Open Access Journal of Surgery - Juniper Publishers
Abstract
Background: An increasing number of general
surgical patients are being prescribed antiplatelet and anticoagulant
medications (APAC) for various cardiovascular conditions. We aimed to
characterise APAC usage in emergency general surgical patients admitted
to a rural hospital and assess the impact of APAC usage on patients.
Results: 118 patients were classified into two groups: non-APAC (n=96, 81%) and APAC (n=22, 19%). The majority (91%) were antiplatelet medications. Patients older than 60 years were more likely to be on APAC (p<0.0001). Patients admitted with bleeding pathology were more likely to be on APAC (p<0.05). 15% of all emergency operations were on APAC. There was no difference in the use of central venous or arterial line for increased monitoring (p=0.14) or in the use of warming blanket (p=0.94). APAC patients were more likely to receive transfusion during admission (p=0.04). The recorded morbidities (n=2) and mortality (n=1) cases in this study were all in the APAC group.
Conclusion: The use of APAC is more prevalent in those aged 60 years and above. 91% of APAC are antiplatelet medications. Patients on APAC are more likely to be admitted for bleeding issues, receiving transfusion, and an increased risk of morbidity and mortality. There is an urgent need for well-established, recognised and more accessible clinical guidelines regarding the emergency APAC management, especially for antiplatelet medications, in rural emergency general surgical patients.
Keywords: Antiplatelet; Anticoagulant; Rural general surgery; Emergency general surgery; Morbidity; Mortality
Abbreviations: APAC: Antiplatelet and Anticoagulant medications
Introduction
Antiplatelet and anticoagulant medications (APAC) are being widely used in the prevention and treatment of various cardiovascular and thromboembolic diseases. With their ever-expanding indications in an aging Australian population, the management of APAC in elective and emergency surgical patients is becoming increasingly challenging, and the advent of novel oral anticoagulants is adding more complexity to this challenge. Patients on APAC present a clinical challenge for treating surgeons, physicians, anaesthetists and haematologists as there needs to be a careful balance between the bleeding and thromboembolic risks associated with cessation of these medications. Surgeons need to decide on the timing and type of operation performed, along with the judicious use of limited, often precious blood products and haemostatic agents.
Previously established guideline on perioperative management of APAC was mostly on the perioperative management and emergency reversal of warfarin [1]. However, the more recent guideline now includes the perioperative management of other APAC including the novel oral anticoagulants [2]. Although the guidelines are helpful, the APAC management in some patients still depends on the clinician’s judgement and individual patient’s clinical situation. The aim of our study was to characterise the prevalence of APAC medications in rural emergency general surgical patients, and to assess the impact that these APAC have on the clinical management of these patients and associated morbidity and mortality.
Materials and Methods
A prospective study of all general surgical admissions through the Emergency Department of Northeast Health Wangaratta (Victoria, Australia) from July to October 2014 was conducted. During these four months, a datasheet for each patient was completed by a member of the surgical team at the time of admission and during inpatient stay. Data collected included patient demographics (gender, age, length of stay, admission diagnosis), APAC usage (type, indication, duration of cessation), admission diagnosis, length of stay, types of operation, anaesthesia techniques, morbidity and mortality. Data was then statistically analysed using ANOVA (t-test) method (Microsoft Statistical Package). The ethics approval was obtained from the hospital ethics committee.
Results
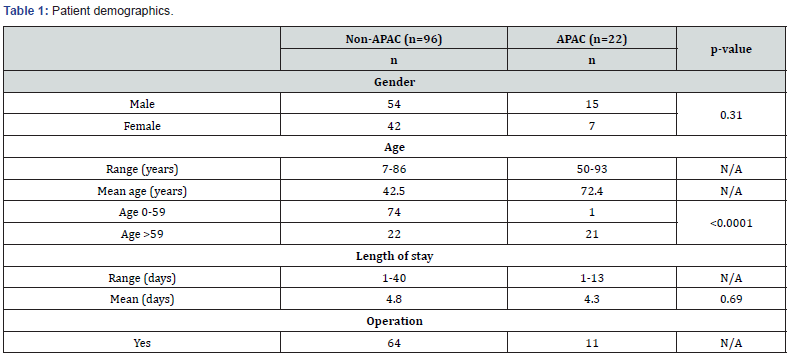
Patient demographics (Table 1)
A total of 118 consecutive general surgical patients were admitted through the Emergency Department. The patients were classified into two groups: non-APAC (n=96, 81%) and APAC (n=22, 19%). There was no difference of APAC usage based on gender (p=0.31). Patients in the APAC group were older compared to the non-APAC patients (mean age 72 vs 43 years old). Amongst patients younger than 60 years old, only one patient (1%) was on APAC. This contrasted with those aged 60 and above, in which 49% were on APAC (p<0.0001). The age groups were analysed in this way as there appeared to be a distinct increase in APAC usage from the age of 60 years old. The length of stay was not affected by APAC usage (non-APAC mean 4.8 days vs APAC mean 4.3 days) (p=0.69). 15% of all operated patients were on APAC medications.
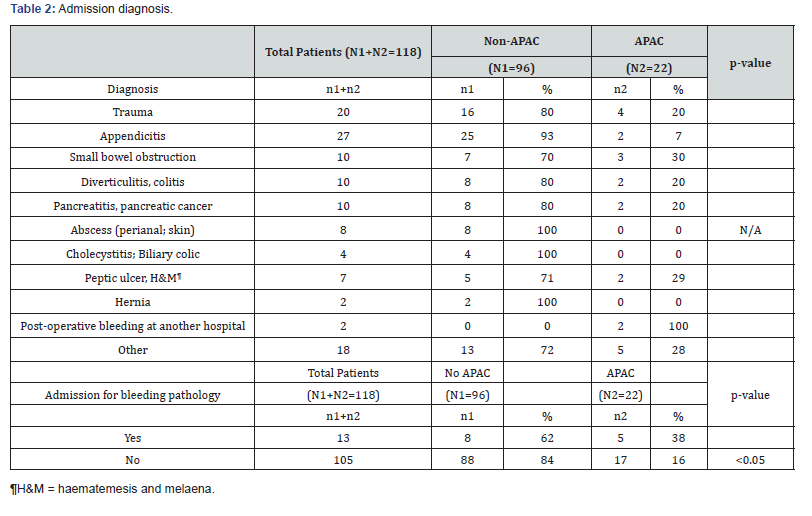
Admission diagnosis (Table 2)
There were 13 patients (out of 118) who were admitted for bleeding problems such as upper and lower gastrointestinal bleed, as well as bleeding complications following surgery at another hospital. In this group, the patients were more likely to be on APAC (p<0.05) with five patients (38%) being on APAC. Also, 20% (4 out of 20 patients) of all trauma patients were on APAC.
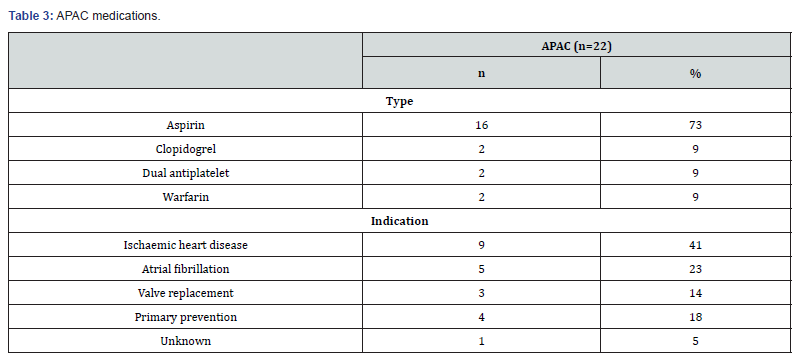
APAC medications (Table 3)
In this study, 19% (22 out of 118) of all emergency general surgical patients were on APAC. 82% of the patients (18 out of 22) were on single antiplatelet medication (aspirin or clopidogrel). two patients were on dual antiplatelet agents (aspirin, and clopidogrel or ticagrelor). No patient was on any of the novel oral anticoagulants (dabigatran, rivaroxaban or apixaban). The recorded primary indications for APAC medications include ischaemic heart disease (n=9, 41%), atrial fibrillation (n=5, 23%), valve replacement (n=3, 14%), and primary prevention (n=4, 18%).
Operations and anaesthesia (Table 4)
15% (11 out of 75 patients) of emergency general surgical patients requiring operations were on APAC. 11% of all laparotomies, and 25% of all gastroscopies were performed on patients taking APAC. The two patients who were operated for bleeding following surgery at another hospital were both in the APAC group. There was no statistically significant difference in the mode of anaesthesia chosen (general/sedation vs. spinal/regional) (p=0.36) nor seniority of staff performing the anaesthesia (p=0.73) between the two groups.

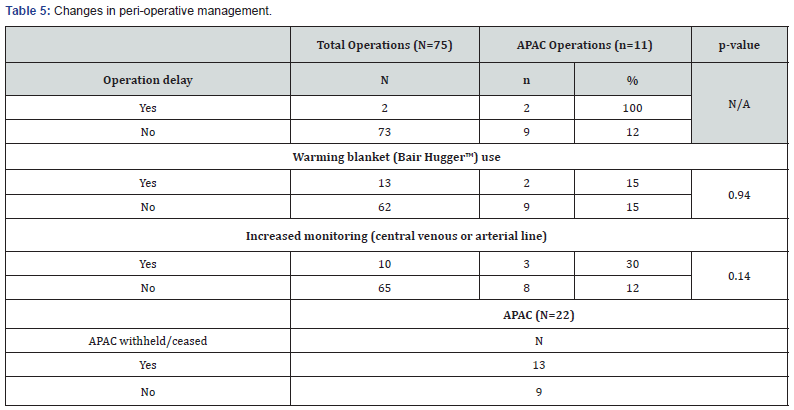
Changes in peri-operative management (Table 5)
59% (13 out of 22) of APAC patients had interruption or cessation to their medications, on average by 3.5 days (range 1-13 days). Two out of 75 emergency operations were delayed due to APAC usage. In this study, there was no statistically significant difference in the use of central venous or arterial line for increased monitoring between the two groups (p=0.14). There was also no observed difference in the use of a warming blanket (Bair Hugger™) between the two groups (p=0.94).
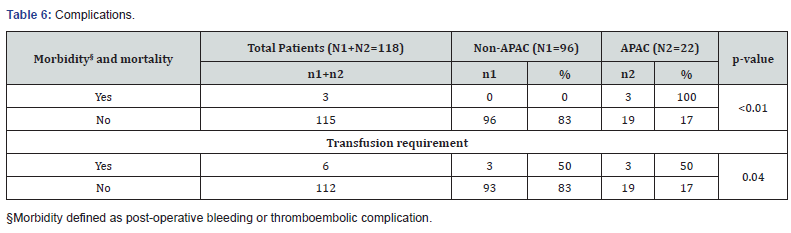
Transfusion, morbidity and mortality (Table 6)
The recorded morbidity (2 patients) and mortality (1 patient) in this study were all in the APAC group (p<0.01). The first complication was a 71-year old male on aspirin who had an appendicectomy and post-operatively developed coffee-ground vomiting. The second complication was a 63-year old female on aspirin who had a traumatic degloving lower limb injury. She was noted to have excessive blood loss at home shortly after discharge. There was no thromboembolic complication recorded. The single mortality in the study was of an 87-year old female on warfarin for mechanical mitral valve, who had a car accident and died shortly after in the Emergency Department from a cardiac arrest. Overall, six patients required transfusion, three from the non-APAC group and three from the APAC group (p=0.04).
Discussion
An increasing number of general surgical patients are being prescribed antiplatelet and anticoagulant medications (APAC) for various cardiovascular and cerebrovascular conditions. This widespread usage is on the rise especially in the face of increasing prescription of novel oral anticoagulants (direct thrombin inhibitor, anti-factor Xa). In our study, 19% of all emergency general surgical admissions were on APAC, with antiplatelet medications being the most prevalent (91%). The absence of any patients on novel oral anticoagulants in this study may reflect the prescribing practice in rural areas like Wangaratta. However, we predict that such prescribing practice will change with more prescription of novel oral anticoagulants. We speculate that a similar study conducted in a tertiary metropolitan hospital may reveal different prescribing patterns. In our current study, patients on APAC tend to be older, with the majority of them being 60 years old or older.
An increasing number of general surgical patients are being prescribed antiplatelet and anticoagulant medications (APAC) for various cardiovascular and cerebrovascular conditions. This widespread usage is on the rise especially in the face of increasing prescription of novel oral anticoagulants (direct thrombin inhibitor, anti-factor Xa). In our study, 19% of all emergency general surgical admissions were on APAC, with antiplatelet medications being the most prevalent (91%). The absence of any patients on novel oral anticoagulants in this study may reflect the prescribing practice in rural areas like Wangaratta. However, we predict that such prescribing practice will change with more prescription of novel oral anticoagulants. We speculate that a similar study conducted in a tertiary metropolitan hospital may reveal different prescribing patterns. In our current study, patients on APAC tend to be older, with the majority of them being 60 years old or older.
Emergency surgery exposes patients on APAC to increased risk of peri-operative bleeding. Depending on the estimated risk of peri-operative bleeding due to APAC, some of the patients on APAC will have their APAC withheld or ceased, and the required operation may have to be delayed until the effects of their APAC are reversed. In our study, 15% (11 out of 75) of all patients requiring emergency operation were on APAC medications, and of these two patients had their operation delayed due to APAC. Among the APAC medications, a warfarin reversal protocol was the most readily available at institutional and national level [1]. However, a more recently developed guideline in December 2018 now incorporates the perioperative management of the novel oral anticoagulants, including emergency reversal of dabigatran with idarucizumab in case of life-threatening bleeding or when an urgent procedure is required [2]. However, as observed in this study, the use of antiplatelet medications was far more prevalent, owing to their frequent usage in the primary and secondary prevention of many cardiovascular and cerebrovascular diseases. Despite their prevalence, there is currently no well-established clinical guideline specific to the management of patients on antiplatelet medications who require emergency general surgery [4]. Current guidelines are limited to the management of elective surgical patients with ischaemic heart disease who are on antiplatelet medications [2,5].
If the cessation of antiplatelet medication is judged essential due to high risk of operative bleeding, then the recommendation is to discontinue aspirin for five days, ticagrelor for five days, and clopidogrel seven days prior to the procedure [2]. However, this recommendation poses danger for high-risk patients as a large meta-analysis involving 50,279 patients on aspirin revealed that its withdrawal could increase the risk of cardiovascular events 3-fold with the average time from aspirin withdrawal to the onset of acute coronary syndrome being 10.7 days [6]. Also, the discontinuation of clopidogrel within 4-6 weeks following bare-metal coronary stenting poses the risk of the development of stent thrombosis with a high perioperative mortality of 20- 40% [7]. Hence, discontinuation of antiplatelet agents should be advocated only after a careful risk-benefit analysis where bleeding risk clearly outweighs that of cardiovascular events. In the elective surgical setting, the usage of bridging tirofiban and intravenous heparin has been described in three cases of patients with drugeluting stents for elective surgery where authors attributed the achievement of minimal surgical bleeding and absence of stent thrombosis to their usage [8].
In life-threatening surgical conditions where urgent or immediate surgical intervention is necessitated, there is lack of universal evidence-based guidelines to mitigate the effects of the antiplatelet agents. Platelet transfusion has the potential to restore normal platelet functions and limit haemorrhage progression in patients on antiplatelet agents, however, its efficacy and indications have not been fully established and clinical data are variable [9-12]; hence, their effectiveness of prophylactic use of platelet transfusions in trauma and emergency surgery for patients on antiplatelet agents remains controversial. Despite this, emergency platelet transfusion is frequently used in neurosurgical patients with traumatic brain injury on antiplatelet medications as these patients have an high mortality rate, and many advocate platelet transfusion regardless of the platelet count [13,14]. However, some authors argue that platelet transfusion in this setting does not reduce mortality rate either [15]. Furthermore, another study suggested that platelet transfusion does not restore platelet function for patients on clopidogrel, and it may only be effective for some patients on aspirin [9]. Platelet function tests, such as Verify Now™ are available to help identify patients who may benefit from platelet transfusion [9,16]. However, these tests are time-consuming and are not performed routinely in most hospitals. In our study, the two patients on antiplatelet agents who required transfusion did not receive any platelet transfusion.
A large cohort study showed that in patients with coronary stents, interrupting antiplatelet treatment by more than five days pre-operatively significantly increased the risk of cardiovascular or cerebrovascular thrombosis [17]. 59% of our APAC patients who had interruption to their medications did not have any thromboembolic complications. The mean duration of APAC interruption in this study was 3.5 days (range 1-13 days). For two patients with dual antiplatelet agents, only one of their medications was temporarily ceased.
In regard to impact of APAC usage on anaesthetic management, we hypothesised that due to multiple medical comorbidities and anticipation of increased blood loss, APAC patients would receive increased anaesthetic monitoring and hypothermia prevention. However, our data showed no statistically-significant difference in the use of central venous or arterial line and warming blanket between the two groups. APAC usage is often noted as a contraindication for neuraxial anaesthesia [18,19] due to increased risk of spinal haematoma with potential devastating neurological sequelae. In our study, we observed no difference in the anaesthetic technique (general/sedation vs. spinal/regional) used between APAC and non-APAC groups. This can most likely be contributed to the small sample size as only one patient in the study had a spinal anaesthesia in the non-APAC group.
The limitations of the study include the small number of recruited patients and that the data that is now 5 years old. In particular, we expect that the usage of novel oral anticoagulants would be much more prevalent if the study is repeated in the current time. Despite such limitations, we believe the current study serves as a useful baseline study to demonstrate the prevalence and effects of APAC in emergency general surgery patients in a rural hospital context. The scope for future research includes recruitment of a greater number of patients to incorporate those on novel oral anticoagulants.
Conclusion
From the highlighted cases of bleeding in APAC patients, we identified that decisions in regard to APAC interruption, type and amount of blood products used were often left up to the individual surgeon’s clinical decision. Apart from emergency warfarin reversal protocol, and more recently for emergency reversal of dabigatran with idarucizumab, there is still a lack of well-established, easily accessible guidelines for emergency management of APAC in non-cardiac surgery, in particular for patients on antiplatelet agents. We propose that such an evidencebased clinical guideline should incorporate APAC pharmacologic data, available coagulation tests, and possible reversal agents or blood products. This would require collaboration of specialist groups at institutional and national level, ranging from surgeons, haematologists, cardiologists, neurologists and anaesthetists. This would not replace clinical judgement for each individual patient but provide the essential guidance for judicious and effective use of blood products, along with identifying opportunities for future research.
To Know more about Open Access Journal of Surgery




No comments:
Post a Comment