Anesthesia & Intensive Care Medicine - Juniper Publishers
Abstart
Background: Postoperative delirium exacerbates the prognosis of elderly surgical patients. Postoperative agitation or confusion is one of the symptoms of hyperactive delirium. We retrospectively evaluated the incidence of postoperative abnormal psychomotor behavior in elderly surgical patients according to different anesthetic methods: nerve block vs. neuraxial anesthesia.
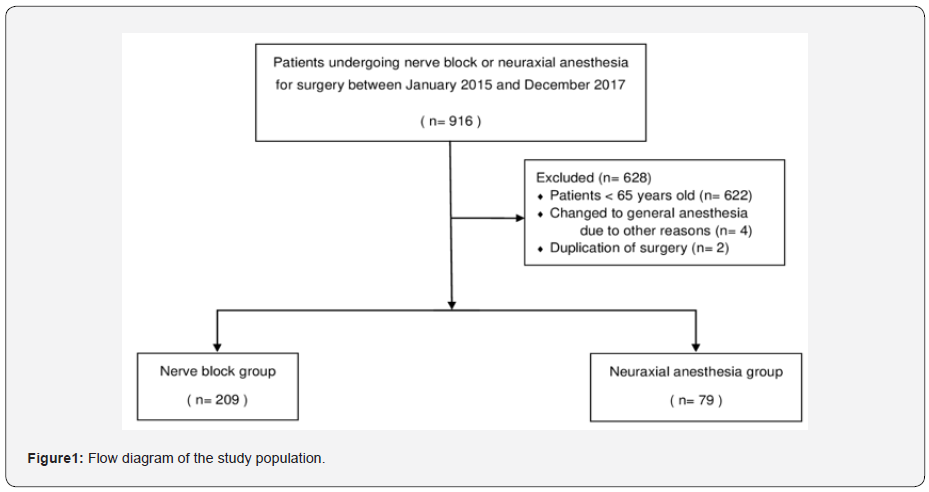
Methods: The medical records of 288 patients older than 64 years who underwent surgery with regional anesthesia between January 2015 and December 2017 were divided into two groups, the nerve block group (n=209) and the neuraxial anesthesia group (n=79). The primary outcome was postoperative agitated behaviors, and the secondary outcomes were patient and anesthesia related factors.
Results: In elderly patients, the incidence of agitated behavior was lower in the nerve block group compared with the neuraxial anesthesia group (4 {1.3%} vs. 8 {2.8%}, P=0.004). Neuraxial anesthesia, older age and male gender were found to be significant factors for the occurrence of agitation in elderly patients.
Conclusions: This study suggests that nerve block, as compared with neuraxial anesthesia, may have a greater beneficial effect in reducing postoperative agitated behavior in surgical elderly patients.
Keywords: Nerve block, Neuraxial anesthesia, Postoperative agitated behavior, Hyperactive delirium
Abbreviations: ANCOVA: Analysis of Covariance, CAM-ICU: Confusion Assessment Method in The Intensive Care Unit, OAA/S: Observer’s Assessment of Alertness/Sedation, RASS: Richmond Agitation-Sedation Scale
Introduction
Postoperative delirium can exacerbate the prognosis of surgical patients, result in increased postoperative morbidity and mortality, and generate higher hospital costs [1-3]. Postoperative delirium is a common complication, especially in elderly patients, occurring in up to 60% of patients after major surgery [4]. The risk factors for postoperative delirium such as old age, hip surgery, and propofol use are known [5-7]. In addition, postoperative pain is an important factor related to postoperative delirium [8]. However, the pathophysiology of postoperative delirium has not been elucidated yet. A previous study reported that peripheral nerve blocks reduce side effects such as postoperative delirium via an opioid-sparing effect [9].
There have been many studies on the incidence of delirium in different types of anesthesia. However, most studies compared general anesthesia with neuraxial (spinal, epidural, or combined spino-epidural) anesthesia [10,11]. There are few studies comparing neuraxial anesthesia with peripheral nerve block in regional anesthesia.
There are three types of delirium: hypoactive, hyperactive, and mixed [12]. Although the hypoactive type is more common than the hyperactive type [13], the abnormal behavioral patterns of the hyperactive type, such as agitation or confusion, are considered harmful to patients and medical providers and need to be quickly managed.
In this study, based on the hypothesis that nerve block may reduce the incidence of abnormal psychomotor behavior compared with neuraxial anesthesia, we retrospectively investigated the incidence of postoperative agitated or anxious behavior with other risk factors in elderly patients who underwent surgery with regional anesthesia.
Methods
Study population and data collection
After obtaining an approval from the Institutional Review Board at Hanyang University Hospital (HYUH 2018-07-006), this study was registered at the Clinical Research Information Service (KCT0003279). The requirement for informed consent was waived. Electronic medical records from January 2015 to December 2017 were reviewed. Adult patients aged 65 and over who underwent surgery with neuraxial anesthesia or nerve block were listed for this study.
Anesthesia techniques: neuraxial anesthesia and nerve block
Patients were injected intramuscularly with midazolam 1-2mg and atropine 0.5mg for anti-anxiety and reduction of salivation at the ward and were transferred to the operating room. The neuraxial anesthesia technique included either spinal or combined spinal-epidural anesthesia, which was chosen according to the duration of operation. In our hospital, an optimal dose of 0.5% hyperbaric bupivacaine is used intrathecally with or without fentanyl (10-20μg). In lengthy surgeries, 0.75% ropivacaine is injected additionally through the epidural catheter placed for combined spinal-epidural anesthesia at 2 hours after surgical incision. The nerve block technique includes brachial plexus block, sciatic nerve block or combined sciatic and femoral nerve block, which are chosen according to the patient’s lesion. In our hospital, an optimal dose of 0.75% ropivacaine is used with or without 2% lidocaine under ultrasound guidance.
Intraoperative sedation
Sedation was provided to patients after confirming the proper regional anesthesia level and obtaining hemodynamic stability. The sedative agent was selected among propofol, dexmedetomidine, remifentanil, midazolam, mixed, or no agents depending on the anesthesiologist’s preference. Sedation was usually maintained to achieve an observer’s assessment of alertness/sedation (OAA/S) score of 3 or 4. For sedation, propofol (Fresofol®, Fresenius Kabi, Graz, Austria) was administered continuously via a targetcontrolled infusion device (Orchestra®, Fresenius vial, Brézins, France), and the effect-site concentration was maintained within 0.5-2.0μg/mL. Dexmedetomidine (PrecedexfM, Hospira Inc., Lake Forest, IL, USA) was diluted with 0.9% normal saline to a concentration of 4μg/mL. Dexmedetomidine of 1μg/kg was administered over a 10-min period as a loading dose and was then infused continuously at 0.1-0.5 μg/kg/h. Remifentanil (UltiAN®, Hanlim Pharm.co., LTD., Republic of Korea) was diluted with 0.9% normal saline to a concentration of 50μg/mL and then infused continuously at 0.05-0.1μg/kg/h. Midazolam (MIDAZOLAM Bukwang, Bukwang Pharrm. Co., LTD., Republic of Korea) was administered 0.5-1mg as needed according to the OAA/S score. In the case of the mixed method, midazolam and propofol or dexmedetomidine, or propofol and remifentanil, were administered.
Assessment of postoperative abnormal behavior
The Richmond agitation-sedation scale (RASS) was used to evaluate the presence of patient abnormal behaviors after surgery [14]. The postoperative daily progress notes and nursing notes were recorded regularly by doctors and nurses in charge. By evaluating these notes, we were able to determine which patients were documented with abnormal behaviors, including agitated, uncooperative, aggressive, confused, combative, violent, hallucination, delusion, or removal of catheters, plasters, or bandages. In addition, the recording of consultation for delirium with the Psychiatry Department was determined to be abnormal behavior. These descriptions of abnormal behavior corresponded roughly to RASS scores of +2, +3, or +4.
Other outcome variables
The following variables were further evaluated:
a. preoperative factors (age, gender, weight, height, body mass index, and American Society of Anesthesiologist (ASA) physical status classification)
b. intraoperative factors (surgery and anesthesia time, use of midazolam for premedication, and use of sedative drugs); and
c. postoperative factors (total admission period).
Statistical analysis
Data are presented as the mean plus or minus the standard deviation or a number (proportion). All continuous data were assessed for normality using the Shapiro-Wilk test. Incidence was analyzed by the chi-square test. The numerical data were assessed using independent t-tests, as appropriate. A binary logistic regression model was used to evaluate the predisposing factors for abnormal postoperative behavior. The dependent variable was the occurrence of abnormal postoperative behavior; and the independent variables were anesthesia method, age, gender, preoperative stroke history, preoperative depressive disorder history, use of sedative agents, and admission period. Analysis of covariance (ANCOVA) was performed to reduce the risk of confounder effects between the nerve block group and the neuraxial anesthesia group. The covariates were age, gender, preoperative stroke history, preoperative depressive disorder history, use of sedative agents, surgery type, and admission period. The dependent variable was the anesthesia method: nerve block or neuraxial anesthesia. Also, the incidence of abnormal postoperative behaviors according to the types of sedatives in elderly patients was analyzed by the Kruskal-Wallis test. All analyses were carried out using IBM® SPSS® Statistics version 22.0 (IBM Corporation, NY, USA). P<0.05 was considered statistically significant.
Results
A total of 916 patients were screened and 622 patients under 65 years old were excluded. Four cases were changed from regional anesthesia to general anesthesia due to incomplete anesthesia. Two cases were excluded due to duplicated surgery of the same patient. Nerve block and neuraxial anesthesia were performed for surgery in 209 and 79 patients, respectively (Figure 1).
Patient characteristics and information regarding anesthesia are shown in Table 1. Demographic data were comparable between the two groups except age, gender, preoperative stroke, and depressive disorder histories, use of sedative agents, surgery type, and admission period. Preoperative stroke and depressive disorder histories were lower in the nerve block group than in the neuraxial anesthesia group (P<0.001 and P<0.001, respectively). The use of perioperative sedative agents was lower in the neuraxial anesthesia than in the nerve block group (P=0.034), and the effect of sedative agents was significantly different between the two groups (P<0.001). Surgery type was significantly different between two groups (P<0.001). Admission period was lower in the neuraxial anesthesia group than in the nerve block group (P=0.001). In order to reduce the risk of confounder effects between the two groups, ANCOVA was performed by setting age, gender, preoperative stroke history, preoperative depressive disorder history, use of sedative agents, surgery type, and admission period as covariance.
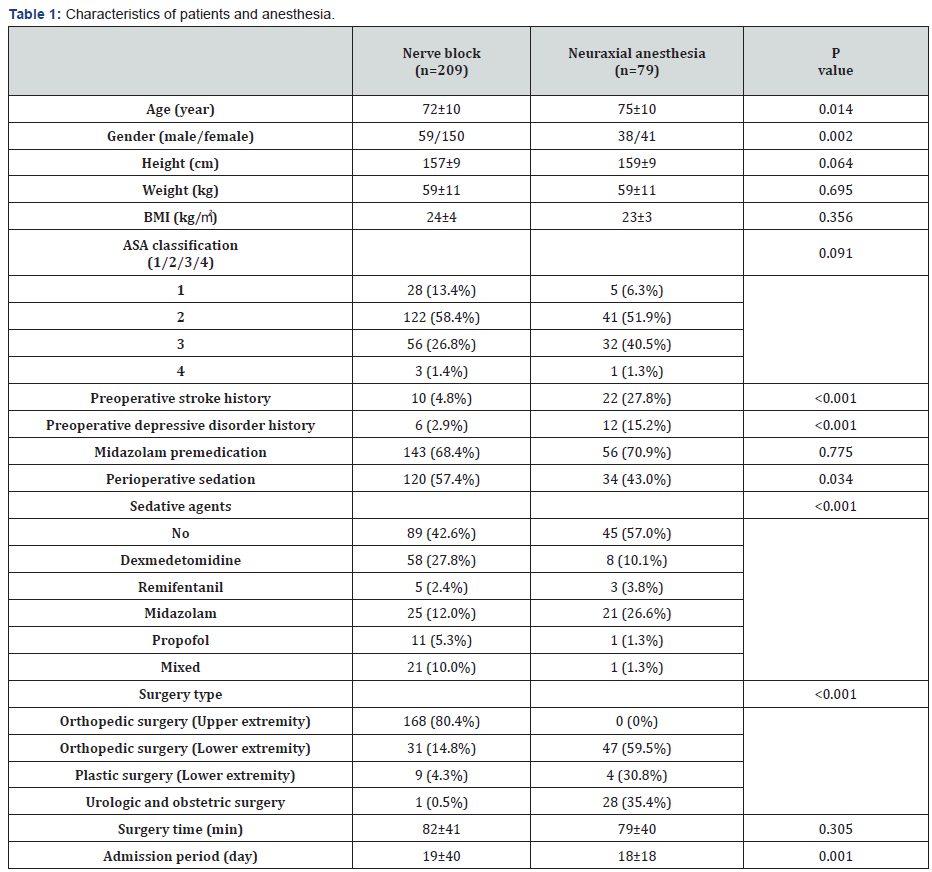
Data are expressed as the mean±SD or the number of the patients (proportion). BMI: body mass index; ASA: American Society of Anesthesiologist classification
We found that there were significantly less postoperative agitated behaviors in the nerve block group than in the neuraxial anesthesia group (1.3% vs. 2.8%, P=0.004), which was corrected with the ANCOVA method. In the nerve block group, one of the 168 patients receiving the brachial plexus block and three of the 40 patients receiving sciatic nerve block had abnormal postoperative agitated behaviors (Table 2).
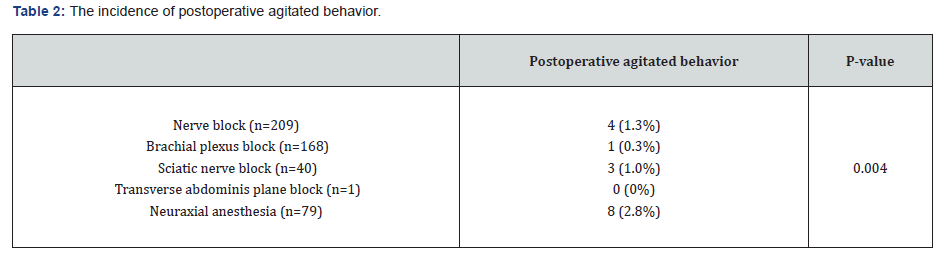
Data are expressed as the mean±SD or the number of the patients (proportion).
The following parameters were confirmed as significant determinants for the occurrence of postoperative agitated behaviors by the binary logistic regression analysis (Table 3). Patients receiving neuraxial anesthesia were 65.26 (95% CI: 2.14- 1991.9, P=0.017) times more likely to experience postoperative agitated behaviors than patients receiving nerve block. Patients were 1.15 (95% CI: 1.03-1.29, P=0.016) times more likely to experience abnormal postoperative behaviors for each year increase in age. Men were 33.24 (95% CI: 4.24-260.7, P=0.001) times more likely to experience postoperative agitated behaviors than women.
The incidence of postoperative agitated behaviors according to the types of sedatives in elderly patients was not significantly different (p=0.217) (Table 4).

OR: odds ratio; CI: confidence interval.

Data are expressed as the mean±SD or the number of the patients (proportion).
Discussion
In this retrospective study, we found that surgical elderly patients under nerve block presented less postoperative agitation than those under neuraxial anesthesia. We believe that this is the first study to verify that type of regional anesthesia during surgery can affect postoperative behavioral pattern.
When assessing the data, our first consideration was whether postoperative agitated, anxious, or confused behavior was associated with postoperative delirium. Delirium can be divided into three types, hypoactive, hyperactive, or mixed type, according to the motor-activity profile [12]. Although the incidence of the hypoactive type of delirium is known to be more frequent, this study focused on symptoms of the hyperactive type. Agitation and confusion are major symptoms of hyperactive delirium. These symptoms can be a threat to patient prognosis and the safety of medical persons. Therefore, rapid diagnosis and multimodal approaches to actively prevent postoperative agitated behaviors are necessary.
Previous studies [10,11] compared general anesthesia with regional anesthesia and showed no difference in the incidence of postoperative delirium. However, the researchers did not investigate the types of regional anesthesia and the subtypes of delirium in detail. Our results specified that nerve block is associated with the reduction of agitated behavior presented in hyperactive delirium. The postoperative agitated state is related to patient safety. The type of anesthetic method is thought to be a modifiable factor, and according to our results, nerve block for surgery can be regarded as one of the preventive strategies for patients with a high possibility of postoperative hyperactive delirium.
To detect abnormal psychomotor behavior retrospectively, choosing the appropriate assessment tool is important. The confusion assessment method in the intensive care unit (CAMICU) is regarded as the standard tool for evaluating delirium [15]; however, in our study, checking CAM-ICU data retrospectively was challenging. Thus, we used RASS, which is a simpler scale than CAM-ICU, to detect any postoperative abnormal behavior. RASS was originally developed to assess the level of agitation and sedation [14]. RASS is composed of four levels of anxiety or agitation (+1 ~ +4) and 5 levels of sedation (-1 ~ -5) with a calm or alert state (0 point) as the center. Unfortunately, we were unable to prove whether the hypoactive subtype of delirium can be relieved by nerve block. Hypoactive delirium often cannot be recognized clinically, and there are limitations in evaluating the hypoactive state via a retrospective investigation [16,17]. Therefore, a precise and well-controlled prospective study may be required for this issue.
This study has a limitation to consider when interpreting its results. Because this study is retrospective in nature, the type of anesthetic method was not randomized. In addition, no specific sample size was determined. Based on a post-hoc power analysis, this study has 83.3% power with a type 1 error of 5% to detect the decreased incidence of postoperative agitated behavior in the nerve block group.
Conclusion
In conclusion, the nerve block method was associated with lowering the incidence of postoperative agitation in elderly patients undergoing surgery via regional anesthesia compared with neuraxial anesthesia. Thus, nerve block can be considered as one of the potential preventive strategies for postoperative hyperactive delirium.
To Know more about Anesthesia & Intensive Care Medicine
Click here: https://juniperpublishers.com/index.php




No comments:
Post a Comment