increase in coronary perfusion pressure (CPP), cerebral blood flow (CBF), and end-tidal CO2 (ETCO2) in cardiac arrest pigs undergoing CPR with A-TT on all 4 legs [1]. There were no negative effects on gas exchange or on biochemical markers. In another study in volunteers, it was found that in addition to increased blood pressures, there was also higher cardiac output and stroke volume when A-TT was placed on both legs [5]. In another series [6] A-TT induced ROSC in 7 of 10 terminal cardiac arrest cases arrived at the emergency department after prolonged out-of-hospital CPR by paramedics. 5 of them survived ICU care and one was discharged with fully preserved mental/cognitive functions.

The study reported here was performed in anticipation of a wider clinical use of A-TT as part of CPR protocol by paramedics in pre-hospital cardiac arrest. We tested if field application of A-TT by a team of 4 paramedics-in-training performing CPR has any negative effect on the standard parameters of CPR quality [7]. We tested if A-TT application causes delays in onset of CPR chest compressions, onset of defibrillations in scenarios where the rhythm was shockable, onset of Epi administration or increased number of >10 sec pauses of chest compressions. We also measured the time it took to apply A-TT on both legs. The quality parameters values were compared to the no-A-TT scenarios and to accepted standards of care [8].
Methods
The study was approved by MDA's research committee. Paramedics-in-training who participated in the study first received a lecture on the physiology and clinical use of the A-TT in cardiac arrest and severe shock, signed a participation consent form and practiced applying the A-TT on a mannequin leg under supervision. The participants were then divided into teams of 4 paramedics-in-training of mixed gender. Every team performed 4 CPR scenarios lasting 10 minutes each. Each scenario started with a brief description of the patient’s whereabout and status, a quick evaluation of vital signs followed by immediate initiation of manual chest compressions of the training mannequin paced by a metronome. In each scenario one of the team members acted as a team leader, another one was assigned to apply the A-TT and the other two alternated giving CPR, starting IV and preparing and administering medications.
A-TT was applied in two of the four scenarios performed by each team, selected by the moderator in a random order. (Figure 2a) shows the application of an A-TT on a limb and (Figure 2b) shows a photograph of the A-TT when up on both legs.
During each scenario we monitored and documented the standard parameters of CPR quality [7,8]:
1. Time to onset of CPR chest compressions
2. Time to first and subsequent defibrillations
3. Time to first and subsequent doses of adrenaline
4. Time to onset of A-TT placement (in scenarios where A-TT was indicated)
5. Duration of A-TT placement (from onset of placement on first leg to completion of second leg)
6. Number and duration of chest-compressions interruptions for more than 10 sec. for any reason.
The data were tabulated in excel which was used for descriptive statistics (mean +/- SD). Comparison between yes-A-TT and no-A-TT scenarios was done using Student’s t-test with two tails assumption. P < 0.05 was considered statistically significant.
Results
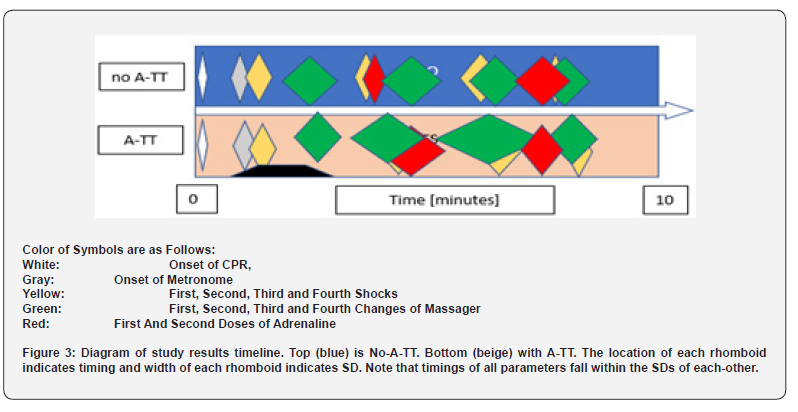
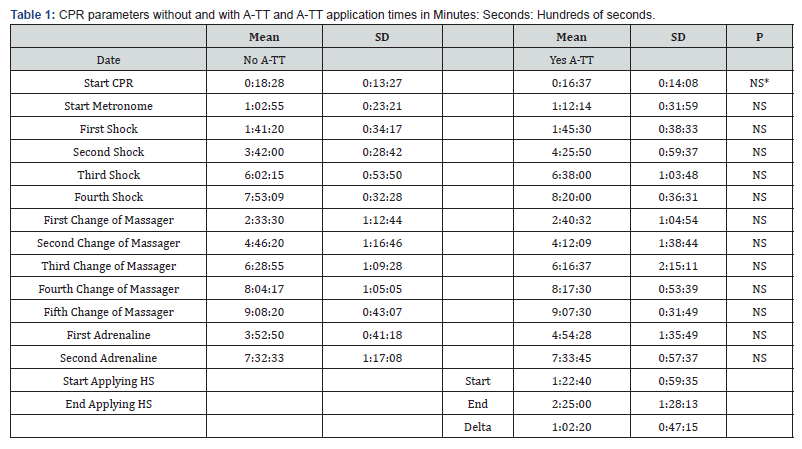
Twenty-six scenarios were performed by the teams, where 13 scenarios were done with A-TT and 13 without. CPR was started within 18.3 +/- 13.3 sec (mean +/- SD) from the onset sign in the no-A-TT scenarios and within 16.4 +/- 14.1 sec in the yes-A-TT scenarios (NS – not a statistically significant difference). (Table 1). In two cases more than 60 sec elapsed from the beginning of the scenario until chest compressions were started: one case with NO-A-TT and one case with A-TT. Time to first cardioversion was 101.2 +/- 34.2 sec in the NO-A-TT scenarios and 105.3 +/- 38.3 sec in the A-TT scenarios (NS). Time interval to first change of massagers was 2:33 +/- 1:12 min in the NO-A-TT scenarios and 2:44 +/- 1:06 min in the A-TT scenarios (NS). Time interval to first IV Epi injection was 3:52 +/- 0:41 min in the NO-A-TT scenarios and 4:44 +/- 1:33 min in the A-TT scenarios (NS). See (Table 1) and (Figure 3) for details.
CPR Quality
There was a total of 6 interruptions of CPR chest compressions that lasted more than 10 sec in 5 of the No-A-TT scenarios (in one scenario there were two interruptions) and 2 CPR interruptions for >10 sec in the A-TT scenarios, both occurring in a single scenario (NS).
A-TT Placement
A-TT was successfully placed by a single paramedic-in-training in all the scenarios that were randomized to A-TT placement. The A-TT placement started 82.4 +/- 59.4 sec after the onset of the scenario and application to both legs was completed 145.0 +/- 68.1 sec after scene arrival. The mean placement duration was 62.2 +/- 47.2 sec (range 30-180 sec) with all but two placements taking less than 60 sec. A-TT placement occurred before first massager replacement in 9 scenarios, before the second replacement in 3 scenarios and before third massager replacement in 1 scenario. All the participants rated the A-TT placement as “Easy”.
Discussion
The purpose of this study is to address a concern that the use of the Auto-Transfusion Tourniquet (A-TT) during performance of CPR in out-of-hospital cardiac arrest may interfere with the quality of CPR. The current AHA directive for high quality CPR requires early onset of uninterrupted and effective chest compressions, early defibrillation if rhythm is shockable, repeated in intervals if ROSC was not achieved, and quick administration of epinephrine with repeated doses in intervals [7,8]. It is now standard to monitor administration of CPR during training and in practice to assess the quality of the care and correct it when needed. As such, this study addresses the question: Does the use of A-TT during CPR interfere with its quality? To do so, we conducted CPR drills with and without application of the A-TT, while measuring the quality parameters. This prospective, non-blind controlled study was performed by trainees in MDA’s paramedics course and their trainers during Q1 2023. The paramedics-in-training were half-way of their course and have all performed CPR drills beforehand.
The physiological rationale for using A-TT during CPR consists of the following factors:
1. Rolling the A-TT on each leg pushes >500 cc of the patient’s own fresh blood to the core and >1000 cc from both legs [4]. In fact, it is postulated that during cardiac arrest the blood volume in the legs vessels is even higher due to the paralysis of the sympathetic nervous system during cardiac arrest, thereby significantly increasing the squeezable blood quantity relative the amount in normal adults. This shift of blood to the central circulation increases the end-diastolic volume of the heart chambers thereby amplifying the effectiveness of chest-compressions and the resulting stroke-volume [5].
2. The positioning of the A-TT ring in the upper thigh blocks the flow of blood into the legs. [The legs blood supply in a normal adult is approximately 24% of the total cardiac output [9]. As a result, the entire CPR-induced cardiac output is distributed to the essential organs (brain, heart, liver, gut, and kidneys) and is not “wasted” to perfuse the legs which can withstand 2 hours of ischemia with no risk of damage [10-12]. If simple arithmetic is used, this increases the share of the CPR cardiac output to the core from 75% to 100% or by approximately 25/75=0.33.
3. The blocking of blood-flow into the legs substantially increases the total vascular peripheral resistance. Therefore, the blood pressure during diastole, which is very low during CPR, increases substantially causing a major rise in coronary perfusion pressure (CPP). It was shown in a porcine study [1] that CPP nearly doubled when A-TTs were applied to the 4 legs of the experimental animals during induced cardiac arrest. Given the fact that most coronary perfusions are diastolic, having a sufficient level of CPP is critical for cardiac O2 supply and the likelihood of successful cardioversion.
4. The application of A-TT is quick, can be done by a single person with minimal training and does not interfere with other treatments given to the patient around his/her upper body (e.g. CPR, insertion of lines, intubation etc.). When ECMO is used as part of CPR [13], A-TT may facilitate cannula placement by increasing large vessels volume and diameter and increase the ECMO rate of suctioning the blood into the oxygenator for the same reason and by prevention of blood vessels flutter. Care must be taken to leave enough space for the sterile insertion of the cannulas.
5. The A-TT completely constricts the blood vessels of the legs. As such, it is an ultimate mechanical vasoconstrictor matching or surpassing the effect of adrenaline on the periphery without any detrimental effect on brain blood supply [14]. It is hypothesized that the use of A-TT in CPR may be able to eliminate the need for adrenaline with similar outcome on ROSC and better cognitive outcome when it is used instead of adrenaline. This hypothesis needs to be tested in prospective clinical studies.
Discussion of the Results of this Study
In all the categories of the CPR quality parameters, no statistically significant differences were observed when A-TT was used compared to when A-TT was not used. Onset of CPR, timing of massager replacement, time of first and subsequent shocks, first and subsequent Epi and the number of CPR interruptions were not statistically different between the scenarios with and without applying A-TT. In the A-TT scenarios the rings were applied approximately 82 seconds after arrival and the application took 62 sec, where all but two applications took less than 60 sec with the shortest application done in 30 seconds and the longest 3 min (Table 1). There were no difficulties in applying the A-TT in any of the scenarios and the paramedics-in-training did so without a problem after a brief practical training on a mannequin leg. The paramedics-in-training consisted of both males and females in equal numbers and there was no advantage to physical strength or body mass in achieving successful applications.
Study limitations
This study was done in teams of 4 paramedics-in-training and its results are only applicable to the situations where 4 or more providers are available on the scene. The number of scenarios with and without A-TT was 13 in each. This number is relatively small but there were no trends in the measured valued that could have become significant had the groups been bigger except, perhaps, the timing of first epi that was 52 sec longer at 4:44 min vs. 3:52 min (p = 0.078) when A-TT was used. Clearly, additional evaluations can and should be done in real-life cases of cardio-pulmonary resuscitations.
Applicability to Clinical use and Conclusions
We conclude that applying A-TT during CPR administered by a team of 4 trained persons does not impose a detrimental interference on the quality of CPR. Other safety and effectiveness aspects of A-TT use in CPR should be studied in real-life cases.
To Know more about Journal of Anesthesia & Intensive Care Medicine
Click here: https://juniperpublishers.com/jaicm/index.php
To Know more about our Juniper Publishers
Click here: https://juniperpublishers.com/index.php





No comments:
Post a Comment