Global Journal of Otolaryngology - Juniper Publishers
Abstract
Pediatric cholesteatoma is classified into congenital cholesteatoma and acquired cholesteatoma. As congenital cholesteatoma has few symptoms, the cases are usually discovered with hearing loss during the examination during enrollment in an elementary school. Acquired cholesteatoma is associated with inflammatory changes and eustachian tube dysfunction of the middle ear, and it is said that most cases are more severe than congenital cholesteatoma. We analyzed 46 cases (47 ears) of pediatric cholesteatoma, diagnosed before attending school and operated upon. We also examined the discovery mechanism, classification, progress level, operative methods of cholesteatoma, postoperative hearing tests, and recurrences. Approximately 85% of these cases were of congenital cholesteatoma; additionally, approximately 15% had acquired cholesteatoma. As a result, there were no significant differences between congenital cholesteatoma cases and acquired cholesteatoma cases in terms of the degree of progression, hearing ability prognosis, and rate of recurrence. Moreover, the rate of recurrence and hearing ability prognoses were better than those in previous reports.
In general, there are several cases in which the cholesteatoma extends to anatomical blind spots such as the tympanic sinus or facial recess in pediatric cholesteatoma. Several papers have discussed the availability of middle ear surgeries using endoscopy (i.e., trans canal endoscopic ear surgery [TEES]). However, we performed middle ear surgery using microscopy (i.e., microscopic ear surgery [MES]) in all cases, and we have invented a way to find operation fields using procedures such as drilling the anterior wall of the external auditory canals.
In conclusion, we believe that polite dissection of the cholesteatoma matrix under the microscope is an important factor in the low rate of recurrence of cholesteatoma.
Keywords: Congenital cholesteatoma; Acquired cholesteatoma; Pediatric cholesteatoma; MES; TEES
Introduction
Middle ear cholesteatoma is classified roughly into congenital cholesteatoma and acquired cholesteatoma. Additionally, the acquired cholesteatoma is classified into three types: pars flaccida, pars tensa, and secondary types. As all cases of cholesteatoma are progressive diseases and cause complications, not only otorrhea and deafness, but also vertigo, deafness, facial nerve palsy, sigmoid sinus thrombosis and intracranial complications such as meningitis and epidural/subdural abscess [1], early diagnoses and early operations are required.
Pediatric cholesteatoma is classified into congenital cholesteatoma and acquired cholesteatoma. It is said that the congenital cholesteatoma is relatively rare and accounts for approximately 12.9% in all middle ear cholesteatomas [2]. Due of the lack of symptoms, such as otorrhea in congenital cholesteatoma, the cases are usually discovered for hearing loss at examination at enrollment in an elementary school. Therefore, congenital cholesteatoma before attending school is often confirmed accidentally by a mesotympanic white lesion in the otolaryngology outpatient department. Acquired cholesteatoma is associated with inflammatory changes and eustachian tube dysfunction in the middle ear. Compared with congenital cholesteatoma, the grades of disease are often severe [3]. As most cases of pediatric cholesteatoma are often diagnosed by a medical examination at school attendance, there are few articles about the cases that are diagnosed before attending school. We examined cases that were diagnosed before attending school and were operated on at this time.
In addition, there are numerous reports that trans canal endoscopic ear surgery (TEES) is effective because congenital cholesteatoma matrices often invaginate into the tympanic sinus and facial nerve recess, which are anatomical blind spaces in pediatric cholesteatoma [4]. Despite many reports of TEES, we performed microscopic ear surgery (MES) in all middle ear surgery cases in our department. Therefore, the aim of this study was to investigate the results of our operation via microscopy, such as the rate of recurrence and postoperative hearing levels in pre-school pediatric cholesteatoma.
Materials and Methods
We examined 46 cases (47 ears) who were diagnosed with cholesteatoma before enrollment at school in the Department of Otolaryngology, Tokyo Women’s Medical University East Medical Center from June 2010 to January 2019. In total, 28 cases were boys, 18 cases were girls, and the average age of the 46 cases was 3.6 years old. In these cases, we examined the consultation opportunity, classification, progress level, operative method of cholesteatoma, postoperative hearing test, and recurrences. We classified all cases based on the JOS staging system for middle ear cholesteatoma (2015) [5]. Cholesteatomas that develop congenitally in the middle ear cavity and is non-continuous with the tympanic membrane and external auditory canal were classified as congenital cholesteatoma. We also classified the acquired cholesteatoma into the flaccid pars flaccida type, pars tensa type, and secondary type. Cholesteatomas occurring due to secondary development of cornified epithelium in the tympanic membrane and behind the handle of the malleus from the perforated margin of a perforation in the pars tensa were also classified as secondary cholesteatoma. Moreover, we evaluated the extension of cholesteatoma using the JOS staging system for middle ear cholesteatoma (2015) [5]. The postoperative hearing test results showed ossicular reconstruction and passed more than one year, and audiometric test results were intended for 27 cases. We judged three patterns as successful cases as below:
a. within 15 dB of air bone gap,
b. above 15 dB of hearing improvement, and
c. within 30 dB of hearing level,
based on the Guideline for Reporting Hearing Results in Middle Ear and Mastoid Surgery(2010). In addition, we classified the cases of recurrence into reconstruction recurrence and persistence recurrence as the mechanism of recurrence.
Result
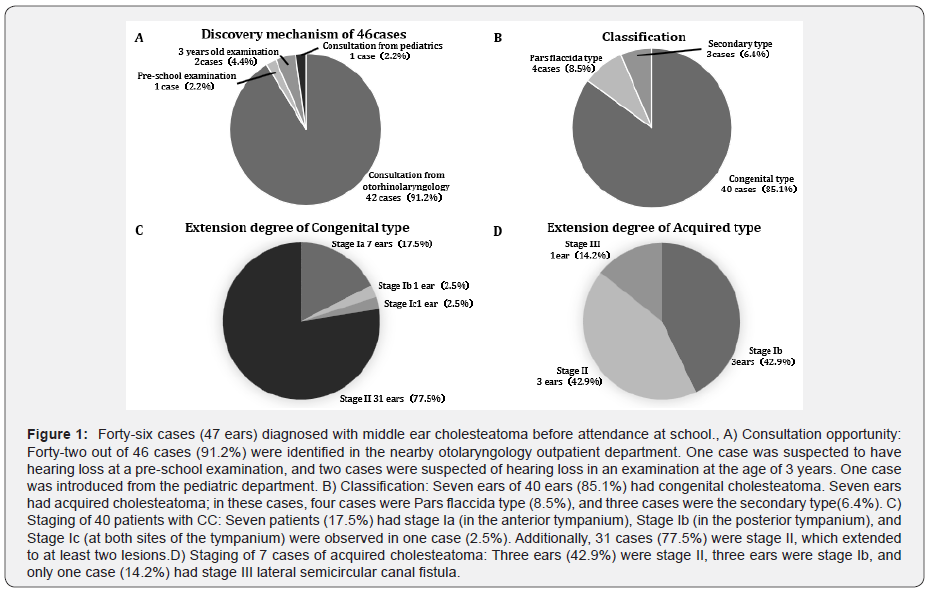
The opportunity to consult our department was obtained by consultation with other otorhinolaryngologists in more than 90% of cases. In one case involving a 3-year-old child, hearing loss was suspected at the examination; additionally, one patient who was referred from pediatrics was noted to have hearing loss during a pre-school medical examination (Figure 1A). In addition, 40 ears (85.1%) showed congenital cholesteatoma, and the acquired cholesteatoma was seen in 7 cases (14.9%). In acquired cholesteatoma, three cases were secondary cholesteatoma, and four cases were pars flaccida cholesteatoma (Figure 1B). For congenital cholesteatoma, 9 cases (22.5%) were stage I, one lesion was extended, and 31 cases (77.5%) were stage II, which extended to at least two lesions (Figure 1C). As for the acquired cholesteatoma, only one case was stage III with a lateral semicircular canal fistula; however, Stage I and Stage II were observed to occur in three cases (Figure 1D). There was no clear tendency denoting that the cases of acquired cholesteatoma had a more severe extension in our cases.
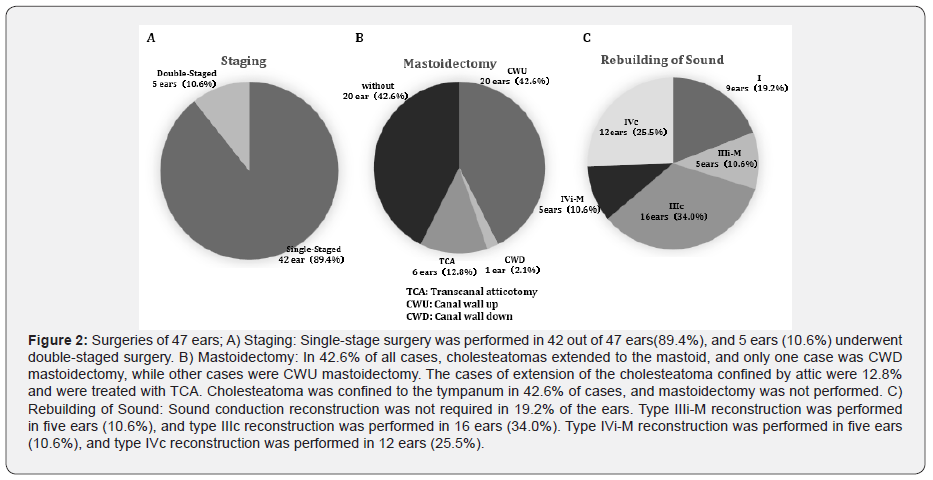
We performed single-stage operations in approximately 90% of cases (Figure 2A). In the cases in which cholesteatomas extended to the mastoid, only one patient underwent canal wall down (CWD) mastoidectomy (i.e., drilling of the posterior wall of the external auditory canal). Notably, other cases underwent canal wall up (CWU) mastoidectomy (i.e., preserving the posterior wall of the external auditory canal). In total, 12.8% of cases of extension of the cholesteatoma confined by the attic were treated with trans canal atticotomy (TCA). Cholesteatoma was confined to the tympanum in 42.6% of cases, and mastoidectomy was not performed (Figure 2B). Approximately 80% of the cases required sound conduction reconstruction, and type III reconstruction was required in 21 cases(44.6%) and type IV in 17 cases(36.1%) (Figure 2c).
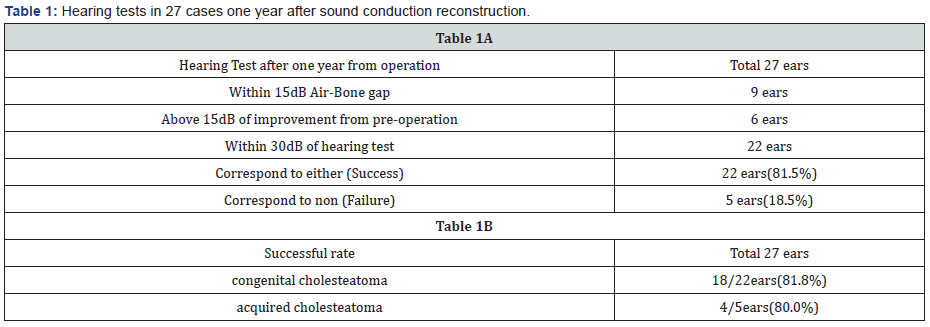
We evaluated hearing tests in 27 cases one year after sound conduction reconstruction; additionally, the success rate was 81.5% in 22 cases (Table 1A). The success rate was 81.8%(18/22 cases) for congenital cholesteatoma and 80.0%(4/5 cases) of acquired cholesteatoma. However, the evaluation was difficult because the number of acquired cholesteatoma cases were few. There was no significant difference in the hearing prognoses between congenital cholesteatoma and acquired cholesteatoma (Table 1B).
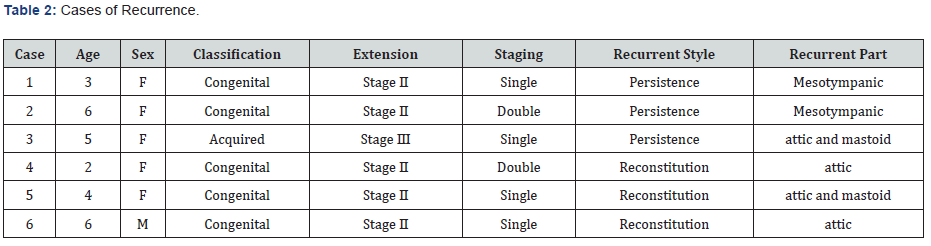
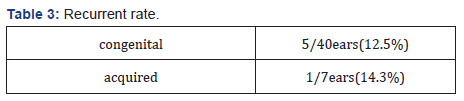
Recurrences were found in six cases in 47 cases(12.8%). Six cases were all advanced cases of stage II or stage III, and there were no recurrence cases in the case of Stage I (Table 2). The recurrences seemed to have several persistence-related recurrences in the previous report [6]; however, persistence-related, and reconstitution-related recurrences occurred in three cases. Additionally, the recurrent style did not show any apparent difference (Table 2). Recurrences were observed in 5 ears out of 40(12.5%) of congenital cholesteatoma and in one case (14.3%)of acquired cholesteatoma (Table 3). As there were few cases of acquired cholesteatoma, the evaluation was difficult; no major differences in the recurrence rate between congenital cholesteatoma and acquired cholesteatoma were found.
Discussion
There have been several discussions about the surgical method for middle ear surgery. There are numerous papers comparing the methods of mastoidectomy to determine the superior method: CWD or CWU [7]. In our department, we often choose CWD mastoidectomy based on the rate of recurrences in most adult cases, except in cases where pneumatization of the mastoid is highly developed. Past reports concluded that CWD mastoidectomy can obtain a low recurrence rate and a high rate of trouble-free ear in the long term in pediatric cholesteatoma [8]. However, in pediatric cases, we choose CWU mastoidectomy because of the undeveloped pediatric temporal bone; this method helps to maintain the form of the external auditory canal and the patients can enjoy swimming. In this study, we performed CWU mastoidectomy, except in one case. One case involved severe cases of stage III with lateral semicircular canal fistula, which recurred several times. About the number of operations, there are many advantages to performing a double-staged operation.
Silicon sheets can be inserted to prevent tympanic adhesion during the first surgery and confirm the presence of recurrence at the second stage of surgery. Nevertheless, we performed single-staged operations in 89.4% of cases, and the rate of recurrence was only 12.8% in pediatric cholesteatoma cases. This rate was better than that in previous reports [6]. In general, the postoperative prognosis of hearing ability was good in pediatric cholesteatoma, and we were able to obtain a success rate of 81.5%. We performed all the middle ear operations in our department via microscopy using the MES approach. However, in the recent years, the number of operations performed using endoscopy (i.e., TEES) has increased. There are many reports of TEES [9,10], and the effectiveness of MES and TEES has been discussed [11].
In congenital cholesteatoma cases, the matrix of the cholesteatoma may extend to the anatomical blind spaces, including the tympanic sinus or facial recess. In these cases, TEES may be effective [12]. Moreover, TEES should remain in effect in a narrow external auditory canal, such as pediatric cases [13]. The field of TEES is good; however, the surgical procedure is not at all brief, and adverse events increase in inexperienced operators [14]. We use microscopy techniques to open the external auditory canal, such as drilling the anterior wall and finding a good field of anatomical blind spaces. We used an endoscope to confirm whether the anatomical blind spot had persistence of the cholesteatoma matrix. We concluded that a polite dissection of the cholesteatoma matrix under microscopy was the key factor in the low recurrence rate.
Conclusion
We examined 46 cases (47 ears) with cholesteatomas who were diagnosed and operated upon before attending elementary school. In most cases, we could preserve the posterior walls of the external auditory canals and perform single-staged operations. In all cases, we performed the surgeries using microscopy, and we had no cases that required endoscopy. However, we were able to obtain a low rate of recurrence and a good hearing prognosis.
To Know more about Global Journal of Otolaryngology
Click here: https://juniperpublishers.com/index.php




No comments:
Post a Comment