Orthopedics and Rheumatology - Juniper Publishers
Abstract
Objectives: Scaphoidectomy and four-corner arthrodesis (FCA) using a circular plate is becoming a common surgical option as a salvage procedure for Scaphoid Nonunion Advanced Collapse (SNAC). In this article we report our experience at Royal Medical Services with Scaphoidectomy and four corners arthrodesis using a circular plate fixation and autogenous bone grafting showing our surgical technique, outcome and complications.
Methods: A retrospective review of all patients who underwent FCA with circular plate fixation between February 2014 to February 2019 at Royal Medical Services. Patients were called and asked to come back to our clinic for clinical and radiological evaluation. 26 patients with a mean age of 34 years (range, 24-56 years) at the time of surgery were evaluated for range of motion (ROM) using goniometer, for grip strength using a dynamometer and for carpal fusion based on the most recent postoperative wrist x ray.
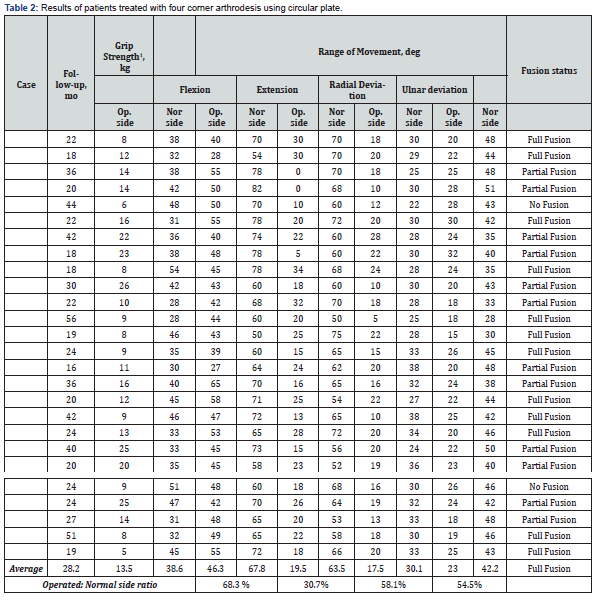
Results: 26 procedures (26 patients) were clinically and radiologically evaluated. Range of motion averaged 52.9% compared to the contralateral wrist (average flexion 68.3°; average extension 30.7°; average radial deviation, 58.1°; average ulnar deviation, 54.5°). Grip strength averaged 34.9% of the opposite side. Radiological evaluation showed that 12 cases progressed to Full fusion (46.1 %), partial but solid fusion was present in 12 cases (46.1 %), while non-union was present in two cases (7.6 %). Three patients (11.5%) underwent additional operations (two for hardware removal and one for tendon exploration).
Conclusion: We found that FCA with circular plate yielded reasonable results, ensures fusion, and is a good alternative to traditional implants like K-wires, Herbert screws, or staples.
Type of study/level of evidence: Therapeutic IV.
Keywords: SNAC wrist; Four-corner arthrodesis; Circular plate
Introduction
Scaphoidectomy and four-corner arthrodesis (FCA) is a salvage procedure used for treatment of scaphoid nonunion advanced collapse (SNAC). This procedure was first described by Watson and Ballet in the 1980s and demonstrated reliable pain relief while preserving a functional wrist range of motion and grip strength [1-4]. Fixation methods for this procedure include K-wires, staples, headless compression screws and recently, circular plates (DCPs) were developed and introduced in 1999 [5]. Circular plate would provide pain relief, improved function, and a higher union rate compared to existing data of other Fixation methods [5,6]. At our institution, Scaphoidectomy and four-corner arthrodesis (FCA) has been routinely performed using different fixation methods since 2008. However, the circular plate was predominantly used since 2014. The purpose of this study is to analyze the outcome of using circular plate as a method of fixation in this procedure, specifically regarding residual range of motion (ROM) and grip strength as well as to assess fusion rate in this patient group.
Materials and Methods
Patient selection
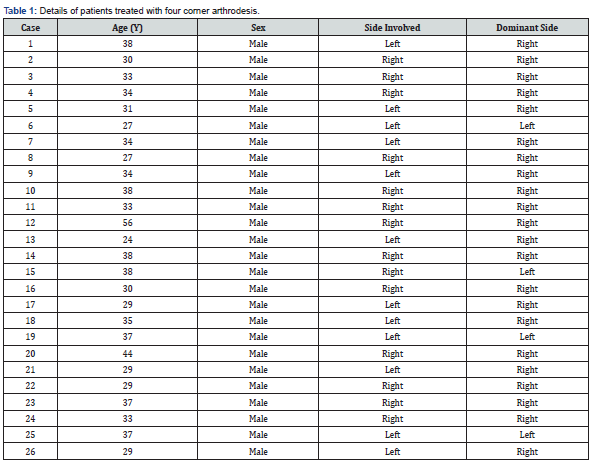
A retrospective review was performed for all patients who underwent Scaphoidectomy and four corner arthrodesis using circular plate between February 2014 to February 2019 in Royal Medical Services by three different hand and upper limb surgeons. Patients were Included in the study if they were treated using a circular plate for SNAC wrist. Patients were excluded from the study if they underwent arthrodesis using any other implant. A total of 26 surgeries on 26 patients were identified that met the study criteria and were considered for inclusion. Surgical indication was SNAC wrist in all patients. The mean age of patients was 34 years. All were men and the Right wrist was involved in 14 patients while Left wrist was involved in 12 patients. 16 injuries were dominant side. The minimum follow-up was 18 months (mean, 28.2 months; range, 18-56 months). The demographic data are listed in Table 1.
Radiological Assessment
Radiological evaluation of carpal fusion status was based on the most recent postoperative poster anterior (PA) and lateral wrist x rays (Figure 1). fusion status was determined by a fellowship-trained hand and upper limb surgeon at our department. Full fusion was determined by the presence of bony consolidation across the intercarpal joints and absence of visible joint lines between all the four bones (lunate, capitate, hamate and triquetrum); whereas partial but solid fusion was defined as the union of the lunate and capitate. These definitions were used because successful clinical results depend on fusion of lunate and capitate, whereas incorporation of either hamate or triquetrum, in and of themselves, are not required for long-term stability of the carpus [2,7-9]. Non-union is defined as persistent visible joint lines between lunate and capitate. Postoperative x rays were also analyzed for any evidence of metallic failure or dorsal impingement. Range of Motion (ROM) and Grip Strength Final ROM measurements were obtained for all patients using goniometer. ROM 52.9% of the opposite side (average flexion, 68.3°; average extension, 30.7°; average radial deviation, 58.1°; average ulnar deviation, 54.5°). The grip strength was also obtained for all patients using dynamometer. The average grip strength was 13.5 kg which was an average of 34.9 % of the opposite side.
Surgical Technique
We performed the surgery through a dorsal midline skin incision in line with the third metacarpal bone. Sharp soft tissue dissection was carried down to the wrist extensor retinaculum. The third compartment with the extensor policies longus (EPL) was released and transposed. The fourth compartment opened, and its tendons were retracted to the ulnar side, in addition to posterior interosseus nerve neurectomy. The capsule was opened with a radially based flap. Next, the whole scaphoid was excised, and a high-quality cancellous bone graft was harvested from distal radius and scaphoid bone (Figures 2 & 3).
A fine bone nibbler was used to denude all articulations down to bleeding cancellous bone of the capitate, lunate, triquetrum and hamate. The four corners of the bones were fixed provisionally with K-wires. The circular plate rasp was centered on the four-corner area, and reaming was started until the rasp was seated below the dorsal tip of the lunate. Any debris were removed with small curette. The bone graft was packed between the bones. An appropriate-size circular plate was placed such that two screws could be placed into each of the 4 bones when possible. A 1.5-mm drill bit was used, followed by either 2.4-mm screws or 2.8-mm screws depending on quality of bones. Screws were tightened progressively in a radial order, to maximum compression. Intraoperative x-ray was used to confirm carpal bones alignment, circular plate position and screws length. More care was required for the triquetral screws, to make sure they do not penetrate the piso-triquetral joint. The center of the circular plate and the surrounding area were filled-up with bone graft. The capsule, retinaculum, and the skin were closed, respectively. The wrist was immobilized for 6 weeks postoperatively.
Results
The mean follow-up period was 28.2 months (range 18-56 months) Table 2. Full fusion was achieved in 12 patients at a mean time of 26 months (range 19-56 months) postoperatively. Another 12 patients (46.1%) had a persistent visible line in triquetral-hamate joint; however, the fusion mass was stable (partial but solid fusion). Two cases (7.6 %) ended with non-union. Two patients (7.6%) had dorsal pate impingement that necessitated plate removal. Another patient (3.8%) had weak ring finger extension and underwent surgery for tendon exploration and repair. There were no postoperative infections. Wrist flexion averaged 46.3° (range, 27°–65°), extension averaged 19.5° (range, 0°–34°), average radial deviation, 17.5° (range 5°–28°); average ulnar deviation 23° (range, 15°–32°). ROM of the surgically treated wrist was 52.8% that of the opposite normal wrist. Maximum grip strength of the surgically treated wrist averaged 13.5 kg which is 34.9% that of the opposite normal wrist (range, 11%–61.9%)
Discussion
Despite the effective diagnostic and treatment options available today for detecting and treating scaphoid fractures, we continue to see a high number of scaphoid nonunion. Left untreated, scaphoid nonunion can progress to carpal arthrosis and scaphoid nonunion advanced collapse (SNAC). The distal part of the scaphoid will rotate into flexion while the lunate will assume an extended posture. Over time, this will progress into dorsal intercalated segment instability (DISI) and pancarpal arthrosis [2,10]. However, the radiolunate joint has consistently spared in SNAC pathway, even when there is severe DISI stance of the lunate. This preservation of the radiolunate joint is the basis of the 4-corner arthrodesis [5,7,8].
Treatment of SNAC wrist has always been challenging. Different kinds of treatments, such as proximal row carpectomy, partial wrist arthrodesis, and total wrist arthrodesis have all been described with varying rates of success and complications [4,8,11-13]. Four corners arthrodesis together with bone grafting is a proven technique in the treatment of SNAC wrist with intact radiolunate articulation favored by many surgeons despite the variable tools used for fixation such as screws, k-wires, staples and more recently, the circular plates [5,6,9]. The circular plate combines the benefits of rigid internal fixation and hence early active ROM exercises with the ability to compress the four carpal bones together [7,14]. It is this feature that essentially makes it a potentially useful tool in the treatment of SNAC wrist.
We hypothesized that the circular plate would be an effective method for treatment of SNAC wrist. Twenty-four patients (92.3%) in our series achieved full or partial solid fusion and reported a reasonable wrist range of motion as well as grip strength. Our study is limited by the lack of statistical analysis due to relatively low number of patients. Moreover, it is a small retrospective case series. Nonunion rates with conventional methods like K-wires, screws, or staples for fixation varies in literature between 0% and 18% [1,8,12,15,16]. In other hand, nonunion rates with circular plates were reported between 0% and 63% [5,12,17], Bedford and Yang [6] and Merrell et al. [2] reported zero nonunion rate. The explanation for the varied results may be attributed to different tools that have been used, differences in quantity and quality of bone graft and exacting technique [6,9-11]. In our series we reported two cases of non-union (7.6%). we attribute this to proper quantity and quality of bone graft, proper reaming and denuding of all cartilage surfaces, and rigid internal fixation afforded by circular plate. In two larger series of comparison studies, Ashmead et al. [6], and Watson et al. [13] reported 53 % ROM of the opposite side. Our results fall near this range at 52.8% ROM of the opposite side. Our result of 34.9% grip strength of the opposite side lags behind those reported in the literature. Watson et al. [13] reported 80% grip strength of the opposite side and Krakauer et al. [9] reported 78.5% grip strength of the opposite side.
Conclusion
In our hands, use of circular plate for scaphoidectomy and four-corner arthrodesis was associated with good clinical and radiological outcomes. We believe that circular plate is a useful tool and is a good alternative to traditional implants like K-wires, Herbert screws, or staples.
To Know more about Orthopedics and Rheumatology
Click here: https://juniperpublishers.com/index.php




No comments:
Post a Comment