Ophthalmology - Juniper Publishers
Abstract
Cystinosis is a metabolic pathology characterized by the accumulation of cystine in lysosomes, essentially damaging the eyeball and the kidney. It is characterized by a cystine transport defect due to a mutation in the CTNS gene. Our objective was to report two familial cases of cystinosis with ocular manifestation. It involved a 7-year-old girl (Case 1) and her 18-month-old little brother (Case 2), followed in nephropediatrics for cystinosis and referred to our department for an eye assessment. Rickets resistant to vitamin D supplementation were noted . They presented with Fanconi syndrome and renal ultrasound was normal in both. At the slit lamp we found superficial punctate keratitis and a deposit of refractive microcrystals scattered over the entire extent of the cornea, with a Gahl score of 3.00 in both patients. A homozygous CNTS mutation was revealed by molecular biology. The asymptomatic parents presented the same mutation in the heterozygous state. They benefited from treatment based on vitamin A in ophthalmic ointment and correction of hydro-electrolyte disorders and vitamin D supplementation. Cystinosis is a rare genetic pathology. It is to be looked for in the presence of corneal crystals associated with a delay in height and weight growth. The diagnosis is made by measuring intra leukocyte cystine. Cysteamine, orally and ocularly, has significantly improved the prognosis. Genetic counseling is of paramount importance.
Keywords: Cystinosis, Corneal crystals, Fanconi syndrome, Cysteamine
Introduction
Cystinosis is a lysosomal, autosomal recessive pathology caused by mutation of the CTNS gene encoding cystinosin. This membrane transport protein allows the efflux of cystine from lysosomes to the cytoplasm, where it is degraded into cysteine. The intralysosomal accumulation of cystine induces the formation of insoluble crystals responsible for progressive multi-organ failure, particularly in the kidneys, pancreas, thyroid and eyes. Several ocular locations of this crystal accumulation have been described and can jeopardize the quality of life of affected patients, possibly creating visual impairment and even blindness [1]. Our objective was to report two familial cases of cystinosis with ocular manifestation.
Case Description
It involved a 7-year-old girl (Case 1) and her 18-month-old little brother (Case 2), respectively from a family of four children, the result of second-degree parental consanguinity. They were followed by a nephropediatrician for cystinosis and referred to our department for an eye assessment. Pediatric examination revealed rickets resistant to vitamin D supplementation, marked by failure to thrive (-2 standard deviations). In Case 1, an epiphyseal bulge at the ankles and wrists, a genu valgum, was noted. On laboratory examination, they presented Fanconi syndrome marked by polyuria, hypocalcemia, hypokalemia, hyponatremia, hypophosphatemia, hypovitaminosis D and elevated β 2-microglobinuria. Renal ultrasound was normal, well differentiated in both.
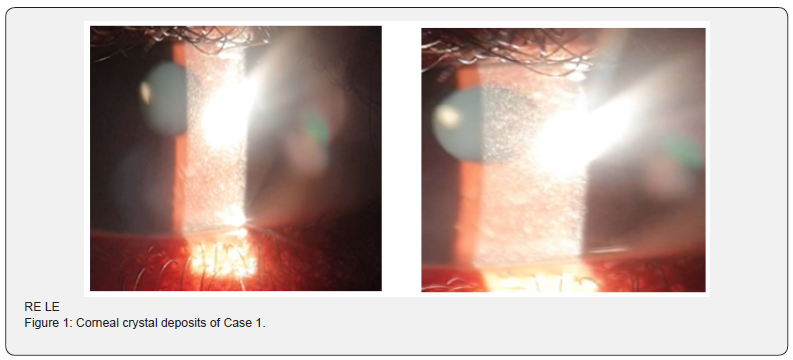
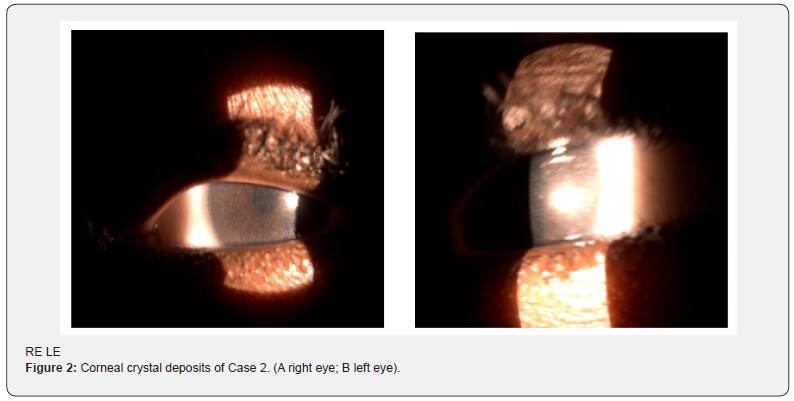
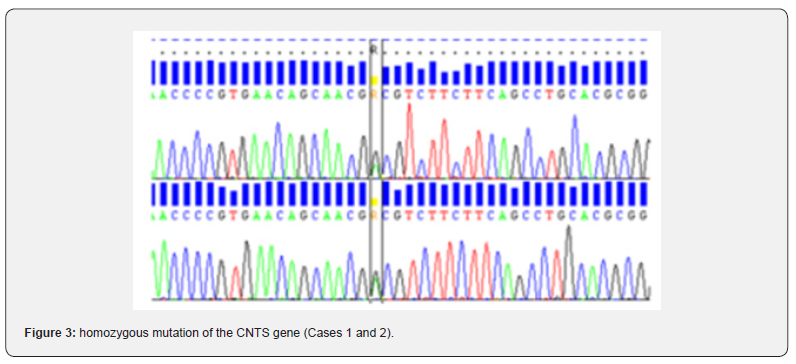
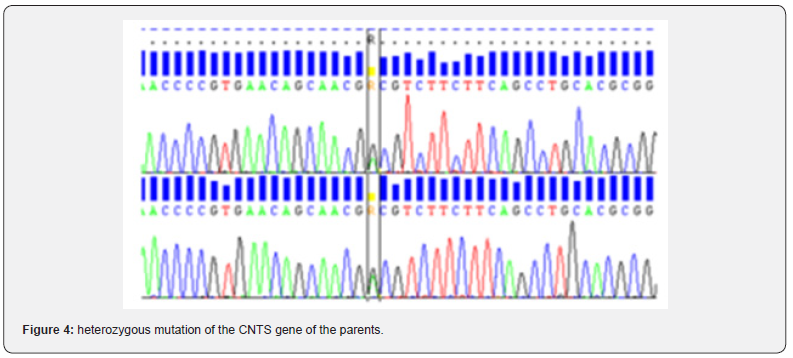
The ophthalmological examination showed distance visual acuity assessed according to the Léa scale at 0.2 at OD and 0.4 at OG in Case 1. It was difficult to assess in Case 2, who presented good light tracking at 2 eyes. At the slit lamp, there was superficial punctate keratitis and a deposit of refractive microcrystals scattered over the entire extent of the cornea, with a Gahl score of 3.00 in both patients (Figures 1 and 2). The remainder of the examination was normal in both Cases. The ophthalmological examination of both parents was unremarkable. Molecular biology allowed us to make the diagnosis of cystinosis in the 2 Cases, revealing a homozygous mutation of the CNTS (c.614A>G) (Figure 3). The asymptomatic parents presented the same mutation in the heterozygous state (Figure 4). The other 2 children of the siblings were unaffected by the mutation. They benefited from treatment based on vitamin A in ophthalmic ointment and correction of hydro-electrolyte disorders and vitamin D supplementation.
Discussion
Cystinosis is an autosomal recessive disease that is caused by an accumulation of cystine in lysosomes. This concerns cells of all tissues and organs with greater sensitivity on the part of kidney tissue. It is the absence of cystinosine, a cystine transporter located in the lysosome membrane, which is responsible for this accumulation, with cystine no longer being transported out of the lysosome [2]. Found in all ethnic groups, this disease has a prevalence of between one birth in 200,000 and one birth in 100,000 depending on the country [3]. These were the first cases found in our department.
Ninety-five percent of people with cystinosis have the infantile nephropathic form. Three clinical forms of cystinosis (infantile, juvenile and ocular) have been described depending on the age of onset and the severity of symptoms. In the infantile form, the most common, the first signs appear after 3 months, marked by a polyuro-polydipsic syndrome and significant growth retardation, secondary to a generalized proximal tubular syndrome (Toni-Debré-Fanconi syndrome) with disturbances. hydro electrolytes severe.
The accumulation of cystine in different organs is responsible for hypothyroidism, insulin-dependent diabetes, hepatosplenomegaly with portal hypertension, muscle damage and brain damage. Ocular damage, secondary to cystine deposits in the cornea and conjunctiva, leads to tearing and photophobia. The disease gradually progresses after the age of 6 to end-stage renal failure. The juvenile form appears after the age of 8 years and presents a clinical picture of intermediate severity, with end-stage renal failure occurring after the age of 15 years [2-4]. Finally, there is the non-nephropathic or pure ocular form , which appears in adulthood . The 2 patients reported presented with infantile cystinosis.
The severity of the disease is essentially based on kidney damage which can be life-threatening. Cystinotic nephropathy manifests itself by weight loss, Fanconi syndrome, damage to the renal glomerulus and manifestations affecting other organs. The extrarenal involvement is essentially ocular and mainly causes photophobia and blepharospasm. Corneal damage is constant, appears from 12 months, and consists of deposits of birefringent spindle crystals which accumulate over time in the corneal stroma, and progress from the anterior stroma towards the endothelium. The appearance is scintillating and multicolored on biomicroscopic examination. Superficial punctate keratitis and strip keratitis are often associated, and the corneal endothelium is spared. In more advanced stages, limbal corneal neovascularization can be found [5,6]. The severity of corneal damage can be assessed by the Gahl biomicroscopic score (0 to 3) and by OCT of the anterior segment [6]. Confocal microscopy makes it possible to analyze and quantify corneal crystals, assess the infiltration of inflammatory cells and look for nerve damage [7].
Cystinotic retinopathy is rarer. Crystal deposits are sometimes noted throughout the retina. Depigmentation of the retinal periphery associated with pigment deposits is possible, which can progress to retinal atrophy [5,8]. The crystals can also be located on the conjunctiva, the iris, the ciliary body, the anterior lens capsule, the choroid or the optic nerve and cause complications such as angle closure glaucoma, posterior synechiae, edema. macular, choroidal neovascularization [6,8]. Our patients did not present any localization other than corneal involvement.
The biochemical diagnosis is based on the intra-leukocyte cystine dosage which is the gold standard. It is a sensitive and precise examination for the confirmation of the disease [5]. It is not available in our context.
The molecular diagnosis is confirmed by the presence of mutations in the CTNS gene coding for cystinosine located on chromosome 17. There are genotype and phenotype correlations explaining the variability of the symptoms [3]. This genetic study is necessary to confirm the diagnosis and carry out family studies with a view to genetic counseling. In our case, it made it possible to confirm the genetic mutation in the 2 children and in the parents.
Treatment with cysteamine has improved the prognosis of the disease. Its aim is to deplete lysosomes of cystine [1,3]. Its early administration makes it possible to delay the age of onset of end-stage renal failure and prevent late complications. To achieve effective corneal concentrations, topical administration of cysteamine in the form of ophthalmic gel is required [1]. This requires an increased dosage which can make treatment compliance difficult. As cysteamine is not marketed in Senegal, patients received symptomatic treatment with vitamin A ointment and hydro electrolytic and vitamin supplementation.
Conclusion
Cystinosis is a rare genetic pathology whose main manifestation is Fanconi syndrome. It is to be looked for in the presence of corneal crystals associated with a delay in height and weight growth. The diagnosis is made by measuring intra leukocyte cystine. Cysteamine, orally and ocularly, has significantly improved the prognosis. Genetic counseling is of paramount importance.
To Know more about JOJ Ophthalmology
Click here: https://juniperpublishers.com/jojo/index.php
To Know more about our Juniper Publishers
Click here: https://juniperpublishers.com/index.php




No comments:
Post a Comment