Global Journal of Nanomedicine - Juniper Publishers
Abstract
Triage system is a process that is critical to the effective management of modern emergency departments. The triage systems aim not only to provide a fair clinical evaluation for the sick, injured and poisoned children, but also to provide a good effective approach to the organization, monitoring and evaluation of emergency medical care in the pediatric emergency departments Over the past 20 years in the world and in Europe, triage systems have been standardized in a number of countries and are making efforts to ensure sustainability of compulsory implementation. In addition, differences at international levels in triad systems, but limits capacities to benchmark standards.
The purpose of this paper is to enable pediatric emergency pediatric healthcare professionals to quickly evaluate, monitor, treat, and transport medical care, and to understand, learn, and apply the newest guidelines of the triage system with priorities. The research of the paper aims to make pediatric emergent medical care professionals in hospital settings to do a fairly fast triage, reducing morbidity, invalidity and mortality in the pediatric emergency department at the hospital. Triage systems in our country at three levels of health care do not work, is a chaotic system because there are no clinical guidelines, algorithms important component should create mandatory triads in three health care providers, advancing, strengthening the triad system as an important component of health care. Education, training of professionals of health care professionals for the three levels of health care should be an obligatory component to increase the quality of emergency medical care in life-threatening children. It’s time to develop and test a triad scheme that will be based on a triad system that will respond and adapt to the conditions of our health system.
Keywords: Triage; Pediatrician; Seriously Ill Critical Children; Convulsive Attacks; Shock; Health Care; Clinical Signs; Life Threatening
Introduction
Pediatric emergency triage system and emergency medical care is a process that is critical to the effective management of modern emergency departments [1]. Trial Systems aim not only to provide a fair clinical assessment for sick, injured and poisoned children, but also to provide a good effective approach to the organization, monitoring and evaluation of emergency medical care in pediatric emergency departments. Over the last 20 years in the world and in Europe, triage systems have been standardized in a number of countries and are making efforts to ensure the sustainability of enforcement [2]. In addition, differences at international level in triage systems but limit the capacity to benchmark. The country-level triage system in chaotic, disorganized Kosovo does not function as a synchronized system but there is no official standard, normative tri-level triage system for health system organization [3].
WHO Emergency triage, assessment and treatment guidelines are used to identify children with life-threatening problems who present with signs and symptoms that should be treated as medical emergencies. But the Kosovo Ministry of Health should bear in mind that this important component should create mandatory triage standards in the three health care needs. It also needs advanced, empowered EMEA and the triage system as an important component of healthcare with education, education, training of health care professionals to enhance the quality of emergency medical care for children at risk.
Purpose of Work
The purpose of this paper is to enable and enable pediatric emergency health care professionals to do rapid triage, assessment, monitoring, treatment, and transport with medical care. To understand, learn, apply the newest triage system guidelines with priority by reducing morbidity, disability and mortality in the hospital pediatric emergency department.
Material and Methods
The research material was obtained from the Children’s Clinic archive at the UCCK Pediatric Emergency Department for the period January - December 2016. The research is retrospective, descriptive, and qualitative. 17 years of age with acute lifethreatening illnesses by researching the pattern of triage, gender, age, place of residence, seasons of the year, monitoring, observation, diagnosis, treatment, complications, referral and education of pediatric emergency medical professionals [4-8]. The sample surveyed 220 cases of children with triad of lifethreatening life-threatening illnesses by pediatric emergency medical professionals with serious illnesses such as febrile convulsive attacks, severe dehydration, hypoxemia, pneumonia, shock, metabolic problem, respiratory distress, cardiac arrest, electrolyte imbalance. Description of data processing Description of data processing is performed statistical parameters, (worked out Exel Word) structure index, arithmetic mean and standard deviation. Statistical tests: X2-test and T-test. Test verification was done for the 95% and 99% confidence levels, respectively for p <0.01 and p <0.05 [9-11].
Results
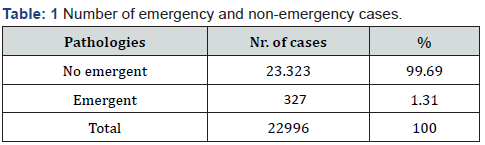
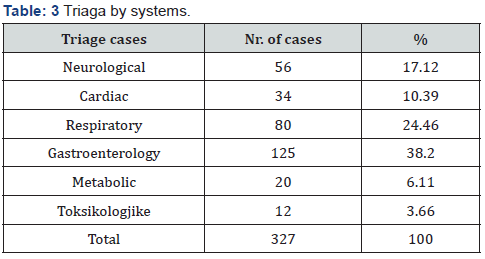
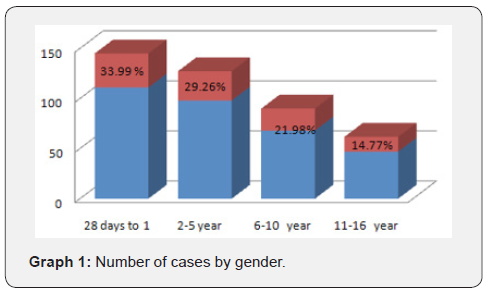
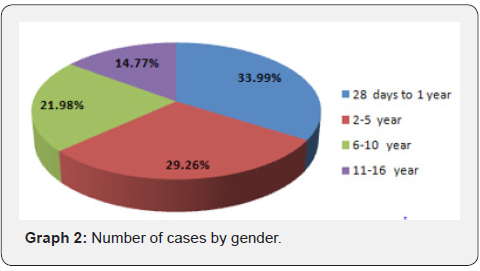
The research material was obtained from the Children’s Clinic archive at the UCCK Pediatric Emergency Department for the period January - December 2016. The research is retrospective, descriptive, qualitative. Only 28-day-old babies up to the age of 17 with acute life-threatening illnesses treated in Department of Pediatric Emergency of UCCK in Prishtina, out of the total number were 23,320 cases 99.69%, and of them were 327 emergency cases or 1.31%. (Table 1). The average age of the patients included in the study was 1-10 years; the youngest patient was over 28 days and the oldest was a child 16 years (Graph 1) (Table 2) . From the total number of 327 children affected by child sex, male cases were 177 cases or 54.12% and female children 150 cases or 45.88%. (X2- test = 39.4, P <0.001), (Graph 2). The average age of the patients included in the study was 1-10 years; the youngest patient was over 28 days and the oldest was a child 16 years. (Graph 2). Number of cases according to systemic acute life-threatening diseases Neurological 56 cases or 17.12%, Cardiac cases 34 or 10.39%, Respiratory cases 80 or 24.46%, Gastroenterology 125 cases or 38.2%, Metabolic 20 cases or 6.11%, and Toxicological cases 12 or 3.66 % (Table 3).

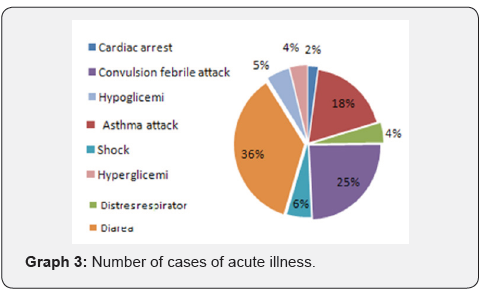
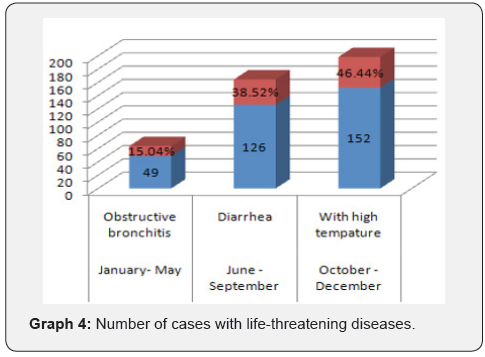
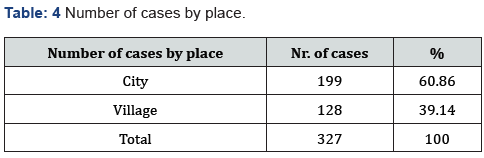
Number of cases with acute illnesses, children with cardiac arrest 7 cases or 2.23%, asthmatic attack 60 cases or 16.43%, respiratory distress 14 cases 4.22%, convulsive febrile attack 80 cases or 25.43%, shock 18 cases or 5.50%, Diarrhea 118 cases or 36.08%, Hypoglycemia 17 cases or 5.19%, Hyperglycemia 13 cases 4.92% (Graph 3). Number of cases that required emergency medical services with life-threatening illnesses by month of the year [12-16]. January-December with obstructive bronchitis were 49 cases or 15.04%, June-September with diarrhea were 126 cases or febrile conditions were 152 cases or 46.44%. (Graph 4) (Table 4). According to the place of residence, the largest number of cases of potentially life-threatening children were from the city 199 cases or 60.86% and from the village were 128 cases or 39.14% Table 7 (Graph 5). Of the 327 cases reported, only 18 or 5.50% of them were in shock, whereas hypovolemic cases were 8 cases or 44.49%, cardiogenic shock 3 cases or 16.6%, vasodilator shock 2 cases or 11.11%, allergic reactions anaphylactic 1 case or 5.54% and with septic shock 2 cases or 11.19% (Graph 8).
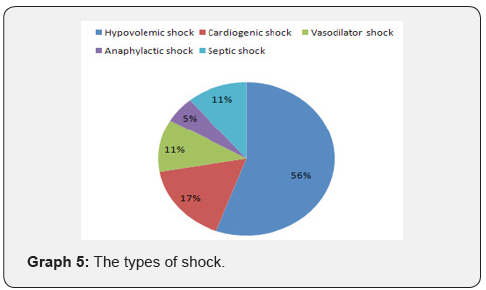
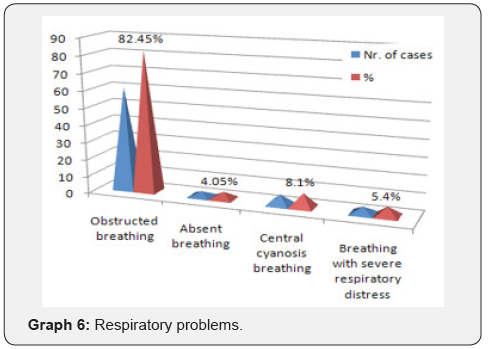
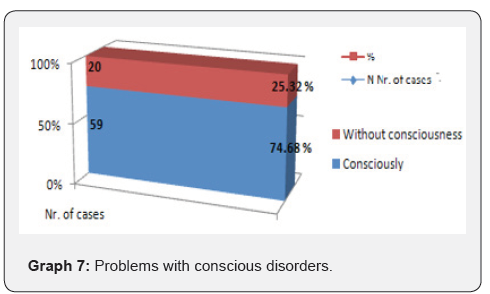
Triage and management of pediatric cases with life-threatening and circulatory injury signs determined based on three clinical criteria such as cold hands and extremities or capillary refills> 3 s and with poor and rapid pulse in all children with these clinical signs have been categorized in children with shock or circulatory impairment [17-21] (Table 5). The number of shock cases defined by three clinical criteria of 18 cases of children with any of the clinical signs of children with cold extremes were 4 cases or 22.23%, capillary duration> 3 s 6 cases or 33.33 and with poor and rapid pulse 8 cases or 44.44% (Table 9) (Graph 9). Children with multiple clinical manifestations of shock may be evaluated in settings restricted by non-specialist healthcare professionals, only with the presence of three clinical signs, and the presence of one or two of these signs indicates a nonspecific impairment of blood circulation that may be due to conditions different from circulatory disorders [22,23] (Graph 6). The total number of 327 cases of them with Respiratory or Obstructive Problems, Absence, Central Cyanosis and Severe Respiratory Disturbances were 74 cases or 22.62%, of them with Respiratory Impairment 61 cases or 82.45%, Respiratory missing 3 cases or 4.05%, central cyanosis respiration 6 cases or 8.10% and respiratory distress respiratory distress 4 cases or 5.40% (Table 9 Graph 9) (Graph 7).


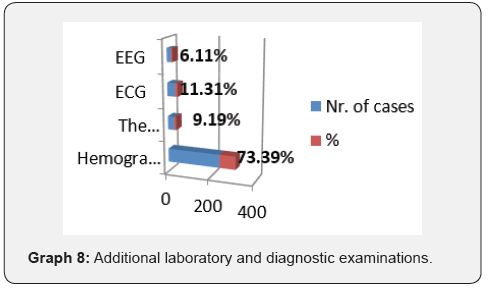
(Graph 7) The total number of 327 cases was 79 cases or 24.15%, with problems of consciousness disorders, whereas 59 cases or 74.68% with consciousness problems and 20 cases or 25.32% with no consciousness problems (Table 6). The total number of 327 cases out of them 118 cases or 36.08%, children with signs of severe dehydration, defined as the presence of diarrhea or any other dehydration condition were with vomiting or insufficient fluid intake 63 cases or 53.40% , with fever were 41 cases or 34.74% and with lethargic or unconscious signs, eyes in orbit, cold skin less capillary filling (> 2 s) were 14 cases or 11.86% (Table 6) (Graph 8). Out of a total of 327 children screened, monitored, observed, diagnosed and treated only needed additional laboratory and diagnostic examinations, biochemical and hematological analysis (hemogram electrolytes, glycemia, urea, creatinine), were 240 cases or 73.39%, Function. lumbal 30 cases or 9.19%, ECG 37 cases or 11.31 and EEG 20 cases or 6.11%.
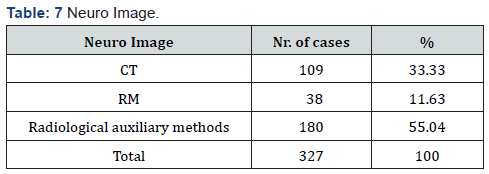
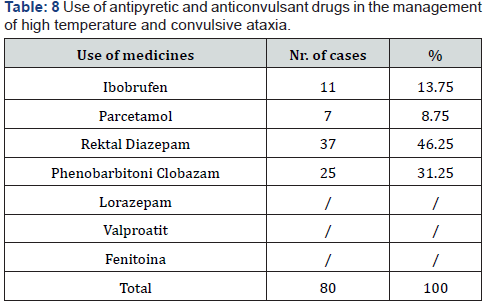
Blood tests for glucose and sodium recommend that routine blood glucose measurement is not required for all children with febrile convulsions and as the information for the diagnosis from blood cultures of children with febrile convulsions does not differ much from that obtained in the pediatric emergency departments. Of the total number of 327 cases in children is the needed CT scan 109 cases or 33.33%, Magnetic resonance 38 cases or 11.63%, and Radiologic Assist 180 cases or 55.04%. X-ray imaging, computed tomography (CT) or magnetic resonance imaging (MRI), but although CT and MRI devices are often not available in secondary care settings, X-ray skull management is useful in the diagnosis of febrile attack (Table 7) (Graph 5). Use of antipyretic and anticonvulsant drugs in the management of high temperature and convulsive ataxia. The use of antipyretics and anticonvulsants with Ibuprofen were 11 cases or 13.75%, Paracetamol 7 cases or 8.75%, Diazepam rectal shin 37 cases or 46.25, Phenobarbitone Clobazam 25 cases or 31.25%, and drugs respectively. others such as Lorazepam, Valproate, and Phenytoin which are not used at all due to the absence of these drugs (Table 8). The administration of infusions and medications during CPR is considered an important component of critical emergency care of infants and children with serious illness, and fluid use within the first 1-2 hours after initial evaluation.
Isotonic solutions were treated 195 cases or 60.63%, Isotonic solutions containing salt and sugar (NaCl 0.9% and Glucosum 5%) treated 70 cases or 21.8%, hypotonic solutions 0.45% NaCL 0.45% with 5% glucose were treated 12 cases or 4.03%, Adrenaline glucose treated 12 cases or 4.03%, Adenosine treated 7 cases or 2.14%, Amiodarone treated 9 cases or 2.75%, Diuretic treated 12 cases 4.03%, and Verapamil 10 cases or 3.05% were treated (Table 9). Of the total number of 327 cases required was masked oxygen administration in 34 cases or 10.39%, 146 cases monitored or 45.64%, unchecked 20 cases or 6.11%, masked oxygen delivery 36 cases or 11.%, intubated 7 cases or 2.14%, RKP 7 cases or 2.14%, respiratory oxygen delivery 7 cases or 2.14%.
Of the total number of 327 cases with emergency medical care, advanced life care treatment were 575 cases or 17.43%, and treatment with basic medical life care was 270 cases or 82.57%. From the total number of 327 cases with complications were 123 cases or 37.69%, without complications 207 cases or 63.31%. Number of cases after admission, monitoring, observation, medical diagnostics, medical consultations, out of 327 cases hospitalized were 305 cases or 93.27%, after emergency treatment were left home for further treatment. 12 cases or 93.27%. Immediate treatment begins when rapid triage is made and life-threatening medical problems are identified such as: airway, respiratory and circulatory evaluation, ABC in case of injuries, and circulatory diseases, airways and respiratory tract CAB).
Discussion
Over the last 20 years in the world and in Europe, triage systems have been standardized in a number of countries and are making efforts to ensure the sustainability of enforcement. But important, however, are the three most common emergencies such as: respiratory distress (hypoxemia), severe circulation (shock), and consciously disordered convulsive attacks and rapid onset by utilizing triage priorities and a more acceptable model for the country. No uniform triage system exists in the United States (USA), this creates a widespread dilemma of assessing the sick and injured, and each region has its own US emergency medical service network. The lack of a uniform system in the US is in contrast to other industrialized countries such as Canada and Australia. Formation of methods that integrate field and hospital needs will support an emergency medical service system that ensures the best continuity of care.
Nursing (IT) nurses need to adapt the approach and assessment based on the child’s chronological and emotional age, especially when feelings and emotions can predominate and capable of expressing themselves. Barriers exist during nursing triage such as age, very young, older persons generally present more difficulties for inexperienced nurses. Non-hospital and hospital systems - In pre-hospital and hospital settings emergency nursing triage aims to determine the priorities of treatment and transportation of the sick and injured. Design principles and protocols must be developed and promulgated by the appropriate medical authorities. In case of major disasters: earthquakes, floods, fires, severe traffic accidents, mines, where a large number of people can be injured within a short period of time, it is difficult to properly trace because working conditions are similar to those of war
Assessing infants and children is a major challenge but these should be assessed as life signs as in an adult, with except the pulse will drop. in the brachial artery and not in the radial artery. Assessment of vital signs monitoring and recording, detailed examination of the body. A child who is upset, crying or screaming or examining the chest and abdomen will be difficult. But using games or entertaining can help the nurse’s nurse to assess breathing rhythm. The trauma nurse in children should never forget the vital signs, all of which can be recorded on the scene and the triage rooms in the priority cards. From this triage, patients can be sent to treatment rooms according to the severity of the disease. Limited space in the treatment area can cause the triage nurse a lot of problems with labeling priorities which may be incorrectly applied to the waiting room, so a quick retrofit should be done
Rapid triage and rapid, aggressive fluid resuscitation is the basis or cornerstone in hypovolemic and septic shock management; concluding that fluid boluses were potentially harmful to children with signs of severe circulatory damage including shock shock International guidelines and training courses such as advanced life support for children (Mackway-Jones et al., 2005. 2010. 2015) and advanced pediatric life support (Fuchs et al., 2007) provide criteria for clinical signs that if present indicate that a child is in ‘shock’. Febrile seizures are the most common childhood attacks, occurring on average in 4% of children. Three-tiered healthcare systems in our country do not work is a chaotic system because there is a lack of clinical guidelines, algorithms and protocols to make a correct pediatric triage system. It is high time to develop and test a triage scheme or model that will rely on a responsive triage system adapting to the conditions of our health system.
Conclusion
Health care institutions should develop and test an adaptable triage scheme that will rely on a triage system that will respond to and adapt to the conditions of our health system. Department of Pediatric Emergency of UCCK in Prishtina, out of the total number were 23,320 cases 99.69%, and of them were 327 emergency cases or 1.31%. The median age of the patients included in the study was 1-10 years; the youngest patient was over 28 days and the oldest was a child 16 years. From the total number of 327 children affected by child sex, male cases were 177 cases or 54.12% and female children 150 cases or 45.88%. (X2-test = 39.4, P <0.001. Number of cases with acute illnesses, children with cardiac arrest 7 cases or 2.23%, asthmatic attack 60 cases or 16.43%, respiratory distress 14 cases 4.22%, convulsive febrile attack80 cases or 25.43%, shock 18 cases or 5.50%, Diarrhea 118 cases or 36.08%, Hypoglycemia 17 cases or 5.19%, Hyperglycemia 13 cases 4.92%. The number of shock cases defined by three clinical criteria of 18 cases of children with any of the clinical signs of children with cold extremes were 4 cases or 22.23%, capillary duration> 3 s 6 cases or 33.33 and with poor and rapid pulse 8 cases or 44.44%.
The pediatric emergency department triage rooms should be operational and supported with medical equipment, drugs, medical supplies and assistive devices based on international standards of triage. The Ministry of Health of Kosovo should bear in mind that this important component should create a model of training for the needs of our country, standard clinical guidelines, algorithms and protocols to make a correct pediatric triage compulsory triage system correctly. health care, by advancing, strengthening the triage system as an important health care component Education, education, training of health care professionals for the three levels of health care should be an obligatory component to enhance the quality of emergency medical care for children at risk. It is high time to develop and test a conceptual triage scheme or model that will rely on a triage system that responds to the conditions of our health system.
Recommendation
Institutionally support the advancement and empowerment of the triage system as an important component, the necessary pediatric emergency triage rooms. Develop clinical guidelines, algorithms and triage protocols at the three levels of health care. All health care professionals must be educated, trained in ongoing coaching, communication courses, Paediatric basic life support- AED, Pediatric Advanced Life Support, International Trauma Life Support.
To Know more about Global Journal of Nanomedicine
Click here: https://juniperpublishers.com/gjn/index.php



No comments:
Post a Comment