Cell Science & Molecular Biology - Juniper Publishers
Abstract
Cytosine arabinoside syndrome is a rare clinical complication of cytosar administration characterized by a constellation of symptoms of fever, myalgia, arthalgia, conjuctival suffusion, non-pruritic maculopapular rash, respiratory distress and non-cardiogenic pulmonary oedema. The clinical manifestation of the syndrome ranges in severity from being mild to fatal. We described a 68-year old man with acute myelogenous leukaemia who developed cytarabine syndrome during subcutaneous cytosar administration. The pathogenesis of this syndrome is still not well understood but it is believed to be an immune mediated cytokine response to cytarabine apoptotic effect on the blasts. Although there is no definite treatment, corticosteroid use has proven efficacious as a prophylactic and treatment agent because of its anti-inflammatory properties. Haematologist should therefore look out for this adverse event in patients with Acute leukaemia who are being treated with Cytosine arabinoside.
Keywords: Cytarabine syndrome; Acute myelogenous leukaemia; Corticosteroids
Introduction
Cytosine arabinoside (Ara-C) is an important component of induction chemotherapy in combination with other agents for acute myeloid leukaemia and other haematological malignancies [1]. Ara-C belongs to the antimetabolites group of cytotoxic drug whose mechanism of action is to block metabolic pathways used in DNA synthesis. Ara-C is an analogue of 2’-deoxycytidine (a pyrimidine), a form it is metabolized to in vivo and incorporated into developing DNA where it acts to inhibit DNA polymerase and blocks replication. It is given at a standard daily dose ranging from low (20mg/m2), standard (100-200mg/m2) and high (3g/m2) through intravenous or subcutaneous routes [2].The commonest side effects of Ara-C are nausea, vomiting, diarrhoea, loss of appetite and fever. In addition, a rare and distinct clinical constellation of fever, arthralgia, myalgia, bone pain, occasional chest pain, maculo -papular rash, conjunctivitis and malaise called Cytarabine syndrome was first described by Castleberry in 1981 and later by other investigators [3,4]. It usually occurs within 12 hours following cytarabine administration [3,5]. A literature search of report of cytarabine syndrome in Africa did not yield any results and hence we concluded that physicians in Africa may be less aware of this complication of Ara-C. This report is therefore aimed at increasing physicians’ awareness to this rare complication of commonly used Ara-C.
Case Report
A 68-year old male who first presented to the Haematology Day Care Unit (HDCU) with a referral letter from another Tertiary health Centre in the country on request of the patient for a second opinion having been previously diagnosed of acute myeloid leukaemia. He had earlier presented to the referral centre with high grade fever and abnormal complete blood count (CBC) ordered by his family physician. He had been on treatment for systemic hypertension, type II DM and benign prostatic hyperplasia. Examination findings at presentation were significant for moderate pallor, shotty left cervical lymph node enlargement and bilateral non-tender pitting pedal oedema. A repeat CBC at our facility shows leucocytosis, severe anaemia and thrombocytopaenia (white blood cell (WBC) 54.5 X 109 Cells/L haemoglobin 7.3g/dl, and platelets 5.0 X 109 Cells/L). Peripheral blood smear review showed leukocytosis with 90% monoblasts and bone marrow revealed a severe hypercellular marrow with maturation arrest and 75% of the nucleated cellular marrow elements being monoblasts.
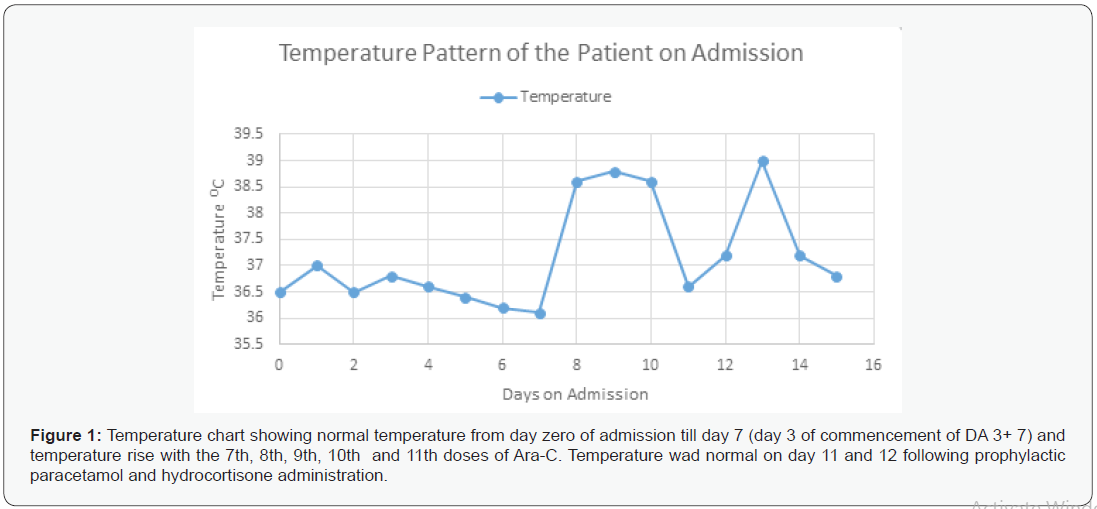
The patient was thus diagnosed of AML-M5a and commenced on supportive treatment with packed cells and platelets transfusions. He was later commenced on DA 3+7 chemotherapy with intravenous (IV) Daunurobucin 50mg/m 2 on days 1, 3, 5 and subcutaneous Ara-C 100mg/m2/day in 2 divided doses for 7 days. Ondasetron and Allopurinol were added as per protocol. On review on day 4 of commencement of Ara-C, he reported fever (temperature 380C), tachypnoea and tachycardia, palpitation, shortness of breath, myalgia, chills and rigor a few minutes after the 7th dose of Ara-C. These symptoms all resolved following administration of iv paracetamol 1g stat and hydrocortisone 100mg start. He also had 2 similar experiences following 8th and 9th doses of Ara-C and at this time there was associated respiratory distress with SpO2 ranging between 90- 93%. These symptoms resolved following oxygen therapy, iv paracetamol 1g stat and hydrocortisone 100mg. A probable diagnosis of Cytarabine syndrome was made and subsequently premedication with iv paracetamol and hydrocortisone were instituted for every other doses of Ara-C with significant improvement in symptoms. On the 6th day following the administration of 11th dose of Ara-C, high grade fever, rigors, myalgia and respiratory distress re-occurred despite premedication and therefore subsequent doses of Ara-C were withheld and fever subsequently resolved. However, in the third week of admission he developed high grade fever (temp up to 39.50c) and lethargy. Blood and urine samples were taken and sent for microbiological culture and sensitivity and he was commenced on empirical iv ceftriaxone and metronidazole, as well as prophylactic oral fluconazole and acyclovir. Blood culture yielded Klebsiella pneumonea while urine culture was sterile. He died 7days post DA 3+7 chemotherapy of features suggestive of septic shock before culture reports were returned. Figure I below shows the temperature pattern of the patients during the chemotherapy.
Discussion
Our patient developed a new onset of fever about four days (80hours) after initiation of standard dose of Ara-c which is within the reported range of timeline of 9-90 hours of onset of Ara-c fever [6]. Fever is the commonest presentation of Ara-C syndrome in combination with other symptoms [6]. Ara-c fever has been defined as a single axillary temperature of 38.30 c (1040F)………….38.00C (1010 F) and above or a temperature of 38.00 c (1010 F) for ≥ 1hour in a patient with absolute neutrophil count above 500 x 109 cells/L and without an apparent source of fever except Ara-c [7].The neutrophil count of our patient at this time was 750 x 109 cells /L and the patient has no identifiable focus of infection although he was on prophylactic antibiotics and had been empirically treated for malarial because of the possibility of transfusion associated malarial. In addition to fever, this patient also had arthalgia, myalgia and a non-pruritic rash but no conjunctivitis. The association of fever with the above symptoms provided a strong evidence for the diagnosis of Ara-C syndrome. The finding of fever which is the only constant symptom in addition to any of the other symptoms described earlier established the diagnosis [3,6,8]. Furthermore, the fact that these symptoms were abated by administration of paracetamol and hydrocortisone, the efficacy of which has been documented [9,10] laid more credence to our diagnosis. The exact pathogenesis of Cytarabine syndrome is not fully understood. The manifestations of Cytarabine syndrome were initially attributed to hypersensitivity or vasculitis [11]. However, recent evidence supports an immune-mediated response following cytarabine induced apoptosis that results in a rapid increase in proinflammatory cytokines as the critical initiating factor [12,13]. Activation of NFkB, by many pathways in response to Ara-C is central to the production of pro-inflammtory cytokines; tumour necrosis factor-alpha (TNFα), interleukin-6 (IL-6), and interferon gamma (IFNγ) which mediates this syndrome [12].
The successes attributable to use of corticosteroids in preventing and treating this syndrome is predicated on its ability to suppress NFkB [10,14]. Our patient also had pulmonary involvement as evidenced by a low spo2 90-93% despite oxygen therapy. Pulmonary adverse effects have been reported to occur in 20-40% of patients exposed to Ara-C12 which may present as mild difficulty with breathing, nonproductive cough, pleural effusion, to severe and fatal respiratory distress syndrome and non-cardiogenic pulmonary oedema [15- 17]. We therefore inferred that the low oxygen saturation in this patient was related to cytarabine although the patient was unable to do a chest x-ray to confirm the pattern of lung affectation due to on non-availability of a functional mobile x-ray machine in our facility at that moment. The clinical severity in our patient can be described as moderate because of the reversible lung involvement.
The clinical severity of Cytarabine syndrome is dependent on a number of factors including the dose of Ara-C and the tumour burden. [3,4,9,10,18] Matthew et al [12] reported persistent respiratory symptoms in a 41-year old with AML despite steroid prophylaxis and concluded that the poor response in that patient was due to high tumour burden. This finding is similar to that of the index patient who continued to have fever and hypoxaemia despite steroid necessitating discontinuation of Ara-C treatment on day 6 of a 7-day cycle. The recommended treatment protocol for Cytarabine syndrome is per oral (PO)steroid prophylaxis with Prednisolone 10mg daily which may be increased to 10mg tds or changed to PO Dexamethasone 8 mg daily, this may also be increased to twice daily. [12] Hall et al suggested intravenous methylprednisolone, 1mg/kg every 6hours, diphenhydramine, 1mg/kg every 6 hours, and ranitidine, 1mg/kg every 12 hours, given for 2 days before the administration, continued throughout the 5-day treatment course and for 1 day after completion of highdose cytarabine [9].
Conclusion
This case report highlights the clinical presentation, diagnosis and treatment of cytarabine syndrome in patients with AML. It is important to recognize this syndrome which may be common but missed in patients receiving Cytarabine therapy so that appropriate therapy may be instituted to prevent potential fatal complications which may arose from misdiagnosis.
To Know more about Cell Science & Molecular Biology
Click here: https://juniperpublishers.com/index.php




This blog is very helpful and informative for this particular topic. I appreciate your effort that has been taken to write this blog for us. top ent specialist in hyderabad
ReplyDelete