Pharmacology & Clinical Research - Juniper Publishers
Abstract
Background: A measles outbreak has been going on in France since 2017, where 2 779 cases were declared, of which 89% were not or poorly vaccinated. Facing the poor immunization among the cases, we carried out this study following the request from French General Direction of Health to “verify the immunization status and promote vaccination or catch-up if necessary”.
Objectives: Principal objective: To assess the vaccination coverage among the women workers in Orleans City Hall. i. Secondary objective: To compare the prevalence vaccination coverage with job activities.
Materials and method: A cross sectional study, based on medical files added to a questionnaire, in the preventive medicine service of Orleans city hall was performed.
i. Participants: including women born from 1980 to 1990 and working for the city at the time of the study. We compared our results by employment category (administrative, childhood and maintenance).
ii. Primary outcome: vaccination rate about women workers in Orleans City Hall
iii. Secondary outcome: prevalence rate and job vaccination coverage rate in Orleans City Hall.
Results: Among the 186 participants, the prevalence of measles vaccination coverage was 57.5% [50.4% - 64.6%] for two doses and 91.9% [88.0% - 95.9%] for one dose. Women working with children were generally less immunized (39.84% [31.52% - 48.17%] for two doses and 59.89% [51.05% 67.74%] for one dose). Moreover, women under 30 were more likely to be immunized (84.6% [74.8% - 94.4%] for two doses and 100% for a single injection).
Conclusion: Our results confirmed our hypothesis. Measles vaccination coverage in working women in the city hall of Orleans is poor compared to national recommendations.
Keywords: Vaccination coverage; Measles; Women’s health; Prevention health
Introduction
A vaccine catch-up is recommended, if measles vaccination of a young woman is not up to date. If they were born after 1980, they must have received a total of two doses of measles-mumps-rubella vaccine spaced a minimum of one month apart, whether or not they had one of these 3 diseases. If they were born before 1980 and have never been vaccinated, vaccination is recommended, especially if they have been exposed in their profession (health professions, early childhood professions). One injection is enough. If the young woman has received a vaccination, she must have effective contraception within 2 months after vaccination. Vaccinations in the workplace have two objectives: To protect employees against occupational risk by assuring them, by this act of prevention primary, individual protection; break the transmission chain and thus avoid, by immunizing them, that they do not contaminate their surroundings (colleagues, patients in the middle care, close). They are governed by: the Code of Public Health (art. L. 3111-4 a , L. 3112-1, R. 3112-1 and R. 3112-2) making certain vaccinations mandatory for some exposed professionals (or exposing the people they have been responsible for Law No. 2016-41 of 21 January 2016) to a risk of contamination; the Labor Code (article R. 4426-6) which provides that an employer, on proposal of the occupational doctor, can recommend a vaccination. For health professionals, is added the recommendation of ensure immunization also of the oldest, born before 1980, unvaccinated, with no history of measles or rubella (or the story is doubtful): a dose trivalent vaccine is recommended for training, hiring or in post, in priority in services hosting subjects at risk of severe measles. It is the same for professionals in contact with children [1].
Why we chosen in our study to follow adults from 28 to 38 years old? These young adults were born during a period of implementation of the vaccination recommendation against measles. The vaccine made its appearance on the calendar in 1983 precisely. But in the following years, the recommendation is followed very gradually. Thus in 1987, only 50% of children were vaccinated, barely 60% in 1988. Result: a wobbly group immunity, which allowed many people born in the 1980s to grow up without encountering the disease in their childhood because less circulation of the virus, while not being vaccinated, since the recommendation was relatively poorly followed. For the record, the highly contagious nature of measles requires about 95% vaccination coverage to prevent the circulation of the virus in the population (principle of group immunity). By contrast, before 1983, only 20% of children were vaccinated. The virus circulated so much, and almost all the children ended up catching it. “In the age groups over 40 years, we have more than 99% of people who are immunized, usually because they had measles as a child [2].
Highly contagious, a person infected by measles can infect 15 to 20 people in a non-immune population [3]. Late complications of measles are well known, such as sclerosing pan encephalitis (mortality rate: 0.5 to 1/1,000) [4]. In France, measles is considered to be harmless, sometimes among the healthcare professionals [5]. Since the vaccination campaigns of the 1980s, measles outbreaks have decreased with the increase in immunization coverage [6]. Consequently, the youngest generations are not familiar with this disease. Since November 2017, in France, a measles epidemic is spreading from Aquitaine to other regions including Centre-Val de Loire (2779 mandatorily reported cases, including 2702 cases in 2018, with a peak in April 2018). Among the cases of measles, 23% were hospitalized. Moreover, 89% of the cases were not or poorly vaccinated [7]. In the Centre-Val de Loire, cases have appeared since mid-January 2018. As of 25 May 2018, 90 cases had been reported in 4 months, indicating that the virus actively spread within the region [8]. To reduce the number of measles cases and their complications, Vaccination is an emergency. Thus, the objective is to reach 95% measles and rubella vaccination coverage (VC) in France [9]. No department achieved this goal until now. For example, in Centre-Val de Loire, in 2015, MMR vaccination coverage among 2-year old children was 76.2% IDC [nc] for two doses of the vaccine.
MMR vaccination has become mandatory for all children born since January 2018 [10]. Based on the High Council of Public Health recommendations, we carried out this study following the request from French General Direction of Health) to “verify the immunization status and promote vaccination or catch-up if necessary”. Following the French cross survey study conducted by Denise ANTONA and colleagues [2], the main objective of our study was to assess the vaccination coverage of women born from 1980 to 1990, working at the Orleans city hall and identify the factors associated with a correct VC. Our hypothesis was inadequate vaccination coverage for this population. The secondary objectives were the influence of job categories and age on vaccination status.
Objectives
i. Principal objective: To assess the vaccination coverage among the women workers in Orleans City Hall.
ii. Secondary objective: To compare the prevalence vaccination coverage with job activities
Materials & Methods
Study Design
A descriptive, cross sectional study based on medical records and a questionnaire were carried out.
Setting: This investigation took place at the Department of Preventive Medicine (SMP) of Orleans city hall.
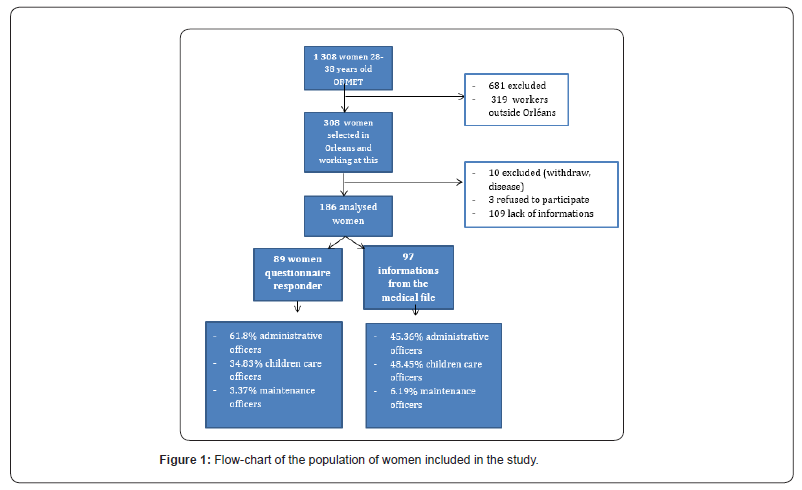
Eligibility criteria: The population was selected in the local medical monitoring software of the agents: Horizon (version n° 4.95.02A, date of conception 1995 in Nimes). Women born from 1980 to 1990 and working for the city of Orleans were included. We excluded agents no longer working at City Hall, women in long term Medical leave, and refusal to participate. The Department of Preventive Medicine (SMP) is in charge of 5 400 agents for the local authority. 1308 were women born from 1980 to 1990. For our investigation, we selected only the women working in Orleans, so we had 308 subjects. The survey involved 308 agents (Figure 1). 295 women answered to the questionnaire, 3 women refused to participate, 10 women were excluded endly 186 women were analyzed. At first, to inform the most people about our action, we carried out an initial communication strategy for the 5,400 agents of the metropolitan area. This strategy consisted of the dissemination of national documents about measles and measles epidemic. So, we would raise awareness about measles for all agents working for Orleans city hall.
Outcomes: From May to June 2018, all the information contained in the agent’s medical files was collected, aged, immunization status against measles, and profession. In July 2018, a questionnaire for the 308 agents was sent to the services. Including: demographic characteristics (age, employment) and measles vaccination status (dose number and date). Agents could return their responses by service mail or email. A phone call has been made for agents who did not have an e-mail address at the city hall. Three reminders by e-mail were sent on 21/08/2018, 04/09/2018 and 13/09/2018. The responses were collected from August to the end of September 2018.Women reporting two doses of vaccine were considered as complete vaccinated. Women who received a single dose or had childhood measles were considered partially vaccinated. Indeed, this choice had been made because one unique dose didn’t protect. For the secondary objectives, we classified women into three main job categories: administrative officers, childcare officers and maintenance officers. To see the influence of age, we grouped women into two groups, the under 30s and the over 30s. The age classes were chosen as the reference class of a German study [11].
Statistical Methods
Data sources: We estimated the necessary number of subjects. For an observational survey, the number of subjects to be included depends on the expected percentage of subjects for the desired trait (p), its difference from 100%, the desired precision, and the “alpha” risk of 5% of the first kind consented.
Statistical significance: It was considered when P was ≤0.05, Results are presented as means and medians, with 95% confidence intervals (95% CI) or Interquartile Ranges (IQR).
Study size: We estimated a necessary number of 280 subjects for an expected percentage of 76.2% (MMR CV rate among children observed in the region Centre-Val de Loire).
Measurement: The analyses were performed with Excel. Immunization coverage was calculated using as denominator: the sum of the information collected from medical records and the number of responses to the survey.
Quantitative and qualitative variables: The questionnaire was administrated by mail and e-mail and included the following socio-demographic variables: age, sex, socio-professional category and place of residence. Data on history of past measles infection and vaccination status were collected on recall. We did an exact Fisher test between the different use categories and immunization status. We did a chi2 independence test, grouping the age into two classes, under 30s and the over 30s.
Ethical review: The investigation was declared to the CNIL, in category MR-003, research in the field with consent. The declaration number, received on July 18, 2018, was the 2202567 v 0. The data from the questionnaires were anonymous for analysis. Express, free and informed consent was signed by the women during the inclusion.
Results
Participants
Among the study targeted population of 308 women, 186 women were included (60.4%) after exclusion of 10 long term leave and work quitting, 3 refusals to participate, and 109 without information in the medical records, and no response to the questionnaire (figure 1: Flow chart).
Descriptive data
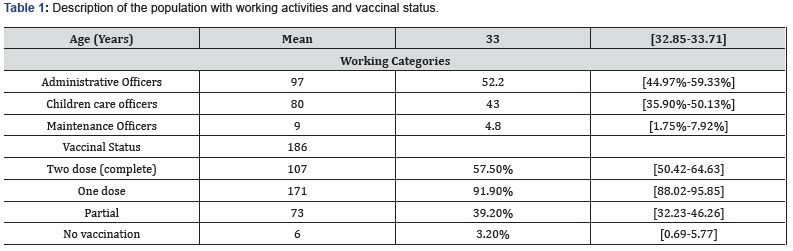
The 186 women were divided into three categories, 97 administrative officers, 80 officers working with children, and 9 maintenance officers. The average age was 33.3 years old [32.9 – 33.7].
Outcome data
The results were 107 complete vaccinated women, 64 partially vaccinated women and 9 who had measles during the childhood. 6 women were not vaccinated (4 administrative officers, 1 childcare officer, 1 maintenance officer).
Main results
The vaccination coverage rate was 57.5% [50.42%-64.63%] for women aged 28 to 38 years for 2 doses of the vaccine. The rate was 91.9% [88.02% - 95.85%] for one dose of the vaccine; this percentage included fully vaccinated women who have at least one dose, and those who received only one injection. Combining women with only one dose and those having had childhood measles, 39.2% [32.2% - 46. 36%] were partially vaccinated. Finally, only 3.2% [0.69% - 5.77%] of women were not vaccinated (Table 1).
Other Analyses
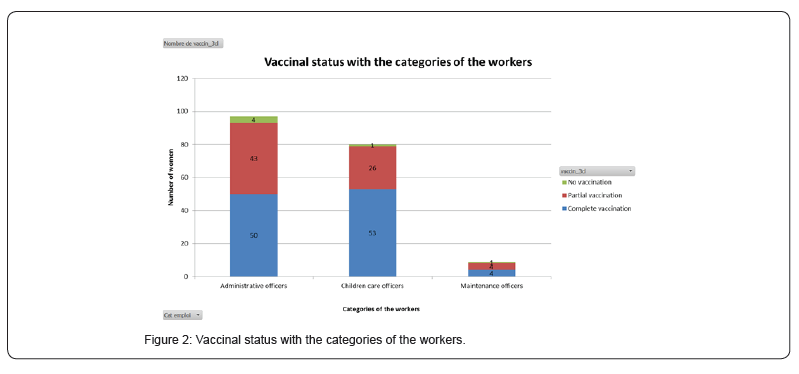
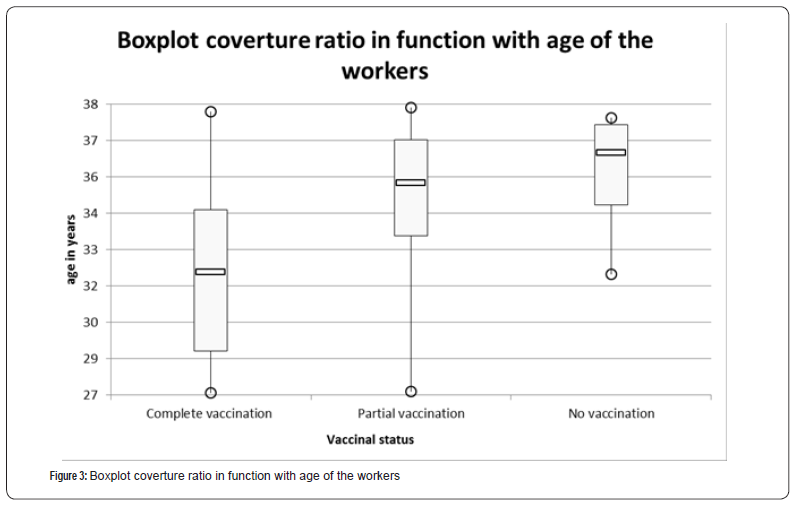
Vaccination against measles was not associated with the profession. We find 51.55% [41.60% - 61.49%] for two dose of vaccine and 86.60% [79.82% - 93.28%] for one dose among administrative officers, (39.84% [31.52% - 48.17%] for two doses and 59.89% [51.05% 67.74%] for one dose) in women working with children, as well as 44.44% [11.98% - 76.91%] for two doses and for one dose in maintenance officers, without any significant difference (p=0.955). Figure 2: Vaccination status by employment category. Taking into account the class-of-age, for the group aged 28 to 30-year old we found a complete immunization coverage of 84.6% [74.8% - 94.2%], and 100% for a single injection. For 31 to 38 years old, the VC is 47.0% [33.5% - 60.6%] for two doses of vaccine and 88.8% [80.2% - 97.4%] for a single dose. With a significant difference according to the age class, women aged 28- 30 years are significantly better covered than those aged 30-38 years (p<0.001) (figure 3: Vaccination coverage by age). There is a significant difference between these two classes (p=3.22.10-6).
Discussion
Between 2000 and 2016, it was estimated that measles immunization prevented 20.4 million deaths, making it the best public health investment. The number of deaths globally decreased by 84%, from 550,100 in 2001 to 89,780 in 2016 [12].
Key Results
Our study estimated vaccination coverage for MMR at 57.5% [50.42% - 64.63%] for two doses for women aged 28 to 38 working in the Orléans metropolitan territorial community. However, the vaccination rate among children in the Centre-Val de Loire is 76% for two doses. Another study conducted in Poitou- Charente [13] shows a CV at 93% for one dose and 76% for two doses in 17 years old adolescents. These results, for children and adolescents, suggest that there has been an increase in vaccination for these new generations. With the obligation since January 2018, it is hoped that immunization coverage will increase. It is important to focus on immunization coverage for both injections. Indeed, the measles vaccination scheme includes two injections. The second dose does not constitute a reminder. This is a catch up for people who have not seroconverted for one or more antigens. Indeed, this decision was taken in view of the vaccine insufficiency and the effectiveness of the vaccine (90-95%) in order to eliminate the risk of having measles. The Vaxisoin study [14] shows that caregivers have insufficient vaccination coverage for recommended vaccines, including vaccination against measles and especially for its the second injection. The vaccination coverage rate for all occupations combined in 49.7% [30.8% - 68.8%]. Our CV rate is close to these results. Yet, the women answering our questionnaire are generally vaccinated women. Non-responders may be unvaccinated. These women may have hesitations about vaccination, or fear of having to be vaccinated. Thus, there is a response bias in our survey. 57% of vaccination coverage is not only a weak result, but it could be overestimated by this way.
Concerning the population of the study, one argument justifying the choice of age, is the importance of injecting the second dose of the vaccine for all persons born since 1980. We based ourselves on the opinion of the High Council of Public Health (HCSP), concerning the MMR, which states that there are no recommendations for people born before 1980. A seroprevalence study shows that these people are much less receptive to the vaccine. In addition, it is assumed that the majority of this population had measles in childhood. A crosssurvey study about measle seroprevalence was conducted on blood donors in France. It showed that the proportion of people 18-32 years old susceptible to measles infections remained high in France in 2013. The rate was estimated 9.2%, in metropolitan France, even after the promotion campaigns about vaccination catch-up during and following the major measles epidemic in 2009-2011 [2]. Moreover, we have taken an interest in women because we know that many works with young children (ATSEM, maintenance officers, childcare assistants, etc.,) and can also be in touch with children in their family life. We may think that some of them show a strong resistance against vaccinations. Indeed, while it is difficult to quantify the number of people hesitant or resistant to vaccinations, the experts acknowledge an increase of these resistances. Vaccination may be perceived as dangerous or unnecessary [15]. Some physicians themselves may have hesitations [16]. The vaccination campaign against influenza / H1N1 has probably had deleterious effects on confidence in vaccines. In the years following this pandemic influenza 2009- 2020, there was a significant decrease in vaccination coverage, suggesting this loss of confidence due to the controversies raised by the vaccination campaign [17-19].
Strengths and Limitations
Our population selection method did not use a random sampling technique. We made a selection of “comfort”, filtered on the city of Orléans for feasibility reasons. In fact, metropolis has been constituted recently. We did not have access to the medical records of the 1308 targeted women, but only to 308 in Orleans. The data were obtained from occupational medicine. The analysis by socio-occupational category, in particular for professions subject to a vaccination obligation, is an innovation approach compared to other methods of measuring immunization coverage [20]. More staff in administrative jobs are not vaccinated, although the difference is not significant, we can hypothesize that they feel less concerned about this vaccination than their colleagues working with children.
Interpretations
Finally, we show that the youngest women aged 28 to 30 are significantly better vaccinated than those aged 31 and over. This result makes it possible to better target priority populations for vaccination catch-up.
Conclusion
This study, the first to be carried out in local authorities at the Orléans City hall, provides very information on the MMR’s vaccination coverage. The MMR coverage rate found in women aged 28 to 38 is well below the 95% required to eradicate the disease. In addition, to providing epidemiological results, this study also aimed to promote vaccination. We believe we have informed many of the city’s agents. We were able to inform women in the study who were only partially vaccinated, to redirect them to appropriate management. In the context of occupational health, this survey could be extended to other vaccines, mandatory or recommended for certain professions.
To Know more about Pharmacology & Clinical Research
Click here: https://juniperpublishers.com/index.php




No comments:
Post a Comment