Endocrinology and Thyroid Research - Juniper Publishers
Abstract
Background: Graves’ disease (GD) and Hashimoto thyroiditis (HT) are autoimmune thyroid diseases. Around 20% of patients with GD develop spontaneously Hashimoto hypothyroid, contrarily, with less frequency occurred that a patient with HT became hyperthyroid during its clinical course. In the present case, a patient shows spontaneous oscillations of her thyroid function over a period of 21 years.
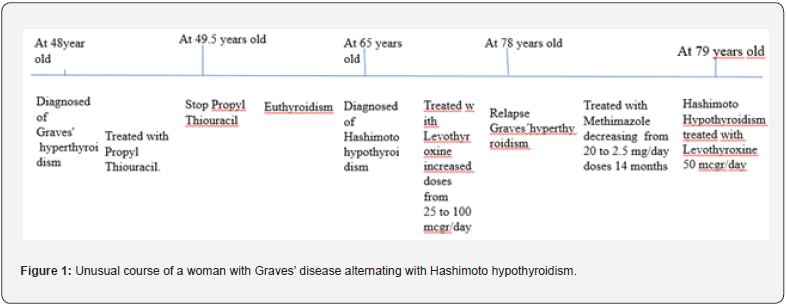
Case report: A 78-year-old woman presented GD, her medical history was notable for had been diagnosed with GD at 58-year-old, she was treated for 18 months with antithyroid drug (ATD). After withdrawal of ATD, she remained in remission for 9 years. Later, she developed HT with frank hypothyroidism, and was treated with levothyroxine for 12 years. At the end of this period, she had Graves’ hyperthyroidism again and was treated with Metimazole for 14 months before returning to hypothyroidism.
Conclusion: there are very rare cases that have an oscillating course, alternating GD, and HT for decades, whose pathogenesis is pending clarification. This case supports the view that GD and HT are two ends of the same spectrum.
Keywords: Graves’ disease 1; Hashimoto thyroiditis 2; autoimmune thyroid disease 3.
Abbreviations: AITD: Autoimmune thyroid diseases; HT: Hashimoto’s thyroiditis; GD: Graves’ disease
Introduction
Autoimmune thyroid diseases (AITD) are organ-specific autoimmune diseases. AITD are the most prevalent alterations that affect the thyroid gland. AITD comprises interrelates conditions: Hashimoto’s thyroiditis (HT), Graves’ disease (GD), atrophic autoimmune hypothyroidism, postpartum thyroiditis, the first two being the most prevalent. The common pathological feature of AITD is the presence of lymphocytic, mainly T cells infiltrate the thyroid gland that may progressively replace the thyroid tissue. Variable thyroid follicular cell atrophy and fibrosis are characteristic of HT, while in GD thyroid follicles are hypertrophied. Anti-tiroperoxidase antibodies (TPOAb) are a sensitive marker of ATID both in HT and GD. Thyroid stimulating hormone receptor antibodies (TSHR-Ab) are characteristic of GD and responsible for hyperthyroidism [1]. One form of AITD may change to another as the course of the immune process progresses [1]. Around 12 % - 20% of patients with GD spontaneously develop Hashimoto hypothyroid after antithyroid drug (ATD) discontinuation [2-4]. Contrarily, with less frequency occurred that a patient with HT became hyperthyroid during its clinical course [5]. In the present case, a patient shows spontaneous oscillations of her thyroid function over a period of 21 years.
Case Presentation
A 78-year-old woman, with anxiety begins to be noticed from about 6 months. Three months later, she added to her symptomatology palpitations, dyspnea and edema in the lower extremities that increase in intensity slowly. Then she requests medical attention in an endocrinology consultation. She was diagnosed with hypothyroidism 12 years ago and treated with 75 mcg/day of levothyroxine. She had not done control thyroid tests for 2 years due to the covid-19 pandemic. A month before the Endocrine consultation, she was attended in a primary care center, for worsening of dyspnea, palpitations, and increased edema in the lower extremities and tachyarrhythmia. Thyroid function tests were done, showed elevation of free T4 and decrease in TSH levels, doctor recommended reducing the dose of levothyroxine to 25 mcg /day, added diuretic (Furosamide) and beta-adrenergic blocker (Bisoprolol) drug to her treatment. Two weeks later due to worsening of her symptoms, she came to our Endocrine office.
Personal medical history was notable for having been diagnosed with Graves’ hyperthyroidism at 58-years-old when living in Houston (USA), she was treated for 18 months with ATD (Propyl-thiouracil). After withdrawal of ATD, she remained in remission for 9 years. Later, she developed Hashimoto’ thyroiditis with frank hypothyroidism, treated with increasing doses of levothyroxine for 12 years. Physical examination revealed a female patient 1.60 meters tall, and 59 kg weight. Blood pressure 150/100, the patient had frank dyspnea, with a fibrillar tremor in both hands, pulse 100/min, with frequent extrasystoles. She also had edema in both ankles. She was diagnosed with relapse of Graves’ hyperthyroidism, and prescribed as treatment: rest, suppress levothyroxine, and administration of Methylmazole (MMI) of 5 mg, 4 tablets per day, and Bisoprolol 2.5 mg every 12 hours. It is also recommended to quit smoking.
Six weeks later, the patients felt better, presented light dyspnea, rhythmic pulse at 76 beats per minute, no edema. The thyroid function test showed Free T4, Free T3, and TSH within the reference values (Table 1). MMI doses were reduced to 2 tablets per day. Two months later she was asymptomatic with thyroid function test within reference values. MMI dose was reduced to 1 tablet per day. Eight weeks later, in view of the results of the thyroid function tests, MMI were reduced to 1 tablet 5 days and a half tablet 2 days. Two weeks after she became to fill anxiety and palpitations, a new function test performed 4 weeks later, revealed a slight increase of Free T4 and Free T3, Table 1, and then MMI dose was increased to 1 tablet per day. The symptoms disappear 10 days later. MMI was maintained until the levels of anti-TSH receptor antibodies were negative. Fourteen months after the diagnosis of GD recurrence, and two months after MMI withdrawal she again presented hypothyroidism demanding treatment with levothyroxine (Figure 1).
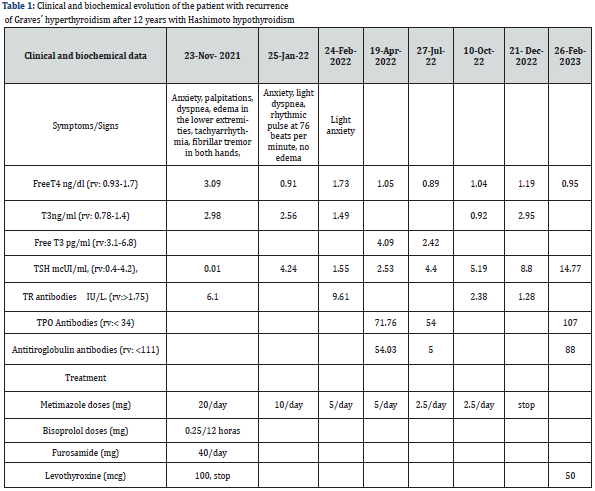
The hormone tests performed included determinations of serum Free T4 (FT4) (reference values: 0.93-1.71 ng/dl), Free T3 (FT3) (reference values: 2.55-4.33 pg/ml), Thyrotropin hormone (TSH) (reference values: 0.30-4.50 mUI/L), all of which were analyzed by an immunochemiluminescent assay, IMMULITE (Diagnostic Products Corp. Los Angeles, CA, USA). The levels of both Thyroid peroxidase antibodies (TPOAb) and thyroglobulin antibodies (TgAb) were measured by a chemiluminiscent assay (Immulite 2000, Diagnostic product Corp, Los Angeles, CA, USA, with reference values of 0-30 and 0-40 mIU/ml respectively. The concentration of Thyroid receptor antibodies (TRAb) (reference values 0-10 IU/L) was measured using a radioreceptor assay (TRAK-assay; Henning, Berlin, Germany). The intra-assay and inter-assay CVs were 5% and 7.5% respectively. South Galicia is an area with sufficient iodine intake [6]. Long-term remission was defined as the absence of clinical manifestations of hyperthyroidism, together with biochemical euthyroidism and negative TRAb values, at least 12 months following the withdrawal of ATDs [7].
Discussion
Autoimmune thyroid disease results from dysregulation of the immune system leading to an immune attack of the thyroid gland. The AITD comprise two main clinical presentations: HT and GD. The clinical hallmark of these conditions is hypothyroidism and hyperthyroidism, respectively. One form of clinical presentation can change to another as the immunological process progresses. There have been cases of patients switching from Graves’ hyperthyroidism to Hashimoto hypothyroidism, being less frequent patients switching from hypothyroidism to hyperthyroidism [8], due to the critical loss of thyroid mass that can respond with TSHR Ab [9], although it is described some patient who developed frank hyperthyroidism and required treatment with ATD [10]. The shift from Graves’ disease to Hashimoto’s disease and vice versa in the same patient suggests that both would be the same disease that can be expressed in two ways. However, genetic studies indicate that GD and HT are modestly related diseases [11].
In the present case report, a woman initially diagnosed with Graves’ hyperthyroidism treated with ATD for two years. After withdrawal of ATD she remained in remission for 9 years. After which she developed Hashimoto’s thyroiditis, being treated with increasing doses of levothyroxine. Twelve years later, frank Graves’ hyperthyroidism requires treatment with ATD. She was treated with MMI for 14 months. Finally, after two months of withdrawal ATD she developed Hashimoto’s hypothyroidism needing small doses of levothyroxine. Cases of alternating hyperthyroidism and hypothyroidism are very rare [12]. The unusual course of this case supports the view that it is the same disease that can be expressed from both hyper- and hypothyroidism.
Some authors postulated that the pathogenesis of patients alternating hyperthyroidism and hypothyroidism is due to the balance between the levels of stimulating TSHR-Ab with thyroid Blocking hormone receptor antibodies (TBHR-Ab) [13]. However, in patients with long-term course, when presented HT, follicular cells are destroyed to a variable extent, depending on the chronicity of the HT related hypothyroidism [14], and for the development of frank hyperthyroidism requires a restoration, at least partially, of the mass of follicular cells of the thyroid. Thus, the pathogenesis of such a phenomenon is pending clarification.
This case also draws attention to the fact that we must bear in mind that patients with long-standing autoimmune hypothyroidism can be transformed into frank hyperthyroid ism, which requires diagnosis and treatment without delay. Some authors believe that given the unpredictability of the diseases in these patients who alternate hyperthyroidism and hypothyroidism, ablative treatment would be advised [10]. In my opinion, educating patients and their families about the nature of the disease, its clinical characteristics, and an annual follow-up, can be sufficient to manage these cases properly, avoiding postablative hypothyroidism that is not easy to handle, in addition, if we avoid ablative treatment, we can know the natural history of Graves’ disease in more patients, without any added risk [15].
Conclusion
Although very rare, there are cases of patients who spontaneously alternate long-term periods of Graves’ hyperthyroidism with Hashimoto related hypothyroidism for decades, whose pathogenesis is pending of clarification. The present case supports the view that GD and HT are two ends of the same spectrum. Clinicians must also keep in mind that although rare, these cases exist and require diagnosis and treatment without delay.





No comments:
Post a Comment