Dermatology & Cosmetics - Juniper Publishers
Abstract
Onychomycosis is the most common nail disease globally, can occur at any age and is related to persistent trauma of the nail, immunosuppression, hyperhidrosis and other risk factors. Onychomycosis can be caused by dermatophytes, non-dermatophyte molds and yeasts. Recent evidence supports the presence of fungal biofilms that protect them from the immune system as well as antifungal drugs. Biofilm may explain fungal resistance and the inability to eradicate fungal chronic infection. Clinically it presents with onycholysis, nail thickening, brittleness and discoloration. This disease can have a negative and significant effect on the quality of life of patients.
Keywords: Onychomycosis; Risk Factors; Dermatophytes; Nails
Introduction
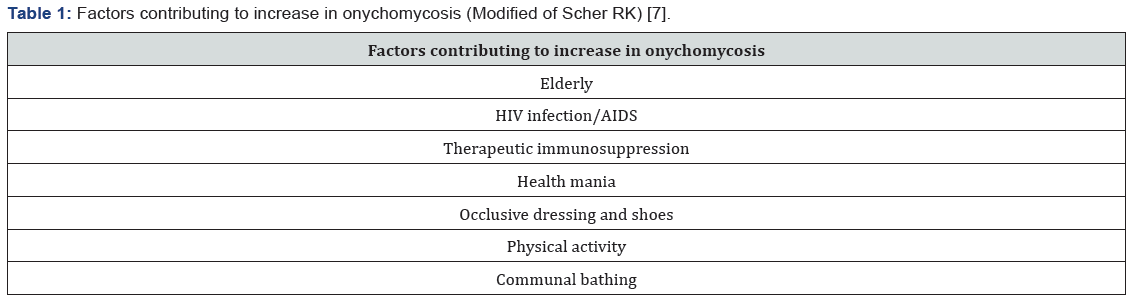
Onychomycosis is the most common nail disease worldwide, accounting for about 90% of toenail and 50% of fingernail infections. The fungal infection leads mainly to discoloration, nail plate thickening and onycholysis [1]. Prevalence increase in the elderly and it reaches all ethnicities with a male predilection (1.5:1) [2,3]. Pediatric cases are increasing, possibly related to childhood obesity and diabetes mellitus [4]. Some known risk factors are the persistent trauma to the nail, human immunodeficiency virus (HIV), immunosuppression, hyperhidrosis and smoking. It is also related to the use of occlusive shoes or synthetic material, poor hygiene and the habit of not drying feet skin properly [5,6]. It is now known that there are some factors that favor the increase of fungal infection of the nails (Table 1). These same factors can lead to recurrence of onychomycosis after treatment, which makes it a challenging and chronic disease.
Etiopathogenesis
Onychomycosis can be caused by dermatophytes, non-dermatophyte molds (NDMs) and yeasts. Around 90% of toenail onychomycosis infections are caused by dermatophytes [8]. The most common etiology in Europe are dermatophytes, typically Trichophyton rubrum followed by T mentagrophytes and T interdigitale [9]. In the United States and Mexico T rubrum is the head agent accompanied by T mentagrophytes [10]. Other less frequent tinea unguium infections are caused by Epidermophyton floccosum, Microsporum spp., T violaceum, T verrucosum, T krajdenii, and Arthroderma spp [11]. Candida albicans and C. parapsilosis are isolated between 8 and 10% and are more likely to be causal in fingernails, especially individuals whose hands are frequently immersed in water [11]. NDMs (1-5%) are predominantly Aspergillus spp., Scopulariopsis brevicaulis, Acremonium spp., Fusarium spp. and Neoscytalidium [7,12]. Although dermatophytes are the most common in onychomycosis, NDMs are being reported more frequently in warmer climates [13,14]. Mixed NDMs-dermatophyte infections are uncommon [15]. Recent evidence supports the presence of fungal biofilms. These are microbial communities, rather than acting as independent spores and hyphae, that attach to biological surfaces, such as the nail plate, via an extracellular matrix (ECM) that encases them. The ECM protects them from the immune system as well as antifungal drugs, physical and chemical removal strategies. Dermatophytes, including T rubrum and T mentagrophytes, NDMs including Aspergillus fumigatus and Fusarium spp. and yeast such as C albicans all form biofilms in vitro. Biofilm may be the reason fungal resistance and the inability to completely eradicate fungal chronic infection [16-19].
Clinical Characteristics
Onychomycosis occurs most often on the feet, with the great toenail most frequently affected. It can present nail separation from the nail bed (onycholysis), nail thickening, brittleness and discoloration (white, yellow or brown). More severe cases may exhibit ingrown nail (onychocryptosis). These symptoms get progressively worse. Dermatophytoma is a fungal mass that presents as yellow, white or brown longitudinal streaks within the nail plate. On the other hand, NDM and yeast infections present usually as yellowish/whitish discoloration [20]. Classification of onychomycosis has five categories established: distal and lateral subungual, superficial white, proximal subungual, endonyx and total dystrophic onychomycosis. Distal lateral subungual infection, the most common form, begins on the distal section of the nail and spreads under the nail bed (Figure 1) [21]. Endonyx is exceptional and involves the nail plate as well as the nail bed. Proximal subungal onychomycosis are less common in the general population, but are the most frequent form in patients with HIV infection and can pose problems because it is more difficult to obtain a good sample for microscopy and culture. White superficial is usually associated with T mentagrophytes rather than T rubrum infection; the sample is relatively simple to obtain and in general has a positive response to topical therapy. Total dystrophic onychomycosis involves the whole nail [22]. Onychomycosis can have a negative and significant effect on the quality of life of patients, both physiologically and emotionally, it can even cause stigmatization and social exclusion. Nail changes can cause pain when walking or standing for long periods, with limited mobility; in addition, it can cause paresthesia, mainly in fingernail onychomycosis. Other negative consequences described are the exacerbation of diabetic foot, acceleration of thrombophlebitis and development of urticaria or dermatophytid reactions [23].
To Know more about Dermatology & Cosmetics
Click here: https://juniperpublishers.com/index.php




No comments:
Post a Comment