Anesthesia & Intensive Care Medicine - Juniper Publishers
Abstract
Introduction: A significant number of men with benign prostatic hyperplasia (BPH) will require surgical therapy. The technique of photo-selective vaporization of the prostate (PVP), using the Greenlight laser™, is one of the most employed procedures to treat BPH. A frequent complication among patients undergoing surgery is intraoperative hypothermia (body temperature < 36.0°C). The aim of the current study was to determine if warming the irrigation and the intravenous (IV) fluids can mitigate hypothermia during PVP surgery.
Methods: This was a prospective, single blind controlled trial, which included participants scheduled for PVP surgery because of BPH. The patients were randomized to four treatment groups:
(1) Warm irrigation fluid and IV fluid.
(2) Warm irrigation fluid and IV fluids at room temperature.
(3) Irrigation fluid at room temperature and warm IV fluids.
(4) Irrigation fluid and IV fluid at room temperature.
The patient's body temperature was taken upon entering the operating room and subsequently every thirty minutes throughout the surgery.
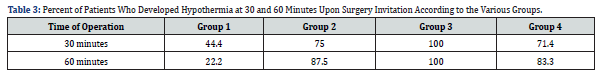
Results: 29 patients were included in the study. Thirty and 60 minutes after the surgery began, 44.4% and 22.2% of the patients in group 1 developed hypothermia whereas 75.0% and 87.5%, 100.0% and 100.0% and 71.4% and 83.3% of the patients in groups 2, 3 and 4 developed hypothermia. However, there was no significant difference between the groups (p=0.236 and p=0.212, respectively).
Conclusion: The data pointed out that the use of both warmed IV and irrigation fluids could prevent the development of hypothermia during surgery.
Key words: Benign Prostatic Hyperplasia; Photo Selective Vaporization of the Prostate; Intraoperative Hypothermia; Warm Irrigation Fluids; Warm Intravenous Fluids
Introduction
Among aging men, clinical benign prostatic hyperplasia (BPH) is a prevalent condition, often resulting in lower urinary tract symptoms (LUTS) [1]. Studies show that as many as 50% of men over the age of 50 and 80% of those over 80, suffer from LUTS due to BPH [2]. LUTS is characterized by a range of symptoms, such as an urgent need to urinate, nocturia, frequent urination, dysuria, trouble fully emptying the bladder, difficulty starting urination and experiencing a weak or broken stream during urination [3]. Pharmacology treatments, such as alpha-adrenergic antagonists, beta-adrenergic agonists, and 5-alpha-reductase inhibitors, are often used as a first line standard of care in those patients. Nevertheless, a significant number of men experience a progression in their condition that requires the subsequent step of surgical therapy. For many years, the surgical standard for treating BPH has been either transurethral resection of the prostate (TURP) or open prostatectomy (OP).
However, both TURP and OP are followed with sets of challenges of intraoperative and postoperative complications. These may include bleeding, the need for intervention due to clot retention, genitourinary infections, fluid absorption, and TURP syndrome [4]. Not only that, but many of these patients might also be managing heart disease with anticoagulants or coping with other comorbidities, such as hypertension, kidney insufficiency, or diabetes mellitus which could increase the chances of developing complications. Moreover, especially in elderly patients or those dealing with multiple health issues, these procedures may lead to a decrease in quality of life. Thus, alternative procedures that are less invasive than TURP and OP might offer a safer treatment option for such patients. The technique of photo-selective vaporization of the prostate (PVP), using the GreenLight laser™ (GLL), is one of the most employed procedures.
It has been demonstrated that the GreenLight laser™ is an efficacious solution for managing LUTS because of BPH, with a notable safety profile, particularly in men who are on anticoagulants and have an increased risk of bleeding. Moreover, PVP offers added benefits including cost-effectiveness due to shorter duration of catheter use and length of hospitalization [5]. A frequent complication among patients undergoing surgery is intraoperative hypothermia, which is characterized by a core body temperature dropping below 36.0°C during the operation [6]. Initiation of either general or neuraxial anesthesia leads to vasodilation, facilitating the transfer of heat from the body's core to its peripheral regions. Such heat redistribution is the predominant factor for hypothermia within the initial hour of anesthesia, even when patients are actively being warmed. Furthermore, it can result in severe complications such as coagulopathy, potential myocardial issues, and surgical wound infections. Additionally, hypothermia can delay drug metabolism, extend recovery periods, and cause the patient to feel uncomfortably cold [7].
PVP surgery is carried out under general anesthesia, using physiological irrigation solutions (0.9% saline) at room temperature. Although the utilization of an isothermal solution lowers the risk of hypothermia, it does not eliminate its possibility. Numerous studies have demonstrated that employing warm intravenous (IV) or irrigation fluid can help in maintaining body temperature. In addition, it was found that warm IV irrigation fluid during surgery could minimize cardiovascular complications [8]. However, currently, to the best of our knowledge, there's no standard practice of combining warm IV and irrigation fluids administered during a PVP surgery to avoid hypothermia. In our research, we aimed to determine if warming both the irrigation and the IV fluids can mitigate the risk of developing hypothermia during PVP surgery.
Methods
The Research took place at Shamir Hospital in Israel during the years 02.2020-02.2023 upon approval of the institutional ethical committee (0050-20-ASF). All patients have signed an informed consent prior to surgery.
Study Design
This was a prospective, single blind controlled trial, which included male participants aged 50 and above, all scheduled for PVP surgery because of BPH. Patients who underwent any previous or alternate prostate surgeries or prostate embolization were excluded from the study. The patients were randomized to four treatment groups:
(1) Warm irrigation fluid and warm IV fluid (in both, heating chamber temperature was 38.5°).
(2) Warm irrigation fluid (heating chamber temperature was 38.5°) and IV fluids at room temperature
(3) Irrigation fluid at room temperature and warm IV fluids (heating chamber temperature was 38.5°).
(4) Irrigation fluid and IV fluid at room temperature. The irrigation fluid was administered using an orthopedic pump maintaining a pressure of 150 ml/min. The patient's body temperature was taken upon entering the operating room and subsequently every thirty minutes throughout the surgery. In addition, details about the patients' age, comorbidities, prostatic size, and laser time were collected.
Statistical Analysis
Analysis was conducted using IBM SPSS Statistics version 29.0. Descriptive statistics were performed mainly with medians and rates, and non-parametric tests were performed. Comparing continuous variables (age, prostate size, treatment time, duration of operation, body temperature and hemoglobin levels) between the treatment groups was performed using Kruskal–Wallis H one-way ANOVA with Bonferroni correction, as appropriate, categorical variables (background diseases and hypothermia rates) were analyzed using Chi-square test. Boxplot diagrams were used for descriptive demonstration of the distributions. Pearson correlation coefficient was performed to estimate the correlation between prostate size and laser time. Differences were considered statistically significant at p value of < 0.05.
Results
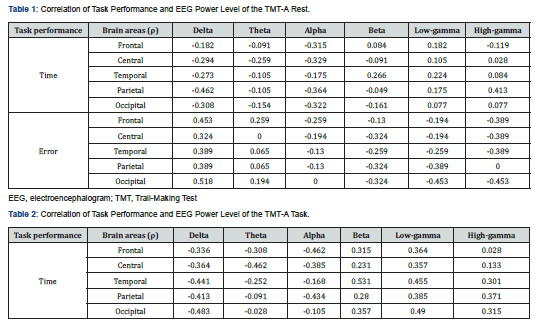
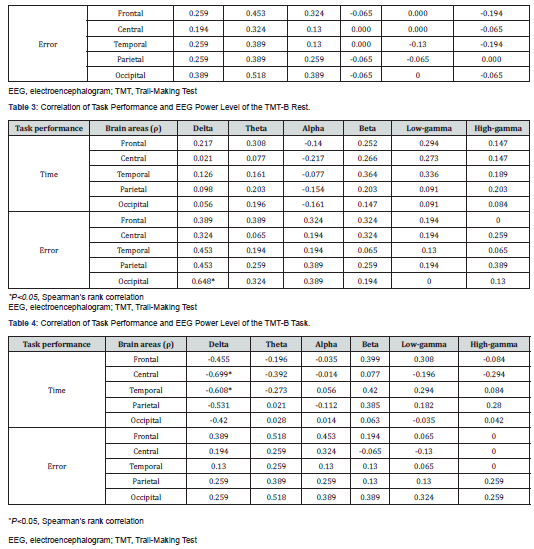
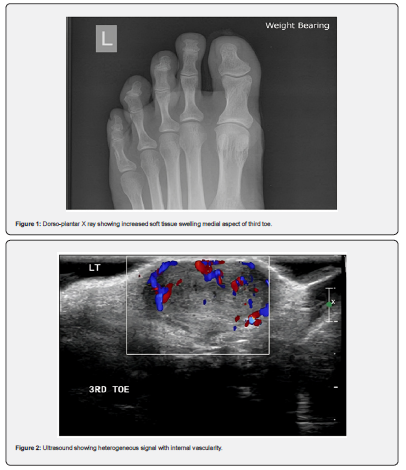
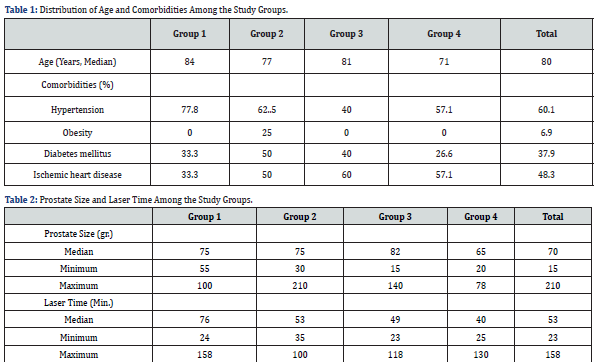
During a period of 2 years only 29 patients were included in the study. The median age was 80.0 years (range 52-92) with no difference between the groups. Most of the patients suffered from hypertension (60.1%). Details about age and comorbidities distribution among the various study groups are presented in (Table 1). Median prostate size was 70.00 gr. (range 15-210), and median laser time was 53 minutes (range 23–158) (Table 2). The Pearson correlation test revealed a week trend of relationship between prostate size (mean: 77.8 gr) and laser time (mean: 63.7 minutes) (p=0.051, r=0.373).
The presence in the operating room varied from 1 to 3 hours. Since it is not possible to compare the decrease in body temperature between a patient who stayed in the operating room for an hour and a patient who stayed for 3 hours, a comparison was made between the patients during their first hour in the operating room. Thirty minutes after the surgery begun, 44.4% of the patients in group 1 (Warm irrigation and IV fluid) developed hypothermia whereas 75.0%, 100.0% and 71.4% of the patients in groups 2 (Warm irrigation fluid), 3 (Warm IV fluids) and 4 (Irrigation and IV fluid at room temperature) respectively, developed hypothermia. Interestingly, after one hour, only 22.2% of patients from group 1 presented hypothermia and 87.5%, 100.0% and 83.3% of the patients in groups 2, 3 and 4 respectively, developed hypothermia (Table 3). Nevertheless, due to small numbers, Chi-square tests showed no significant difference between the groups regarding hypothermia.
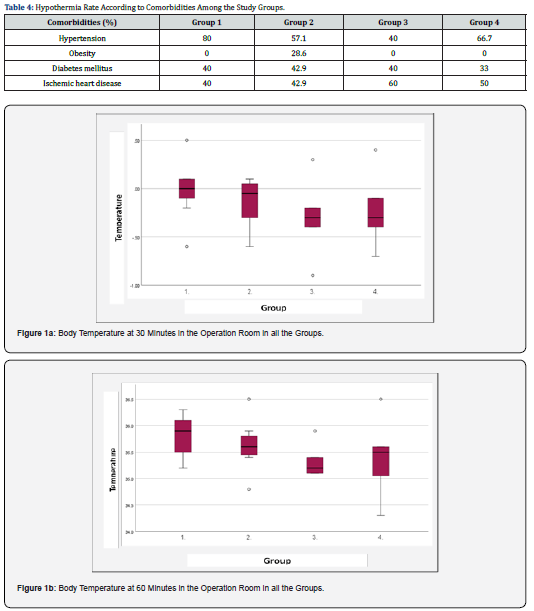
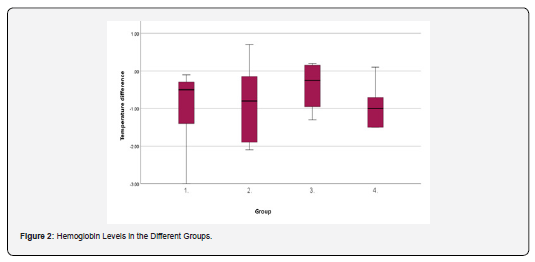
The lowest temperature measured at 30 and 60 minutes of surgical time was observed in group 3 (warm IV fluids) while the highest was demonstrated among group 1 (Warm irrigation and IV fluid) (Figure 1a and 1b). However, independent samples of the Kruskal-Walli’s test revealed no significant difference between the groups (p=0.236 and p=0.212, respectively). Hemoglobin levels were measured before the surgery (upon admission) and before discharge (about 24 hours after surgery). The difference between the first and the second measurements was -0.5 in group 1 (Warm irrigation and IV fluid), -0.8 in group 2 (Warm irrigation fluid), -0.3 in group 3 (Warm IV fluids) and -1.0 in group 4 (irrigation and IV fluid at room temperature) (Figure 2). Independent samples Kruskal-Wallis Test revealed no significant difference between the groups (p=0.621). As for the relation between the comorbidities and hypothermia, patients with obesity, diabetes mellitus and ischemic heart disease demonstrated hypothermia upon 1 hour in the operating room (a drop in temperature below 36.00C), however Chi-square test revealed no statistical significance. In groups 1 (warm irrigation and IV fluid), 2 (warm irrigation fluid) and 4 (irrigation and IV fluid at room temperature), most of the patients who presented with hypothermia also suffered from hypertension (80%, 57.1% and 66.7%, respectively), while in group 3 (warm IV fluids) 60% of the patients who developed hypothermia suffered from ischemic heart disease. (Table 4).
Discussion
Body temperature is one of the most important vital signs, as it ensures the proper functioning of cellular and molecular processes in mammals. The regulation of body temperature, or thermal homeostasis, hinges on a delicate equilibrium between the generation and loss of heat. Yet, during the operation period, this balance can be unsettled by the effects of anesthesia, surgical procedures, and low surgery room temperature, making unintentional hypothermia occur frequently among patients under anesthetic and surgical procedures. When patients undergo general anesthesia, not only does inadvertent perioperative hypothermia represent a decrease in body temperature, but it also poses a risk as an adverse event that can negatively impact the intra- and post-operative outcome. This can result in a range of consequences, from uncomfortable shivering to serious complications such as infections, increased bleeding, prolonged recovery times, and even severe cardiovascular events. It is critical to monitor the core temperature of these patients and to implement active warming procedures from the pre-induction phase through to the recovery period [9].
In this study, we utilized the PVP surgical model, a technique frequently employed in today's urologic surgeries. The PVP procedure is executed with the patient under general anesthesia, employing room temperature physiological irrigation solutions (0.9% saline). The study included 4 treatment arms: warm irrigation and warm IV fluids; warm irrigation fluids and IV fluids at room temperature; irrigation fluid at room temperature and warm IV fluids; and irrigation fluid and IV fluid at room temperature. Our results show that at 30 and 60 minutes through the operation less patients who were treated with warm irrigation fluid and warm IV fluids, developed hypothermia compared to the other groups. In addition, the highest body temperature was observed between 30 and 60 minutes through the operation among patients who were treated with warm irrigation fluid and warm IV fluids than the other groups. Yet, most probably due to a small cohort size, the results did not reach statistical significance. Nevertheless, the current study demonstrated that warm irrigation and IV fluids at one hour into the operation could serve as a modification to prevent the development of hypothermia.
In the past, attempts have already been made to test the effectiveness of heating IV or irrigation fluids to prevent the development of hypothermia during surgery. The effects of warmed IV fluids on body temperature were examined by 105 patients who underwent TURP surgery. Body temperature was significantly higher in patients who received warmed IV fluids compared to the control group which was treated using a cotton blanket. A meta-analysis was conducted to exhibit the effect of warmed bladder irrigation fluid on the development of hypothermia in patients with BPH treated by various surgical procedures. Data collected from a total of 28 clinical studies with 3858 patients revealed that the group treated with room-temperature irrigation fluid resulted in a greater dropped body temperature compared to the warm irrigation fluid group [10]. An interesting meta-analysis was published by Campbell et al., who collected data from 17 studies that examined the effect of warming IV and from 5 studies in which irrigation was used to prevent hypothermia during surgery in adults and compared between the results. Although the collected data was of moderate quality, it demonstrated that warm IV fluids kept the body temperature about half a degree warmer than that of participants who were treated with room temperature IV fluids. No statistically significant difference was reported in the body temperature between patients treated with warm and room temperature irrigation fluids [11].
Most of the published studies dealing with the use of warmed IV fluids or warmed irrigation fluids to prevent hypothermia, do not compare the two treatment arms. Nevertheless, the only study we found that investigated the effect of using warm IV fluids together with warm irrigation fluid on body temperature was conducted by Okeke et al. In this study, 120 patients with obstructing BPH who were about to undergo TURP were randomly divided into 3 groups; patients treated with irrigation and IV fluids at room temperature, patients treated with warmed irrigation fluids at 38°C administered along with IV fluids at room temperature and patients treated with warmed irrigation fluid and IV fluids at 38°C. It was found that there was no significant change in the mean body temperature among patients treated with both warm IV and irrigation fluids than that observed in the groups that were treated with only warm IV or only warm irrigation fluids [12]. Our study is not without limitations. The main limitation of our study is the small sample size. Also, the older age of our patients could be a risk of bias distressing the effect of the treatment arms on the body temperature. Thus, larger studies with a higher sample size and a wider age range should be conducted to evaluate the effect of warming IV and the irrigation fluids on body temperature during surgery.
Conclusion
The data from our study pointed out that the use of both warmed IV and irrigation fluids could prevent the development of hypothermia during surgery. However, wider studies should be performed to establish this finding.
To Know more about Journal of Anesthesia & Intensive Care Medicine
Click here: https://juniperpublishers.com/jaicm/index.php
To Know more about our Juniper Publishers
Click here: https://juniperpublishers.com/index.php