Palliative Medicine & Care - Juniper Publishers
Abstract
Background and purpose: A single-center observational study involved the assessment of pain in palliative care patients PC who required surgery. The question was asked: How does acute pain influence the behavioral pain perception in palliative patients treated with opioid drugs before and after surgery.
Materials and methods: Patients who were qualified for surgical procedure and diagnosed with a disease qualifying for palliative treatment were followed up. Acute pain therapy was applied in the ward as in all cardiac surgeries. The diagnosis in the applied pain therapy was not distinguished due to the coexisting palliative disease. All patients received pain medication according to the same schedule. The survey assessed the level of pain sensation and the accompanying emotional states such as anxiety, fear and depression. The standardized and own type questionaries’ has been used.
Results: Based on the analysis of the answers provided, 30% of respondents PC rated their pain, assessed on the 4th day at 7/10, i.e. severe. More than half of the respondents replied that they had new pain ailments. Patients indicated more than one location of the intensity of postoperative pain, but the highest intensity of pain was found at the operated site. The patients indicated the occurrence of anxiety and there was no difference between the anxiety before and after the surgery. When expressed about pain, it can be seen that the elderly complained less about pain than younger people.
Discussion: The conducted studies of behavioural pain assessment in cardiac surgery patients indicate that the overall health condition of the patient should be taken into account in the assessment of pain. It has been shown that patients who have had palliative disease are prone to pain after cardiac surgery procedures and that conventional pain treatment in these patients is not sufficient. Analysis of the collected data provided information on the use of painkillers, pain assessment and how patients cope with emotions after surgery during palliative treatment. The choice of painkillers depends primarily on: the type of pain, its severity, as well as the length of pharmacotherapy and whether the previous analgesic therapy and the drugs used reduced the pain.
Introduction
Palliative patients are a group particularly exposed to pain. Post-operative pain in this condition caused by damage to tissues, intensified by perioperative stress, causes an additional emotional and behavioural response of the system to surgical actions [1]. Regardless of the primary disease, pain after cardiac surgery, and in particular after midline sternotomy, is a strong, critically related to proper ventilation and haemostasis of the circulatory system. Acute pain caused by surgery forces an unfavorable position, which is difficult for the proper respiratory mechanics, leads to atelectasis, worsening of postoperative complications and changes in the perception of pain stimuli, including persistent chronic pain [2]. According to the literature data, properly treated patients without additional comorbidities stop experiencing acute pain a few days after the procedure. On the other hand, the lack of adequate pain treatment after surgery may cause pain to persist for many months after the patient’s discharge [3]. Palliative patients operating in cardiac surgery departments constitute a special, diverse group of patients. Most often, operations are performed on them because of the primary palliative disease or diseases that occurred during palliative treatment. They are in each of these cases particularly prone to pain and are usually treated with anti-pain medications before surgery; therefore, postoperative pain perception may be different in this group of patients. Additional acute pain, insufficiently controlled, has an impact on the partial and / or complete disability of the patient. It is a problem that, if it occurs, will intensify the occurrence of chronic and persistent pain, which causes escalation of the doses of anti-pain medications and limiting the independence and comfort of life [3,4].
Treatment of acute pain in palliative patients
The choice of the drug, as well as its dosage, depends on the intensity of pain and is based on the use of analgesics of increasing effectiveness, as well as supplementing the action of analgesics [5]. According to WHO recommendations, drugs are used in palliative patients according to the analgesic ladder [6]. The first step of the analgesic ladder covers the treatment of low intensity pain on the numerical scale (NRS). In such cases, it is recommended to use non-opioid analgesics (NSPB), which include non-steroidal anti-inflammatory drugs (NSAIDs) as well as paracetamol and metamizole. NSAIDs have an analgesic effect, especially in nociceptive pain. They are more effective than paracetamol and metamizole in counteracting inflammatory pain. In order to improve the effectiveness of analgesia, it is recommended to combine NSAIDs with paracetamol, but never to combine two NSAIDs, as well as paracetamol and metamizole, because they act on similar cyclooxygenase isoforms. NLPB should be administered in doses and at intervals that guarantee effective analgesia. In the case of NSAIDs, the choice of dose and timing of administration is dependent on the drug selected. On the other hand, paracetamol is used in regular 4-6 hour intervals. In the case of NSAIDs, it is worth remembering that drugs have their effect on the activity of COX-1 and COX-2, which may cause differences in the profile of their analgesic effects and the profile of side effects [7].
The second step of the WHO analgesic ladder covers the treatment of pain with a severity of> 4-6. The transition from the 1st to the 2nd and 3nd step of the ladder occurs most often due to the ineffectiveness of drugs in the 1st step of the ladder or in the case of increasing pain associated with the disease [8]. In the case of using tramadol, it should be remembered that due to the serotoninergic mechanism of action of these drugs, they should not be combined with other drugs enhancing the transmission of serotoninergic system due to the risk of serotonin syndrome. Drugs from the 2nd rung of the analgesic ladder should not be combined [9].
Behavioral Aspects of Acute Pain in Palliative Patients
After surgery, pain often reduces the patient’s satisfaction with the procedure performed. Pain delays the patient’s mobilization, increases the incidence of postoperative complications and increases mortality [10]. In patients staying in the postoperative ward, it can cause depression and excessive excitability, fear, and fear of their own health in the future [10]. It is believed that the emotions accompanying the patient have an evident influence on the perception of pain [11]. Patients with additional anxiety and fear experience worse postoperative pain [11].
In the preparatory management of postoperative pain, the general assumptions, recommendations for education and planning of perioperative management in pain therapy after cardiac surgery should be taken into account. It is important that the patient is provided with knowledge about the possibilities of pain treatment [12]. The psychological sensations of a pain stimulus consist of closely related stages. The first stage is sensory-discriminatory experience, while the second stage causes a reaction of pain with a small share of other functions. In the first two stages, it is possible to assess using pain scales such as VAS or NRS. The next stage is the suffering stage, it is related to the patient’s feelings and views on pain [9]. The final stage is behavioral pain expression, also known as conservative pain. This stage determines the patient’s motor activities. The evaluation of the emotions of anxiety and fear of the second stage was carried out on the basis of the answers to the questions included in the survey.
Aim
The study posed the question: is pain sufficiently measured in palliative patients if they are treated according to the regimen typical for patients without palliative disease? Does pain depend on the presence of pre-operative anxiety and depression in postoperative patients? In addition, it was decided to investigate whether the type of pain ailments changes the expression of emotions such as fear, anxiety, anxiety in these patients, and the quality of analgesia was assessed, allowing for the performance of respiratory therapy and other physiotherapeutic procedures.
Materials and Methods
The method of diagnostic survey was used in the study. The survey was conducted anonymously. It was carried out among patients staying in the postoperative ward of the Cardiac Surgery Clinic of the University Teaching Hospital in Białystok. The study involved 50 patients. The study included patients who were on day 4 after surgery. The study included patients with diseases eligible for elective surgery and who were treated palliatively prior to surgery. The research tool was a questionnaire containing questions, as well as elements of the VAS, NRS, PHHPS scale, and questions related to the coexistence of emotions such as anxiety, depression.
The survey was divided into two parts. The first part is sociogeographic questions, while the second is specific questions about pain assessment. The questions contained in it concerned the patient’s well-being and the assessment of the severity of pain after cardiac surgery. The respondents were informed about the purpose and scope of the study and were presented with a consent form to participate in the study. Patients who were aware, in logical verbal contact, were treated on an outpatient basis and in hospital after procedures such as:
a) Patients undergoing cardiac surgery without circulation
b) Patients after operations in extracorporeal circulation not longer than 3 hours
c) Postoperative pain measurement was based on features such as pain intensity, duration and location.
d) Pain was assessed using the VAS and NRS scales.
VAS (Visual Analogue Scale) is a visual scale. The level of perceived pain is marked on a straight horizontal line, and the researcher or subject determines the intensity of pain. When assessing pain, the researcher uses the scale reproduction based on the marked points on the line to indicate no pain symptoms and the strongest pain that the patient can imagine [2,5,6]. NRS Numerical scale - on this scale, pain is rated from 0 to 10 in the 11-point range, where 0 is assigned the sentence “I do not feel pain at all” and 10 is “the worst pain that cannot be imagined” [7,8].
Prince Henry Hospital Pain Score - PHHPS - the scale is applicable after thoracic surgery, cardio surgery and epigastric surgery [2]. 0 - no pain when coughing1 - pain when coughing, but not with deep breathing2 - pain only with deep breathing3 - slight pain at rest4 - severe pain at rest All patients were treated for pain according to PTBB (Polish Association for the Study of Pain) guidelines published on 2018 [6]. Regular opioid infusion of short-acting remifentanil was used for surgery, and patients received fractionated doses of morphine, paracetamol, and NSAIDs after surgery.
The statistical evaluation of the work was performed using the statistics program, on the basis of the questionnaires and the applied VAS scale and the numerical scale [9]. Sociologist E. Babbie claims that a survey is the best method to gather information in a larger group of respondents. It perfectly describes the collected data on respondents [13]. A questionnaire was used to conduct the research. According to the definition of Bauman and Plich, it is “a technique of collecting information consisting in filling out a questionnaire, most often by the respondent, of special questionnaires, usually with a high degree of standardization” [14].
Result
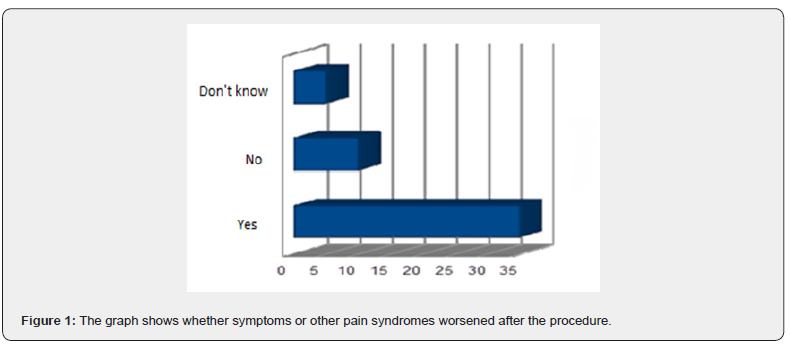
In the group of respondents, new pain ailments occurred in 25 people. Such feelings were not experienced by a smaller group of respondents, as many as 20 respondents. 5 people remained neutral. In the further part of the questionnaire, it was found that 34% of patients report severe pain after surgery, there were affirmative responses, while 40% of respondents stated that they did not experience postoperative pain, and the remaining patients were unable to provide answers. Additionally, when asked about the severity of other pain ailments, as many as 35 respondents out of 50 provided information that other pain syndromes had worsened. On the other hand, as many as 10 respondents gave a negative answer. 5 respondents remained neutral. The results are shown below Figure 1 [15-17].
“Did the pain before the surgery hinder the daily functioning?”
A large group of respondents were people for whom pain hindered their daily functioning. More than half of the respondents, i.e. 28 people, answered that pain is difficult in everyday life. No problems in everyday functioning occurred in 10 people and 12 people chose the answer “I don’t know.” The result is shown below Figure 2 [18].

Was there any fear before the surgery?
A large group were also people who felt fear and anxiety before the surgery, there were 35 of them, which constitutes 70%. Before the surgery, 13 people said that fear and anxiety had no effect on their well-being. Two people answered the question “I don’t know”. To the question “Did the pain cause you fear unknown so far?” The answers among the respondents were as follows: as many as 40 people answered this question in the affirmative, while 10% answered negative (Figure 3) [19].

Do I expect that after the surgery I can get pain treatment that will not hurt me?
Among the respondents, 40 respondents know about the possibility of alleviating postoperative pain. No information on this topic appeared in 5 people. The least numerous answers were “I don’t know” [20] (Figures 4-7).
Collected Results and Discussion
The study answered the questions that standard pain management used in all cardiac surgery patients is not adequate for palliative patients. They need more intensive analgesic therapy. Standard pain therapy used routinely in the ward is not sufficient for palliative patients. Patients suffer from pain especially between 2 and 4 days after the procedure. The question whether surgery and pain increase depression in palliative patients has not been resolved. The stay in the ward and the pain will increase the anxiety felt by the patients [21-23].
Pain and surgery have not been shown to influence depression when assessed shortly after surgery. The greatest pain was recorded on the fourth day after the cardiac surgery. This is due to the fact that the respondents suffer from postoperative pain related to the performed procedure and it is perceived differently than in non-palliative patients who, according to the literature data, have the worst pain on the 2nd day after surgery. Pain is related to the place where the drains are led out or where the wound is cut. Pain intensity in cardiac surgery is the highest among all the types of pain in surgery described so far [24-27].
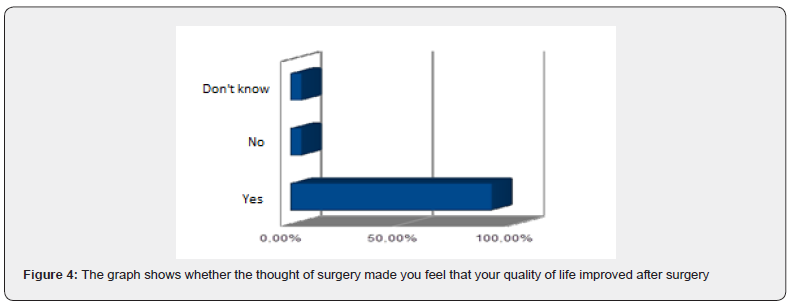

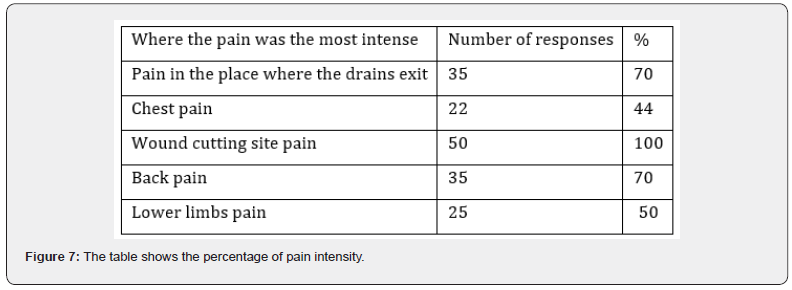
Numerous studies show that most often, as in our work, that: The indicated areas of pain after surgery are the medial part of the chest, i.e. the area of the postoperative wound, the area where the mediastinal and pleural drains are introduced. The group of respondents stated that the operation would improve their quality of life. There was no evidence of an increase in the drug after surgery despite pain. High doses of drugs used in cardiac surgery and the need for deep anesthesia reduce the level of anxiety due to pain. The group of subjects required the use of higher doses of pain medications. When the pain was stronger, respondents reported the need for a higher dose of pain medication. The variety of methods used to relieve pain and the techniques used were not effective enough. Pain therapy is based on the close collaboration of an interdisciplinary team. A nurse may give you a pain reliever as needed. In the first few days, the painkiller is administered on medical prescription, according to the hours indicated; in case of prolonged acute pain, the rescue dose should be adjusted. The drug should be administered by the most convenient route for the patient, in the case of cardiac surgery patients it is usually central access. The selection of agents should consider the analgesic ladder, ranging from the less active drug to the more potent drugs [28,29].
Pain in almost 90% of respondents caused unknown fear. Anxiety is a sensation that can be attributed to a high level of negative affect and a fear of possible danger or threat and a feeling of being unable to predict and control them. Trait anxiety can be viewed as a motive or acquired behavioral disposition through which an individual may perceive non-threatening situations as threatening, thereby reacting to them with drug states that are not actually equivalent to them. The tendency to anxiety reactions may cause higher levels of anxiety and depression in the perioperative period. Pain can be a sensitive, early sign of fear, especially in patients who have undergone cardiac surgery. Preoperative fear associated with the procedure, awareness of possible complications, general anesthesia and the patient’s mental attitude increase the anxiety. Pain sensations after the procedure increase anxiety in a large number of patients, which contributes to the intensification of anxiety or fear, which results in an extended recovery time. With each scale, we can evaluate pain after cardiac surgery. The VAS scale positively correlates with each other in zero and in the following days the possibility of assessing pain. An important point is pain monitoring in the intensive care unit is possible with all pain characteristics. Post-operative pain impairs cognitive processes and limits the possibility of performing physiotherapeutic procedures. Weakened mental functioning extends the recovery period and, after surgery, deteriorates functioning. Currently, the best-known risk factors for disturbance of consciousness are old age, previous stroke, renal failure, obliterating arteriosclerosis of the lower extremities, and somatic stresses such as atrial fibrillation. The study showed that patients diagnosed with palliative disease are very sensitive to acute pain caused by surgery. Severe pain occurs in 30% of them and in more than half of patients there is pain that requires above-standard treatment.
The conducted studies of behavioral pain assessment in cardiac surgery patients indicate that the overall health condition of the patient should be taken into account in the assessment of pain. Analysis of the collected data provided information on the use of pain medications, pain assessment, and how patients cope with emotions after cardiac surgery. A significant part of the respondents experienced chronic pain of a significant degree, and the number of these people increased significantly with the age of the respondents.
Cardiac surgery procedures are a type of large and very extensive procedures. The duration of the treatments, the way they are performed, and pharmacotherapy have a great impact on the patient’s condition. Pain after cardiac surgery is one of the strongest postoperative pains. Pain requires a large contribution of medical personnel and a large amount of pharmacotherapy to improve the patient’s feelings. More pain medications are sometimes needed to improve the quality of life of patients after cardiac surgery and to relieve pain.
In our study, pain was examined on the 4th day after surgery, where severe pain was found in a significant number of patients. 7/10 Failure to treat it causes a number of complications, including unsuccessful surgery. Pain is also influenced by the extent of the procedure and the degree of tissue cutting [2]. We believe that the studied group of palliative patients is especially prone to pain due to the specificity of end-stage disease. Although few people die of pain, many die in pain and still more live in pain. The psychological perception of a stimulus consists of four closely related stages. The first and second stages can be assessed using simple scales, for example the VAS visual-visual scale. The first stage is a sensory-discriminatory experience, which in the second stage causes a distress reaction with a small share of cognitive functions. The third stage is suffering, which is a more complex phenomenon related to the patient’s views on pain, including complex reactions such as depression, anxiety, anger. This stage is shaped by personality traits, ways of coping with pain, experiences. The fourth stage is the behavioral expression of pain, otherwise known as the pain behavior. It is determined by motor efficiency and daily activities [10].
Nowadays, we can observe an upward trend in the willingness to learn about the possibilities of analgesic therapy before surgery. This reduces stress levels, anxiety and the occurrence of depression. In our study, the patients were aware that pain medications could be used to prevent pain. Most of the patients expected them not to be hurt. In the further part of the questionnaire, it can be stated that patients report pain after surgery, and thus one of the factors hindering recovery is the feeling of pain in various parts of the body. Difficult contact with the patient causes mood swings, disturbances of the circadian rhythm, delayed convalescence. Most of the answers were affirmative [26]. On the other hand, 10% of respondents stated that they did not experience postoperative pain.
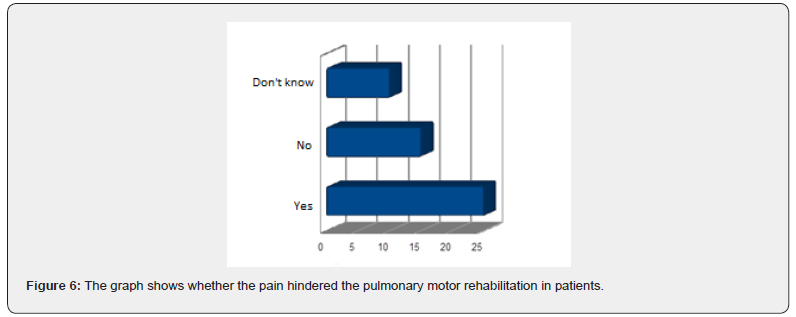
It was shown that the occurrence of pain significantly limited the possibilities of rehabilitation. According to the literature, this has a significant impact on the recovery period after surgery. The study considers that the use of early rehabilitation shortens the postoperative period and reduces the number of pulmonary complications. The main task of cardiac rehabilitation is to consolidate the results of conservative, interventional or surgical therapy by stopping the disease progression, restoring the lost psychophysical fitness and facilitating the return to active life [20]. Due to the modern surgical techniques currently used, the performance of procedures in increasingly elderly people, who were previously disqualified due to the high risk of surgery, more and more patients require rehabilitation [21,22]. Patients qualified for cardiac surgery differ in the degree of risk. One group consists of elderly patients with multivessel lesions, concomitant diabetes mellitus and symptoms of heart failure. The second group consists of patients with lower risk, young people with isolated, but not eligible for angioplasty, lesions in the coronary vessels, without heart failure and comorbidities. It is associated with a different preparation of the patient for surgery, the risk of the surgery itself and postoperative treatment, including rehabilitation [23].
In the perioperative period, the most important improvement procedure is the activation of the mechanisms of proper lung ventilation by breathing exercises: 4-track (upper costal, lower costal, diaphragmatic, left and right chest side), the bronchial tree toilet (positional drainage, learning effective coughing and expectoration, breathing exercises with water bottle, flutter, etc.); placing the lower limbs from which the material for transplantation was made in a position that facilitates the outflow of blood; reducing the tension of the abdominal press during isometric efforts and changes in position from lying down to sitting and vice versa; active exercises of the upper and lower limbs (coordination of movement with breathing); active lower limb exercises for thromboprophylaxis; starting a sick person and preparing for self-service; isometric and relaxation exercises [23- 25].
Working with a patient with acute pain and palliative disease requires professional knowledge of how to relieve pain, support and demonstrate understanding in proportion to the patient’s condition. The interdisciplinary team must be aware that physical suffering affects the mental sphere [17]. Therefore, as pain after cardiac surgery is one of the most severely felt types of pain, especially in the first few days, treatment should be started to relieve pain as effectively as possible until full consciousness is regained upon recovery from general anesthesia. Opioids (mainly morphine, tramadol) and drugs such as paracetamol, pyralgine, and ketoprofen are the best [18,19].
The nurse’s participation in the treatment of postoperative pain is based on her preparation for the care of a pain patient. In Poland, such patients may be cared for by nurses who have completed a qualification course or specialization in anesthetic and intensive care nursing, or a specialist course in acute pain therapy in adults. Education increases knowledge about pain and encourages patients to participate in pain management. It should cover analgesic methods, methods of pain measurement, establishing an analgesic action plan, and explaining the importance of honesty in pain assessment and treatment for overall therapy success [14,15]. Assessing acute pain care is difficult because pain is a subjective symptom that people perceive differently. After surgery, insufficiently treated pain may cause prolonged suffering, rehabilitation, aggravate depression and anxiety, and affect the occurrence of postoperative delirium; it may increase the number of complications [16].
Conclusion
The analysis of the collected results and the conducted research led to the following conclusions. In our work, severe postoperative pain occurred on the fourth day after the surgery in palliative patients undergoing cardiac surgery. We believe that palliative patients are more prone to pain than the group of patients without comorbidities. The pain concerned the operated site, especially the chest, and it was shown that the occurrence of pain significantly limited the possibilities of rehabilitation, especially increasing the risk of pulmonary complications. Monitoring and assessment of pain in the postoperative department is possible using the VAS scale. The conducted studies allow for the behavioral assessment of pain in patients after cardiac surgery, it has been shown that the pain did not change the level of the drug after surgery in palliative patients.
To Know more about Palliative Medicine & Care
Click here: https://juniperpublishers.com/index.php




I wasted a lot of money trying to find the right medication for my moms dementia all to no avail until Dr Erayo showed up and eradicated the stigma with the natural roots and herbs i ordered from him , my mom took it for 21days and she was cured from her dementia.
ReplyDeleteGod have use Dr Erayo herbal home to cure my mom, thank you so much Dr Erayo I am so happy. You can email Dr Erayo for help drerayoherbalhome@gmail.com
or whatsapp him on +2348151937428
website---- https://alternativeherbs.weebly.com
Youtube link---- https://www.youtube.com/channel/UCSp2m-_EHnCRQT4gYYTQWtg
FB page---- https://rb.gy/yuofn6
Wow, that is quite informative. I like this article very much. The content was good. If any of the engineering students are looking for a projects for vanet projects, I found this site and they are providing the best service to the engineering students regarding the projects vanet projects
ReplyDelete