Gerontology & Geriatric Medicine - Juniper Publishers
Abstract
Objectives: Lack of knowledge about geriatric
conditions is a barrier that prevents older minority populations from
receiving optimal healthcare. We aim to develop an educational
initiative to improve the knowledge gap on cognitive dysfunction in
three target populations: older minority community members, their
caregivers, and healthcare professionals (HCPs).
Methods: A nested mixed-methods with an
interventional pre-post assessment approach was used for this
community-based educational initiative. Educational sessions on memory
loss were developed and conducted. 182 community members, 63 caregivers
and 133 HCPs participated. Pre-posttest questionnaires and qualitative
data were collected to measure the impact.
Results: The results showed significant
improvements in knowledge in all three participant groups. The
qualitative comments showed improved understanding and intentions to
change.
Discussion: Development of an educational
program on cognitive dysfunction targeting community members, caregivers
and HCPs who take care of older patients is feasible in underserved
community and clinical settings.
Keywords: Cognitive dysfunction Educational initiative Ethnogeriatrics Older minority populations
Abbrevations:
MCI: Mild Cognitive Impairment; HCP: Health Care Providers; HRSA:
Health Resources and Services Administration; MSK: Memorial Sloan
Kettering Cancer Center; GRIP: Geriatric Resource Interprofessional
Program; CBOs: Community-Based Organizations
Introduction
One important public health dilemma is the
multi-layer challenge associated with the care of the older adult,
specifically focused on cognitive health. The US population is getting
older and growing more racially diverse. The number of racial/ethnic
minority populations has increased from 46 million in 1980 to 83 million
in 2000, with an estimated increase to 157 million by 2030 [1].
Minorities and older adults represent an intersection of populations
that are particularly vulnerable to suboptimal care. The causes are
complex and focus on racial and ethnic disparities in health resulting
from socioeconomic status, unequal access to care, differences in
behavioral, environmental and genetic risk factors, and social and
cultural biases that influence the quality of care [2]. Moreover, ageism
tends to reinforce social inequalities as it is more pronounced towards
poor people or those with dementia [3]. An estimated 5.4 million
Americans have Alzheimer’s disease, and by mid-century, this number is
projected to grow to 13.8 million [4]. Today, someone in the US develops
Alzheimer’s disease every 66 seconds. By 2050, one new case of
Alzheimer’s is expected to develop every 33 seconds, resulting in nearly
1 million new cases per year [4]. Studies have shownthat more years of
education is associated with a lower risk for dementia [5]. It is no
surprise that dementia afflicts minority populations more than
Caucasians; African Americans are twice as likely, and Hispanics are
about one and one-half times as likely, to have Alzheimer’s or other
dementias compared to Caucasians [6]. Several barriers to addressing
cognitive dysfunction exist within both the older and minority
populations. These barriers include poverty, lack of transportation,
illiteracy, cultural taboos regarding dementia and poor communication
[7-9]. For example, in New York City (NYC), 23% of the population is
categorized as having low-English proficiency. Many people in the community with Mild Cognitive
Impairment (MCI) and Alzheimer’s disease do not recognize cognitive,
functional or behavioral impairment as abnormal [10]. This lack of
understanding can have serious effects on health, and because they or
their caregivers cannot recognize and acknowledge the deficits, they do
not seek treatment. Daily functioning may be compromised because they
lack adequate judgment of situations [11]. Enough education needs to be
given to those affected and to the community at large to aid in
preventive care and to improve understanding of early diagnosis and
disease management.
Caregivers play a crucial and physically, mentally and
emotionally demanding role in the management of patients with
serious chronic diseases. People with dementia typically require
more supervision, are less likely to express gratitude for the help
they receive and are more likely to be depressed. These factors
have been linked to negative caregiver physical and psychosocial
outcomes [12]. Family caregivers often feel unprepared to provide
care, have inadequate knowledge to deliver proper care, and
receive little guidance from the formal health care providers [13].
Family caregivers may not know when they need community
resources, and then may not know how to access and best utilize
available resources [14]. Without this support, caregivers often
neglect their own health care needs to assist their family member,
causing deterioration in the caregiver’s health and well-being
[15].Despite the growth in the older population, there is an unmet
need in healthcare workforce to take care of these patients’ needs.
While the demand for physicians specialized in the medical care of
older adults is increasing, the interest among medical students for
a career in geriatrics is slow to follow [16]. Though the coverage
of geriatric topics at medical schools is increasing, students still
express significant reservations about their abilities to treat older
patients. In one national survey, only 27 % of graduating familypractice
residents and only 13% of graduating internal-medicine
residents felt very prepared to care for nursing-home patients.
Although a large majority of graduating psychiatry residents felt
very prepared to diagnose and treat delirium (71%) and major
depression (96%), only 56% felt very prepared to diagnose and
treat dementia [17]. In this paper, we examine the role held by
three specific groups of people in the care of cognitive health
in underserved ethnically diverse populations: the older adult
community members themselves, their caregivers, and the health
care providers (HCP) taking care of them. Each role has significant
opportunity in improving knowledge and in understanding the
disease and its appropriate management. We focused our efforts
on a large-scale educational program to address these gaps in
knowledge, focusing on cognition in older adults, for all three
groups.
Methods
Team development
The Health Resources and Services Administration (HRSA),
an agency of the U.S. Department of Health and Human Services,
is the primary federal agency for improving health care to people
who are geographically isolated, and economically or medically
vulnerable. Through the Geriatric Workforce Enhancement
Program (GWEP), HRSA provides funds to improve the healthcare
of older adults through education and training. With the GWEP
award, the Geriatrics service at Memorial Sloan Kettering Cancer
Center (MSK) established the Geriatric Resource Interprofessional
Program (GRIP). The GRIP team serves as content experts and a
teaching core that includes representation from occupational and
physical therapy, pharmacy, nutrition, medicine, nursing, social
work, psychiatry, immigrant health and members from the GRIP’scommunity and clinical partners that serve community-dwelling
older adults in culturally diverse and medically underserved areas.
The community-based organizations (CBOs) and clinical sites are
experts in the populations they serve. Team members teach each
other about their respective professions, context, and its unique
relevance in the health management of the older adult during the
process of developing appropriate community, caregiver and HCP
educational material. Via GRIP, multiple professionals’ expertise
and perspectives are infused into one educational program
targeted for each audience.
Target population
We targeted three groups of learners: older community
members, caregivers, and HCPs. All participants were selected
by convenience sampling. Older adults were accessed through
regular attendance to community programs in the NYC area,
partnered with GRIP. The NYC boroughs of Queens and
Brooklyn were targeted for their ethnic diversity to cater to the
underserved. The borough of Queens in NYC is the most ethnically
diverse urban area in the US with 74% of the population being
Hispanic, African American or Asian and 48% being foreign
born. The borough of Brooklyn is about 34% African American,
13% Asian and 19% Hispanic or Latino with about 36% of the
population being foreign born [18]. The partner CBOs marketed
for the educational programs through phone calls, digital and
print advertising, and through in person reminders at other
educational programs. Caregivers were approached through CBO
staff who targeted invitations to this caregiver-client group. Digital
and print marketing were also utilized for the caregiver audience.
HCPs included residents and fellows in training, attendings,
nursing staff including nurse practitioners, and social workers.
Sessions for staff were conducted at scheduled educational
settings, like monthly staff training and conferences at NYC area
hospitals. Participation in the sessions and completion of related
assessments were voluntary and explained as such by site staff
with the help of interpreter(s) if needed.
Content development and implementation
Across all content development, the GRIP team used the
Patient Education Materials Assessment Tool -A/V (PEMAT)
[19] to rate the content’s understandability and actionability.
GRIP team members, including CBO representatives, provided
feedback to the presenter about content organization, language,
and engagement. Cultural responsiveness was discussed to
ensure attendees would be able to connect and identify with the
material and that the material was communicated in a culturally
appropriate way, accounting for traditions and norms around
aging and health.To understand the educational gaps of older community
members, regular attendants of our partner CBO educational
programs at senior centers, religious institutions, public libraries
and CBO headquarters completed an informal needs assessment.
Older community members were asked to rank the followingtopics on their interest level, on a scale from 1 to 4 (1 being their
first choice and 4 their last) on four listed topics: nutrition, falls,
memory loss and cancer. Thirty-five older adults responded to
this survey and 71% indicated memory loss as most interesting to
them. From this, the GRIP team focused initial efforts to develop
the memory loss and dementia program. In the Fall 2015, the
primary presenter, a geriatrician, developed the audiovisual
module Memory Loss & Dementia, for the community older adult
population. The material incorporated imagery that the target
audience could relate to, such as Yoga, ethnic foods and landscapes
for sessions developed for the South Asian communities. The
geriatrician presented the material to the GRIP team. Using the
PEMAT, GRIP team members rated the material and the scores
for understandability and actionability were 59% and 78%
respectively. The material was revised based on the feedback,
improving these scores to 83% and 90%. Five of the 8 lectures
were interpreted, 4 to the predominant South Asian language
(Hindi or Bengali) and 1 to Spanish. The remaining 3 lectures
were delivered to English speaking audiences.
To identify the educational needs and the interests of
caregivers, the GRIP conducted a 90-minute focus group. The
subject of memory loss was identified as a topic of interest. A
module called Caregiver Education: Cognitive Impairment was
developed. Per GRIP’s content development process, it underwent
a PEMAT review (83% understandability and 80% actionability),
with the presenter adjusting after the feedback regarding
organization, language and cultural responsiveness. Since most
caregivers identified as South Asian, 4 of the 7 sessions were
provided in English with simultaneous interpretation to the
predominantly understood language of the group, Hindi. Though
the majority caregivers were native Gujarati speakers, the most
commonly understood language in the group was Hindi. The
remaining 3 sessions did not need interpretation or translation as
it was to English-speaking audiences.
Given the well-documented shortage of appropriately trained
HCPs in the care of the older adults, the subject of memory loss/
dementia/delirium, was well-suited for our HCP target population.
Four modules were created to meet the needs of each types
and level of HCP audience: Delirium in Older Hospital Patients
(Post Graduate Year -PGY- 1-3), Assessment and Management
of Cognitive Impairment in the Older Adult (Interprofessional),
Cognitive Impairment in the Older Adult (Nursing), and Dementia
& Delirium (PGY1). In this large educational initiative across three
learner groups, between November 2015 and January 2019, the
following sessions were implemented: Memory Loss & Dementia
(older community members) was conducted 8 times at 7 different
centers. Caregiver Education: Cognitive Impairment was offered
7 times at 3 different centers (one being a video live-stream
program) for caregivers. The 10 sessions for HCPs comprised one
of the four modules described and were conducted in 5 different
sites.
Measures
This study was conducted as a nested mixed-methods pre-post
intervention design to incorporate quantitative pre and post data
and qualitative data after the intervention to assess its effectiveness
(20). Questionnaires were developed to assess knowledge uptake
after participation. They contained five to six multiple choice
questions and were translated to multiple languages. They were
administered prior to and immediately after participation in the
educational program. Pre- and post-questionnaires were matched
using an identification case number. In August 2018, the pre-post
questions for community members were modified to increase
the difficulty of one question due to ceiling effect (question was
too easy on baseline). As seen in (Table 2), we are presenting the
aggregate results for the sessions prior to and after this change in
measure for the Memory Loss & Dementia sessions. Completion
of the questionnaires was voluntary and anonymous, and the
publication of these data was approved by the MSK Institutional
Review Board.
Analysis
Analyses were conducted using the statistical program
SPSS 21 (IBM Corp. Released 2017. IBM SPSS Statistics for
Windows, Version 25.0. Armonk, NY: IBM Corp). Demographic
characteristics, including age, gender, language preference and
birthplace, were analyzed using descriptive statistics (mean,
frequencies and standard deviations). Paired samples t-tests were
used to evaluate change in knowledge on the programs on preand
post-assessments. A p-value less than .05 was considered
statistically significant. Qualitative analyses were conducted
using thematic content analysis, the most frequent themes are
presented on (Table 3).
df: Degrees of Freedom
Sessions conducted before August 2018
Sessions conducted after August 2018: Questionnaire B includes increased difficulty in listed questions
Results
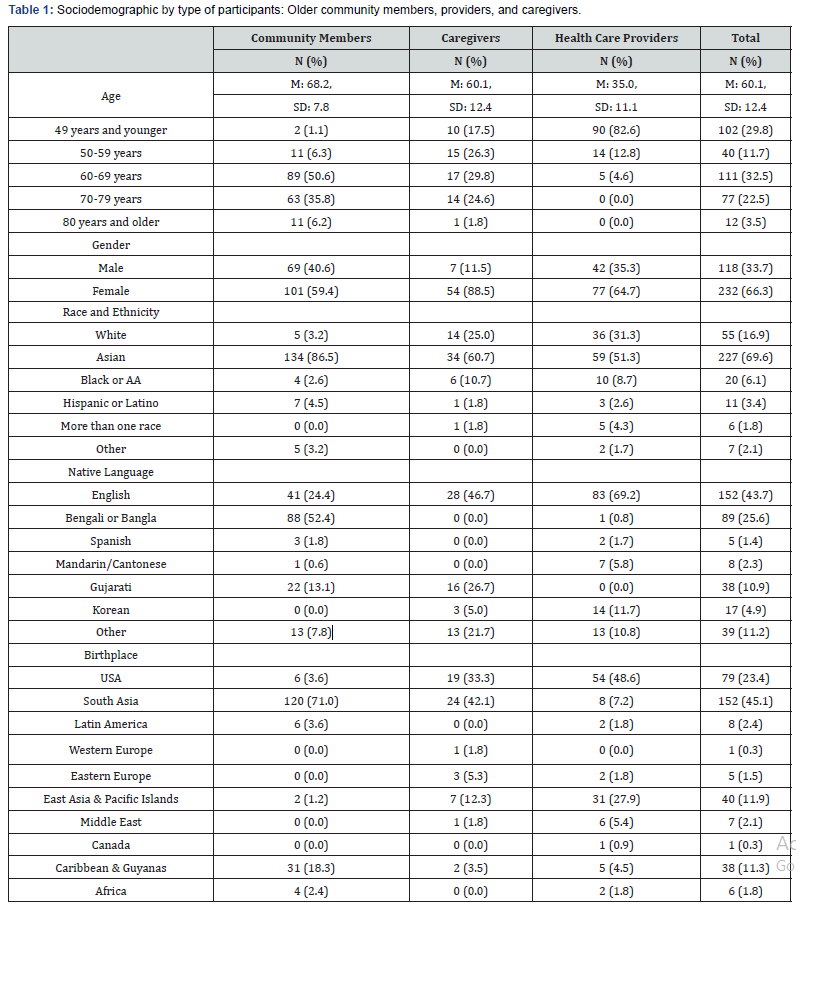
The total sample consisted of 378 participants:182 community
members, 63 caregivers, and 133 HCPs. Sociodemographic data
is presented in (Table 1). Of the older community members
who reported demographic information, the mean age was 68
(SD=7.8) and three out of five were female (59%). The majority
were Asian (87%), half reported their native language to be
Bengali (52%), and 71% were born in a South Asian country
(India, Pakistan, Bangladesh and Nepal). Caregivers had a mean
age of 60 (SD=12.4). The majority were females (89%) and almost
two thirds were Asian (61%). The primary language of 47% of
the caregivers was English, followed by Gujarati (27%). One third
were born in USA (33%) and 42% were born in South Asia.
Note: a Mean and Standard Deviations presented
instead of frequencies; b Other languages include: Arabic, Armenian,
Bahasa, French, German,
Guyanese, Hebrew, Hindi, Kannada, Korean, Nepali, Persian, Poshto,
Punjabi, Romanian, Russian, Tagalog, Tamil, Telugu, Turkish, Urdu,
Vietnamese;
c Other Countries by region include: 1) in South Asia, Bangladesh,
India, Pakistan, Nepal, 2) in Latin America, Brazil, Colombia, Puerto
Rico, Dominican Republic, Paraguay, El Salvador, 3) in Western Europe,
England, Germany, Ireland, 4) in Eastern Europe, Poland, Romania,
Russia,
Botswana, Greece, 5) in East Asia & Pacific Islands, China,
Philippines, Korea, Taiwan, Vietnam, 6) in Middle East, Israel, Syria,
Turkey, Bahrain,
Iran, Saudi Arabia, Lebanon, Iraq, Cyprus, in 7) Caribbean
(non-Hispanic) & Guyanas, Jamaica, Trinidad, Haiti, and 8) in
Africa, Cameroon.
Providers had a mean age of 35 years (SD=11.1), two thirds
were females (65%), almost half (51%) were Asian, the native
language of two thirds (69%) was English followed by Korean
(12%). Most of the providers were born in USA (49%), followed
by East Asian countries (28%). Almost half of the medical
professionals were residents (49%), followed by nurses (24%),
medical students (19%), physicians (5%), patient care technicians
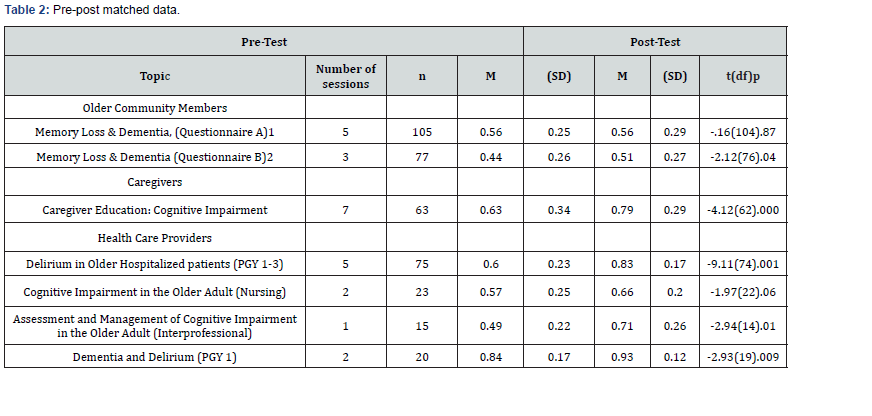
(2%), and social workers (2%). The t-tests for paired samples are presented in (Table 2). The
results indicate a statistically significant difference for the sessions,
Memory Loss & Dementia [t (76) = -2.12, p< .04], conducted with
older community members after the measure assessment was
updated in August 2018. The pre-post evaluations for the sessions
on Memory Loss & Dementia prior to upscaling of difficulty in the
measure conducted between April 2017 to May 2018 did not yield
significant results [t (104) = -0.16 p = .87]. The sessions conducted
with caregivers: Caregiver Education: Cognitive Impairment
showed highly significant increase in knowledge [t (62) = -4.12,
p < .001]. Among the HCP sessions Delirium in Older Hospitalized
Patients (PGY1-3) [t(74) = -9.11, p < .001]; Cognitive Impairment
in the Older Adult (Nursing) [t(14) = -2.94, p = .01]; and Dementia
and Delirium (PGY 1) [t(20) = -2.93, p = .009] showed improvement
in knowledge. There were no significant improvements in
knowledge for the Assessment and Management of Cognitive
Impairment in the Older Adult (Interprofessional) group. All
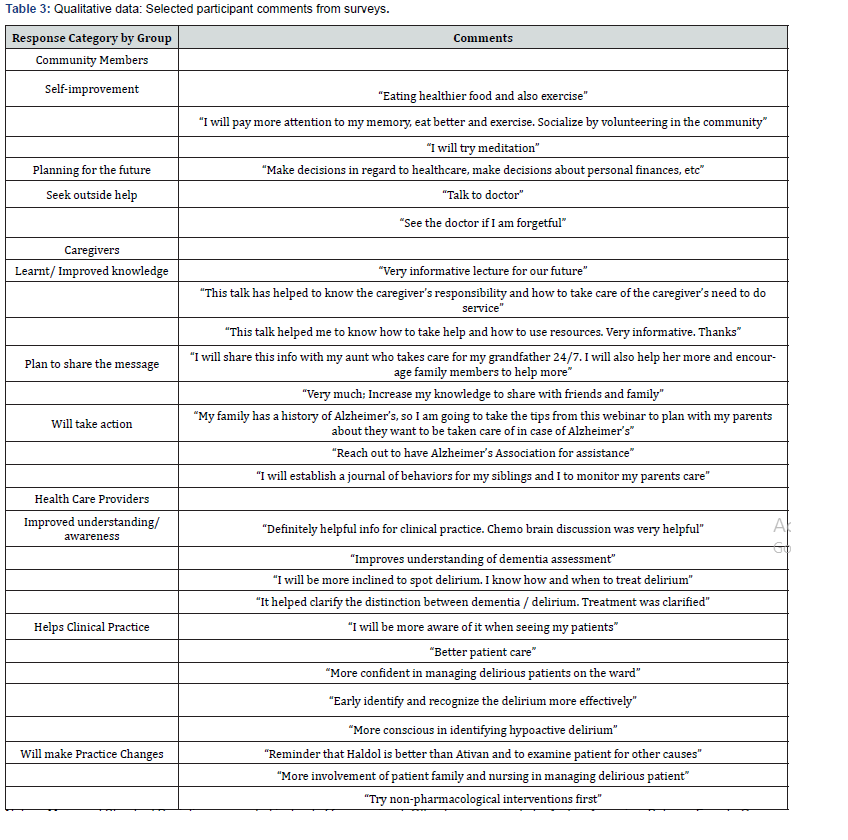
participants were given the opportunity to provide feedback after
completion of the sessions and asked how this information would
change their daily behavior or practice. These responses were
categorized into common broad themes which reflect improved
understanding and plans to make behavioral changes. Selected
themes and comments are presented in (Table 3). Overall, older
adults described specific behavior changes they would make, as
well as resources they would seek out to clarify doubts and obtain
care. Caregivers commented on knowledge gained as well as
future planning for those older family members who might need
dementia care. HCPs reported increased knowledge and detailed
clinical practice changes they planned to make in the care of older
adults with cognitive impairment.
Discussion
Our results demonstrate the successful development
and application of an educational program to improve the
understanding of cognitive syndromes in older minority
communities. We see consistent, significant improvements
in knowledge among older adults, caregivers and HCPs, and
qualitative data that describe improved understanding and
planned changes in behavior after the sessions. We identified
educational needs of older community dwelling ethnic minority
members and their caregivers to provide culturally responsive
educational sessions, in their language in a familiar and
comfortable environment. This specific educational and cultural
tailoring made sessions interactive and open for community
members and caregivers to approach it with a sense of familiarity.
There is a well described national shortage of geriatricians in
the US [21, 22]. Few medical residents choose the extra year of
training required to become a geriatrician, and those going into
other specialties typically get little exposure to the health needs
of older adults during their training. Internists, family medicine
doctors and other HCPs such as nurse practitioners and physician
assistants provide most care for older adults and they should be
trained [21-23] Educational programs like ours help to correct the
deficits in geriatric medicine knowledge in non-geriatrician HCPs.
This is one way of improving the quality of healthcare received by
older patients.
The implementation of this educational approach came
with its own set of challenges. Community health education in
underserved populations is complex: One major barrier we faced
was the wide range in literacy levels of the community member
participants. It ranged from a few people who were illiterate
and could not write their name in their primary language to
people with post-secondary and professional degrees. In many
cases, community organizers and members of the GRIP team
had to sit one-on-one with participants to fill the questionnaires.
Tailoring a pre-post questionnaire to assess knowledge change
in such an audience proved challenging Additionally, we had to
adjust educational materials to ensure understandability. Some
audiences wanted more detailed information and others didnot, so adjustments would often have to be made during the
presentation. These adjustments might have limited the ability to
accurately capture knowledge gain. After analyzing the difficulty
level of the questions based on initial sessions with a wide range
of audiences, we noted consistent high achievement on one item.
We modified that item to increase the difficulty of a question and
subsequent results showed statistical significance in knowledge
improvement. The community members’ qualitative comments
showed a positive impact. In the case of the HCPs, with higher
and more homogeneous educational attainment, the quantitative
analysis showed a significant improvement in knowledge uptake
and it paralleled the qualitative comments.
Another barrier we faced was adapting to the multiple
cultures and primary languages of the community and caregiver
participants. The sessions were interpreted to the most
understood predominant primary language of the audience and the
questionnaires and take-home resources were translated into the
same language. However, it is still probable that the sessions were
not fully understood by all members who attended because some
participants spoke different variations of the primary language or
a different primary language entirely. We conformed to cultural
practices by learning the cultural norms of the community prior to
conducting in each session. The sessions conducted at a mosque
for example had physical partitions between seating areas for
the male and female participants, and our own staff members
respected these boundaries and conformed to the dress codes and
interactions. Transportation and access to the community centers
by participants varied. Even in NYC, where public transportation
is available, it is a challenge for some older community members
and the attendance also depended on the weather. We tried
to schedule sessions according to the best times of day for the
caregiver groups and utilized existing protected meeting times for
HCPs to maintain attendance.
Future directions
We will need ongoing educational efforts and future studies to
assess the long-term benefits of these interventions in increasing
awareness and promoting a more proactive approach to care
from the community members and their caregivers. Patient
reported outcomes could be measured in community clinics after
educational interventions. Behavioral intention measures after
the sessions are also worth exploring. Caregiver related measures
such as stress, satisfaction with medical care, knowledge retention
and change in behavior should be evaluated long-term. Continued
retention of knowledge and the implementation of geriatric
principles by HCPs in their daily practices could also be studied.
Strategies to address challenges around health literacy and
surveys will continue to be addressed and cultural responsiveness
will continue to be integrated into the data collection procedures.
Conclusion
We have successfully developed and applied a critical
educational program about memory loss for older communitymembers, their caregivers and HCPs in diverse underserved areas
of NYC. The education was very well received and prompted the
attendees to propose behavior changes that could potentially
improve the care of individuals with cognitive disfunction. We
demonstrated significant short-term knowledge uptake on
memory loss and cognitive health among the three audiences.
The long-term effect of the knowledge gain and behavior change
needs to be better determined on future studies.
To Know more about Gerontology & Geriatric Medicine
Click here: https://juniperpublishers.com/oajggm/index.php
Click here: https://juniperpublishers.com/oajggm/index.php
To Know more about our Juniper Publishers
Click here: https://juniperpublishers.com/index.php




No comments:
Post a Comment