Journal of Surgery- Juniper Publishers
Abstract
Gallbladder disease is a condition that affects nearly 20% of adults in the United States. Roughly 20% of them will develop symptoms throughout their lives; the risk of cholecystitis increases with age and sex, being females in a higher-risk population with a female-to-male ratio of 4:1. An early cholecystectomy is the best choice to treat gallbladder disease. However, it is imperative to determine the best surgical approach based on the risks and benefits for the patient. This comparative review addresses the clinical relevance of gallbladder surgery by examining the diverse indications considering factors such as the severity of the condition, patient preferences, and surgeon experience. The choice between procedures has significant implications for patient outcomes, recovery time, healthcare costs, and sustainability. Robust evidence supports laparoscopic cholecystectomy due to its efficacy and lower risk for the patient. The purpose of this article is to review the current and most relevant concepts in comparing laparoscopic versus open gallbladder surgery, its indications, technique, and complications.
Keywords: Bladder Surgery; Cholecystectomy; Laparoscopy; Laparotomy; Minimally Invasive Surgery
Abbreviations: GD: Gallbladder disease; GB: Gallbladder; GS: Gallstones; CBD: Common bile duct; CT: Computed Tomography; MRI: Magnetic Resonance Imaging; LFTs: Liver function tests; LC: Laparoscopic cholecystectomy; OS: Open surgery; AC: Acute cholecystitis; ECC: Early cholecystectomy; SIS: Surgical Indications for Surgery; PVS: Percutaneous or endoscopic gallbladder drainage; SSI: Surgical Site Infection; IV: Intravenous; PCS: Postcholecystectomy syndrome; CO: Carbon monoxide; PG: Patient group; TE: Technical factors; WR: Wound-related complications; BI: Bile duct injury; RCBDS: Retained common bile duct stones; PH: Postoperative pain; RH: Respiratory complications; TRH: Trocar site hernias; ER: Early recovery; HS: Hospital stay
Introduction
Gallbladder disease encompasses a range of disorders affecting the gallbladder, including gallstones, cholecystitis, and biliary dyskinesia. It has a higher incidence in specific populations, particularly individuals over 40, women, and those with obesity. Clinical features include severe abdominal pain, nausea, vomiting, and jaundice. The diagnosis typically involves imaging studies such as ultrasound, CT scans, MRI, and liver function tests. Treatment options depend on the specific condition and can range from lifestyle modifications and medications to surgical interventions, with cholecystectomy being the most common and practical approach to managing gallbladder disease. Early diagnosis and appropriate treatment are crucial to prevent complications and improve patients’ quality of life [1,2]. Gallbladder surgery, or cholecystectomy, is a standard surgical procedure to treat various gallbladder-related disorders. This review article delves into the indications for gallbladder surgery and offers an in-depth analysis of the two primary surgical approaches, laparotomy and laparoscopy. We aim to comprehensively understand the clinical considerations when deciding between these surgical methods [2,3]. With an increasing number of gallbladder surgeries performed annually worldwide, there is a growing demand for a comprehensive evaluation of the indications and surgical techniques employed [4,5].
This comparative review addresses the clinical relevance of gallbladder surgery by examining the diverse indications considering factors such as the severity of the condition, patient preferences, and surgeon experience. The choice between laparotomy and laparoscopy (minimally invasive surgery) has significant implications for patient outcomes, recovery time, and healthcare costs. Thus, understanding these surgical approaches’ merits and drawbacks is pivotal for patients and healthcare providers [6]. This review will discuss the specific indications for gallbladder surgery, encompassing acute and chronic gallbladder diseases. Additionally, we will present a detailed comparison of the laparotomy and laparoscopy techniques, including their respective procedural aspects, advantages, and limitations. By synthesizing current evidence and clinical insights, this article offers guidance for optimizing patient care and surgical decisionmaking in the context of gallbladder surgery.
Gallbladder Surgery by Laparotomy
Procedure and Technique
Surgical and Endoscopic Approaches for Gallstone Diseases
When managing gallstone diseases, various surgical and endoscopic procedures are available. Laparotomy is a conventional surgical technique used to treat these diseases, involving an abdominal incision to access the gallbladder and address gallstone-related complications [7,8]. On the other hand, for cholelithiasis complicated by choledocholithiasis (the presence of stones in the bile duct), the choice between one-session and two-session treatments depends on multiple factors. One-session treatment, often performed endoscopically, offers benefits such as shorter hospital stays and cost-effectiveness [9]. This minimally invasive endoscopic approach involves the insertion of specialized instruments and a camera through small incisions to visualize, diagnose, and remove gallstones from the bile duct.
Timing of Cholecystectomy in Acute Cholecystitis
Acute cholecystitis commonly results from gallstone blockage in the cystic duct and primarily necessitates cholecystectomy as the standard treatment [7]. The debate revolves around the timing of this surgical procedure. Early laparoscopic cholecystectomy is increasingly favored over delayed cholecystectomy due to several advantages. It offers a higher quality of life, reduced morbidity rates, and cost savings within the hospital [9]. This technique entails making small incisions in the abdomen and inserting a laparoscope, allowing the surgeon to view and remove the gallbladder. The choice of timing, whether early or delayed, should be personalized, considering the patient’s clinical condition and the available hospital resources [9].
Management of Acute Cholecystitis
Acute cholecystitis is a severe condition associated with gallstones, with an approximate 3% mortality rate that escalates with patient age and comorbidities [7]. The gold standard for treating acute cholecystitis is early laparoscopic cholecystectomy, accompanied by the appropriate administration of fluids, electrolytes, and antibiotics [8]. However, alternative techniques like gallbladder drainage are considered for patients with high operational risks. This drainage can be accomplished through percutaneous or endoscopic methods and has demonstrated clinical success in most cases [9]. These approaches use specialized instruments to access the gallbladder or bile ducts through minimally invasive means. After recovery from acute cholecystitis, patients who have undergone drainage may contemplate cholecystectomy as a definitive treatment. Nonetheless, in elderly patients or those with significant comorbidities, the risks associated with cholecystectomy may still be high, making alternative techniques such as gallstone removal through a percutaneous tract or endoscopy more appropriate [9].
Complications of Open Cholecystectomy
Open cholecystectomy is performed when the laparoscopic critical view of safety cannot be achieved for suspected or confirmed gallbladder malignancy or patient clinical condition prohibiting a laparoscopic approach. The complication rates associated with open cholecystectomy are higher than a laparoscopic cholecystectomy [10]. The incisional site required for an open cholecystectomy is more significant than in laparoscopic surgery, resulting in a higher incidence of incisional hernia formation, adhesion formation, wound infection, hematoma, and postoperative pain [11,12].
i. Hernia formation: Incisional hernia formation is a relatively common complication of abdominal surgery, ranging from 2-20%, and is likely multifactorial and dependent on patient and technical factors [13]. Risk factors include wound infection, connective tissue disorders, and surgical technique [14,15]. Incisional hernias are more common in open abdominal surgery than in minimally invasive surgical techniques [16,19,27]. Open cholecystectomy is associated with a higher risk of Incisional hernia than laparoscopic cholecystectomy [11,17,28]. However, single-incision laparoscopic cholecystectomy is associated with a higher prevalence (4.5%) of Hernia formation compared to open (1.5%) [18,29].
ii. Adhesions: Postoperative adhesion formation is a common complication of intra-abdominal surgeries with a prevalence of over 50% [19]. Adhesion formation involves a complex immune response of cytokines, cellular growth factors, cellular adhesion molecules, neuropeptides, and other growth factors released around the surgical trauma site and are influenced by surgical technique [20]. Open cholecystectomy results in more tissue trauma and an increased inflammatory reaction [21,26]. Laparoscopic cholecystectomy results in less abdominal tissue trauma than open and is associated with less inflammatory reaction and less adhesion formation than open cholecystectomy [20,23].
iii. Postoperative Pain: The traditional incision used for an open cholecystectomy is a right subcostal or Kocher incision. This incision is made 2 centimeters below the right costal margin and extends from the midline laterally to the desired length, usually across the rectus muscle [13]. A complication of the Kocher incision, commonly used in open cholecystectomy, is the development of chronic postoperative pain and paresthesia inferior to the scar, typically due to the division of the ninth intercostal nerve [14,15,24].
iv. Surgical Site Infection: Surgical Site infections (SSI) are the most common healthcare-associated infections [16]. SSIs depend on patient and technical factors such as surgical approach [25]. Open cholecystectomy has been consistently associated with a higher risk of SSI compared to laparoscopic [18-20].
Gallbladder Surgery by Laparoscopy
Procedure and Technique
Laparoscopic cholecystectomy is an innovative and minimally invasive surgical technique designed to address gallbladderrelated ailments effectively. This procedure finds its application in the treatment of a spectrum of conditions, including cholecystitis (both acute and chronic), symptomatic cholelithiasis, biliary dyskinesia, acalculous cholecystitis, gallstone pancreatitis, and gallbladder masses or polyps [30]. To execute this intricate procedure, a specialized set of equipment is meticulously employed, comprising two laparoscopic monitors, a laparoscope equipped with a camera cord and light source, a carbon dioxide source with tubing for insufflation, trocars ranging from 5 mm to 12 mm, an assortment of laparoscopic instruments (such as atraumatic graspers, Maryland graspers, clip applier, electrocautery, and a retrieval bag), a scalpel with an 11/15 blade, forceps, needle driver, and absorbable sutures [22-29].
The laparoscopic cholecystectomy unfolds following anesthesia induction and intubation. It commences with the insufflation of the abdominal cavity to 15 mmHg, employing carbon dioxide. Subsequently, four small incisions are made at strategic points in the abdomen for trocar placement: one above the umbilicus, one below the xiphoid process, and two along the right subcostal region. Utilizing a laparoscope and specialized long instruments, the gallbladder is gently retracted over the liver, allowing for clear visualization of the hepatocystic triangle. The procedure requires meticulous dissection to achieve the critical view of safety, defined by three key criteria: the clearance of fibrous and fatty tissue from the hepatocystic triangle, the presence of only two tubular structures entering the base of the gallbladder, and the separation of the lower third of the gallbladder from the liver to visualize the cystic plate. Once this view is satisfactorily attained, the surgeon can confidently isolate the cystic duct and cystic artery, carefully clipping and transecting both structures. The gallbladder is then meticulously separated from the liver bed using electrocautery or a harmonic scalpel. Hemostasis is ensured after reducing the abdominal insufflation pressure to 8 mmHg for 2 minutes. The extracted gallbladder is placed in a specimen pouch and removed from the abdomen, and all trocars are extracted under direct visualization [30].
The benefits of laparoscopic cholecystectomy are numerous and significant. Patients who undergo this procedure experience less pain, a reduced risk of complications, and a swiffer recovery, enabling a quicker return to their regular activities. Furthermore, the incisions are smaller, resulting in less noticeable wounds and scars. In addition, blood loss during surgery is notably lower compared to traditional methods, and hospital stays tend to be shorter, providing patients with a more efficient and less disruptive recovery process [31,32].
Complications
Laparoscopic cholecystectomy, a minimally invasive surgical procedure to remove the gallbladder, is generally considered a safe and effective treatment for gallbladder-related conditions. However, complications can still arise, including wound infection, bleeding, bile duct injury, retained common bile duct stones, and postcholecystectomy syndrome (PCS) [33]. Wound infection is one of the most common early complications following laparoscopic cholecystectomy. This complication typically manifests as pain, redness, and discharge at the incision sites, posing discomfort to the patient. The risk of infection is often mitigated through strict adherence to aseptic techniques and careful wound care postsurgery [33,34].
Bleeding can occur during the procedure or afterward, leading to the formation of hematomas or collections of blood at the surgical sites. Although bleeding complications are relatively rare, they can delay wound healing and cause discomfort. Close monitoring and prompt management are essential to address this issue [35]. One of the more severe complications is bile duct injury, which may occur during the gallbladder dissection from the liver. Injury to the common bile duct or its branches can lead to bile leakage, scarring, or stricture formation, resulting in symptoms such as jaundice, abdominal pain, or cholangitis. Repairing such injuries often necessitates specialized surgical interventions [35]. Another potential complication is the retention of common bile duct stones, which may inadvertently remain in the bile duct after gallbladder removal. These retained stones can cause recurrent symptoms, including pain, jaundice, or infection. They may require endoscopic procedures or further surgery for removal [33,36].
Post-cholecystectomy syndrome (PCS) is a long-term complication characterized by gastrointestinal symptoms, including abdominal pain, bloating, diarrhea, and dyspepsia. It can persist or develop following gallbladder removal, and its exact etiology is not entirely understood. Management may involve dietary modifications, medications, or further evaluation to rule out other gastrointestinal disorders [33,37].
It is important to emphasize that while complications associated with laparoscopic cholecystectomy can occur, the overall incidence remains relatively low. The risk of these complications varies based on factors such as patient characteristics, surgical technique, and the surgical team’s experience. Clinicians must maintain vigilance in recognizing and managing these complications when they do occur to ensure optimal patient outcomes (Table 1).
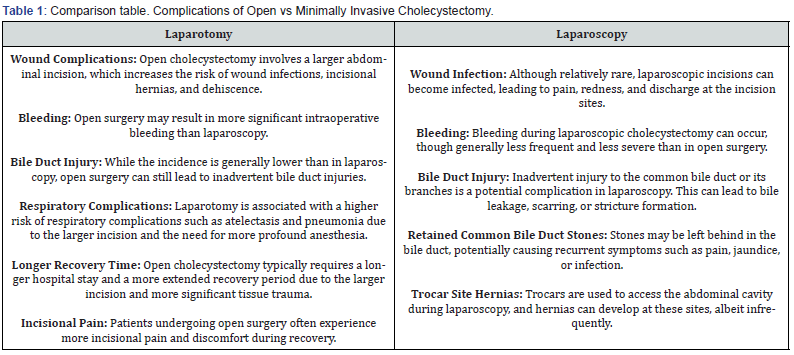
It is important to note that laparoscopic cholecystectomy is generally associated with fewer complications, a shorter hospital stay, and faster recovery than open surgery. The choice between these approaches is often based on the patient’s medical condition, surgeon’s expertise, and other factors. The risk of complications can also vary depending on the patient’s health status and the complexity of the surgery [38-40].
Conclusion
Gallbladder disease encompasses various disorders, predominantly affecting those over 40, women, and individuals with obesity. Diagnosis involves imaging and liver function tests. Treatment options range from lifestyle changes to cholecystectomy. This article discusses laparotomy and endoscopic approaches, emphasizing the advantages of endoscopy, particularly for complex cases. It promotes early laparoscopic cholecystectomy in acute cholecystitis and underscores personalized care. It outlines the benefits of laparoscopic cholecystectomy, including shorter hospital stays and quicker recovery. This article recognizes the higher complication rates associated with open cholecystectomy and elaborates on complications such as incisional hernias, adhesions, postoperative pain, and surgical site infections. It acknowledges the relevance of alternative techniques. Complications following laparoscopic cholecystectomy, including wound infections, bleeding, bile duct injuries, and postcholecystectomy syndrome, are emphasized, highlighting the importance of prompt recognition and management for favorable patient outcomes. Lastly, the article underscores the significance of personalized care and surgical technique selection for gallstone diseases. It emphasizes the benefits of minimally invasive laparoscopic cholecystectomy and the importance of recognizing and managing complications for positive patient outcomes.
To Know more about Open Access Journal of Surgery
To Know more about our Juniper Publishers




No comments:
Post a Comment