Salivary secretory Ig A is characterized as a
considerable indicator for assessment of the risk of pathological
processes affecting periodontal tissues and structures. The initiation
and progression of the excretory system disorders of pyelonephritis and
nephrotic syndrome correlate to the necessity of frequent
hospitalizations of patients in child’s age. The aim of the study is to
be evaluated the gingival health status in children suffering from
pyelonephritis and nephrotic syndrome. In the study are applied
clinical, laboratory and statistical methods. Among the children with
diagnosed nephrotic syndrome is registered moderate negative correlation
between salivary sIg A and PLI, as well as moderate negative
correlation between salivary sIg A and GI. The healthy representatives
of the study are characterized with significant negative correlation
between the indicators of salivary sIg A and PLI, as well as significant
negative correlation between salivary sIg A and GI. The participants
with nephrotic syndrome are characterized with moderate negative
correlation between the clinical indicator of PLI and salivary pH level.
In the group of children with pyelonephritis is recorded significant
negative correlation between PLI and salivary pH. Among the healthy
representatives is registered extremely great negative correlation
between both of the indicators of PLI and salivary pH. Great negative
correlation between the clinical indicator of GI and salivary pH value
is ascertained among the representatives of the three groups included in
the study. The lowest level of secretory sIg A is registered among the
participants suffering from nephrotic syndrome. The increased
concentration of salivary secretory Ig A correlates to the lower levels
of the PLI and GI. The reduced level of sIg A in saliva predisposes to
initiation and progression of inflammatory reactions of the gingival
tissue.
Keywords: Gingival health; Children; Pyelonephritis; Nephrotic syndrome; Salivary Ig A
In saliva of healthy people can be determined
insignificant quantities of organic substrates, namely: bilirubin,
creatinine, triglycerides, cholesterol [1,2]. Salivary concentrations of
urea and uric acid are similar to these in plasm and can vary as a
consequence of metabolic disturbances such as kidney disorders [3], gout
[4] or metabolic syndrome [5]. Other essential organic molecules-
ascorbic acid and vitamin E, ensure the functionality of salivary
antioxidant protective system [6,7]. Salivary DNA is routinely applied
in many clinical laboratories for the purposes of assessment of
individual’s genetic predisposition towards some diseases. Saliva-based
assays are efficiently implemented for identification of HIV infection
[8], monitoring of the course of renal disorders [3], prevention of
cardio-metabolic risk [9], detection and quantitative evaluation of
viral nucleic acids [10], forensic medicine investigations [11], oral
health-related researches [12,13], as well as in condition of monitoring
of medicines’ abuse [14]. Ig A is detected in mucosa secretion,
precisely as an ingredient of saliva, tears, sweat, milk, and secretion
of respiratory, urinary, and gastro-intestinal tract. Ig A is produced
by plasmocytes of the
mucosa-associated lymphoid tissue. Secreted Ig A is connected to
glandular epithelial cells which are supplied with corresponding
receptors on their basal surface [15]. The main function of Ig A is to
connect to the microorganisms trying to colonize mucosa and to prevent
their adhesion upon epithelial cells [16]. As a marker of human immune
response, secretory Ig A fluctuates in conditions of local or common
status-related bacterial and viral infections. Based on profounf
investigations, A. Ivanova, A. Krasteva-Panova, Z. Krastev, established
that the referent values of secretory Ig A in mixed saliva of children
vary in the interval between 30-130 mg/L [17]. The synergetic and
additive interaction of secretory Ig A with other antibacterial
compounds in saliva such as lysozyme, lactoferine, peroxidase and
mucines have the potential to protect oral mucosa from penetration of
various antigens [18]. Some researchers accentuate on the interrelation
between low levels of salivary Ig A and enhanced susceptibility of the
organism to periodontal disorders [19-26].
Salivary secretory Ig A is characterized as a
considerable indicator for assessment of the risk of initiation and
progression of pathological processes affecting periodontal tissues and
structures
[27,28]. Simultaneously, an investigation among patients suffering
from differentiated forms of primary glomerulonephritis,
respectively: Ig A-related mesangyal nephritis, idiopathic
nephrotic syndrome, idiopathic membranous nephropathia,
accentuates on the establishment of significantly increased
concentration of immunoglobulins, and especially Ig A, in saliva
[29]. Urinary tract infections are characterized as inflammatory
processes which affect the topographic zone between the urethra
and renal parenchyme, clinically manifested with the compulsatory
symptom of bacteriuria. These excretory system disorders are
diagnosed in different periods of childhood, including the breastfeeding
period and early childhood. In condition of status febrilis
and anaemia with non-identified etiology in the age between one
and three years the diagnosis of pyelonephritis has to be taken
into consideration. In child’s age bacterial infections of the urinary
tract are ranged as second in distribution, following the infections
of the upper segment of the respiratory tract [30,31].
The aim of the study is to be evaluated the gingival health
status in children suffering from some renal disorders, namely
pyelonephritis and nephrotic syndrome.
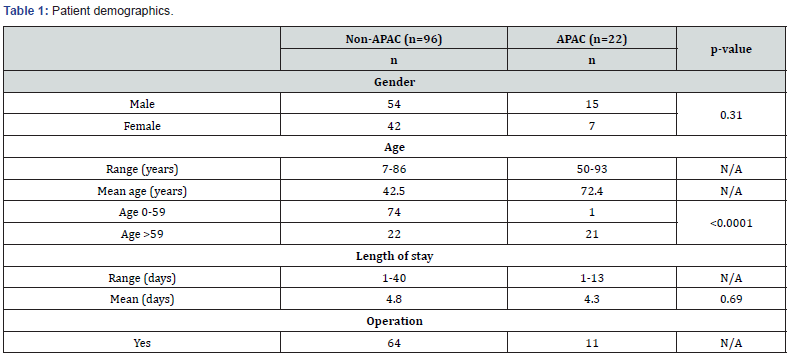
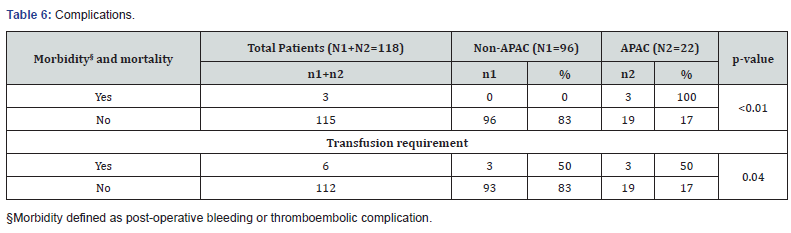
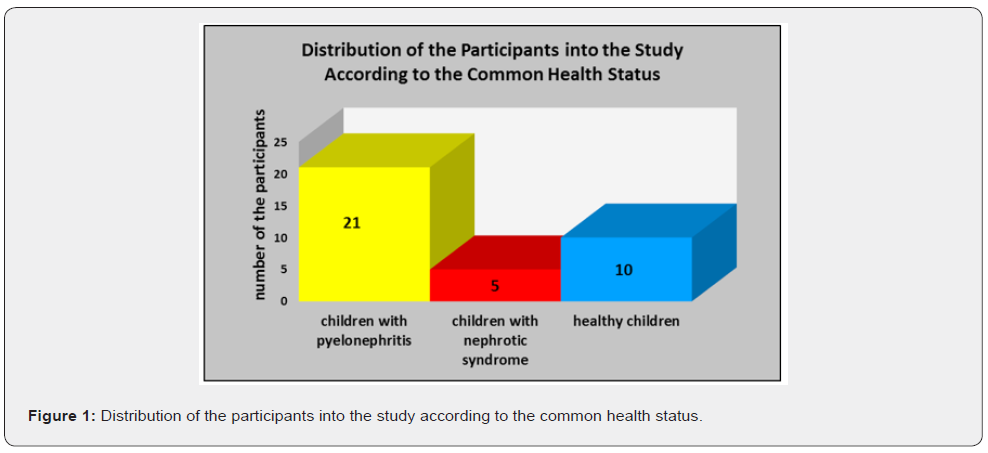
Subject of the study: A total number of thirty-six (36)
participants are included in our study. All of them belong to the
age interval of childhood, respectively up to the age of 18. These
children are divided into three groups according to their common
health status. The number of participants with diagnosed excretory
system disorders equals to twenty-six (26). A control group of
ten (10) healthy children also takes part in that investigation. A
declaration of informative consent has been signed by a parent or
guardian of each of the participants into the study (Figure 1).
In the context of that study are applied clinical methods,
laboratory methods and statistical methods.
The gingival status of the examined participants is
assessed by
the clinical indices of Plaque index by Silness-Lȍe (PLI) and Gingival
index by Lȍe-Silness (GI). By application of the plaque index PLI
Silness-Lȍe is evaluated the level of accumulated dental plaque on
teeth surfaces as an essential factor for initiation and progression
not only of carious lesions, but also of gingival inflammation. The
representative teeth which are included are. The level of dental
plaque is assessed with figures in the interval from 0 to 3, with
record of the medial, distal, vestibular and oral surfaces of all
the applied ramfjord teeth. The sum of figures illustrating the
plaque on ramjord teeth surfaces of each participant in the study
is divided to the total number of teeth surfaces, respectively 24,
which results in the average individual value of the plaque index
PLI Silness-Lȍe. B the means of the gingival index GI Lȍe-Silness is
ascertained the status of gingival inflammation. With the figures
from 1 to 3 is registered the degree of gingivitis of the same teeth,
respectively teeth surface as in the indicator of PLI Silness-Lȍe.
The figure of 0 corresponds to healthy gingiva, without symptoms
of edematization or bleeding. The figure of 1 associate to slight
degree of gingival inflammation, clinically manifested by slight
degree of edematization, without bleeding. The figure of 2 is equal
to moderate degree of gingivitis. The last is characterized with
edematized marginal gingiva and interdental papillae, combined
with the symptom of provoked bleeding (bleeding on probing).
The figure of 3 is related to severe degree of gingival inflammation,
which correlates to pathological morphological substrate,
interstitial edema in the zone of marginal gingiva and interdental
papillas and spontaneous bleeding. The sum of all the recorded
figures is divided to the total number of examined teeth surfaces,
respectively 24. As a result, is obtained average individual value
of the gingival index GI Lȍe-Silness for each of the participants
included into the study.
The level of salivary secretory Ig A is evaluated by
implementation of the method of radial immune diffusion. The
individually collected samples of non-stimulated mixed saliva are
collected in small containers with volume of 5 ml. The containers
are stored at t = - 80 ○C. The salivary samples are being centrifuged
for 15 minutes with 14000 revolutions per minute in condition of
t = 4 ○C. According to the protocol, on a special plate supplied with
outlined wells are deposited the centrifuged individual samples of
non-stimulated mixed saliva. The plate with the samples is stored
in its original package for providing proper level of humidity and
hermetization for the period of incubation of the samples for 72
hours in room temperature (t = 22 ○C). After the fixed interval of
72 hours is made a record of the diameter of the circle around each
well, measured in mm. Based on a monogram by the manufacturer
of the product, each value of all of the registered diameters
corresponds to a definite concentration of sIg A evaluated in mg/L.
Descriptive Analysis: The average value of n figures is
determined when the total sum of all figures is divided in their
whole number of n. The average value is the most widely applied
parameter of central tendency. The median is the value which
is in the middle position of the order of explored variables, or
that is the value which separates the cases aligned according to
the criterion of differentiation into two equal parts. Similar to
the average value, the median is a definite characteristic of each
statistical order and is unique for each sequence of data. The
standard error is the quantitative expression of the uncertainty of
the evaluation of the average value. Taking into consideration the
variable of standard error and the rate of probability, the actual
level of average value for the whole population is calculated in the
range of average value plus/minus the standard error in terms of
the fixed rate of probability. That is related to the variable of the
interval of confidentiality. In the context of our investigation the
interval of confidentiality equals to 95%.
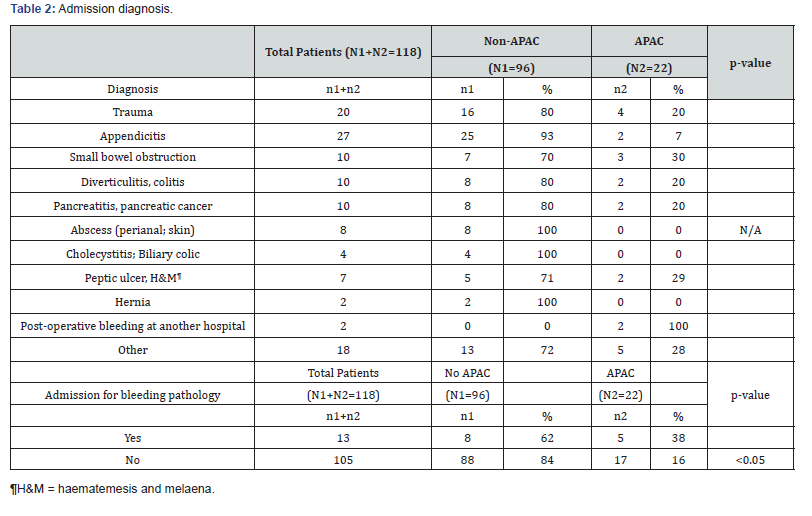
Correlation Analysis: One of the main tasks of statistical
analysis in the scope of medicine science is related to
determination and establishment of interrelations between
various events and phenomena, figured out at definite levels. The
interrelation between the factorial characteristic and several or a
great number of variations of the results-associated characteristic
is defined as an interrelation of correlation. The coefficient of
correlation by Pearson evaluates the significance of the linear
interrelation between two variables. There is a five degreerelated
scale of evaluation of correlation between two parameters
based on definite intervals of variations of the coefficient of
correlation by Pearson. In the interval between 0,00 and 0,25 is
registered slight correlation. In the interval between 0,26 and
0,49 is evaluated moderate correlation. The interval of values of
the coefficient by Pearson between 0,50 and 0,69 corresponds
to significant correlation. The interval of values of the coefficient
of correlation by Pearson between 0,70 and 0,89 regards to the
condition of great correlation, and in the interval between 0,90
and 1,00 is established extremely great correlation. The positive
interrelation of correlation is characterized with simultaneous
increase or decrease of both of the investigated variables. The
negative interrelation of correlation is marked out with elevation
of the values of one of the explored parameters and reduction of
the values of the other one (Figure 2).
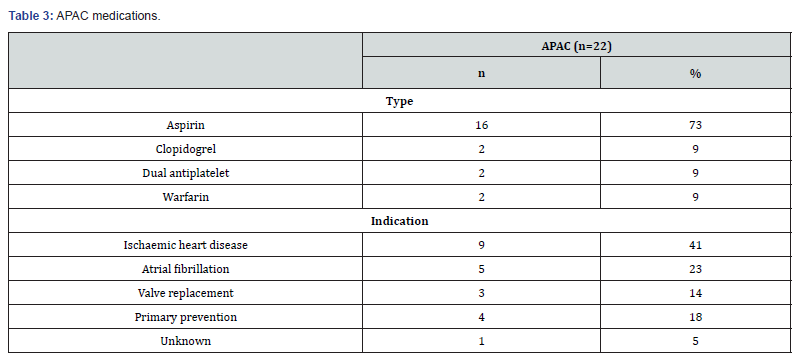
The lowest average value of the indicator of
secretory salivary
Ig A, namely 33,5920 mg/l, is established among the examined
children with diagnosed nephrotic syndrome. Among the
participants suffering from pyelonephritis and healthy children
are registered similar values of this parameter of sIg A, respectively
58,7143 mg/l and 56,8800 mg/l. The lowest value of the median
of secretory Ig A is recorded among the patients with nephrotic
syndrome, namely 40,0000 mg/l. The healthy participants and
children with established pyelonephritis are characterized with
similar levels of that indicator, respectively 52,2000 mg/l and
52,1000 mg/l. The lowest minimal value of sIg A amounts to 4,06
mg/l and is recorded among the examined patients with nephrotic
syndrome. Greater minimal value of secretory Ig A, equal to 12,80
mg/l, is registered for the healthy controls. The highest level of that
indicator is related to the representatives of the study with the
diagnosis of pyelonephritis, respectively 14,70 mg/l. The lowest
maximal value of the variable of salivary sIg A, namely 57,2000
mg/l, characterizes the participants in the study with diagnosed
nephrotic syndrome. Among the participants without common
health disorders the maximal value of sIg A amounts to 123,0000
mg/l. In the group of patients suffering from pyelonephritis is
ascertained the maximal value of sIg A equal to 130,0000 mg/l.
With the highest average value of the Plaque Index by Silness-
Lȍe (PLI), respectively 1,8640, and the highest average value
of the Gingival Index Lȍe-Silness (GI), respectively 1,6020, are
characterized the children suffering from nephrotic syndrome.
Among the patients with diagnosed pyelonephritis and healthy
controls are recorded similar levels of the average value of PLI
equal to 1,3957 and 1,3010, respectively. The average values of GI
among the participants with pyelonephritis and children without
common health disorders amount namely to 1,0390 and 1,0150
(Tables 1-3). Based on the calculated coefficient by Pearson
there have been established definite interrelations. Among the
patients suffering from pyelonephritis has been recorded slight
negative correlation between salivary sIg A and the Plaque index
PLI, as well as between salivary sIg A and the Gingival index GI.
Among the children with diagnosed nephrotic syndrome has been
registered moderate negative correlation between salivary sIg A
and PLI, as well as moderate negative correlation between salivary
sIg A and GI. The healthy representatives of the study have been
characterized with significant negative correlation between the
indicators of salivary sIg A and PLI Silness-Lȍe, as well as with
significant negative correlation between salivary sIg A and GI Lȍe-
Silness (Graph 1).
Among the participants with the diagnosis of nephrotic
syndrome has been ascertained moderate positive correlation
between the indicator of salivary sIg A and salivary pH. Children
without common health disorders included in the investigation
confirm similar level of moderate positive correlation between
both of these variables of salivary pH and sIg A (Graph 2).
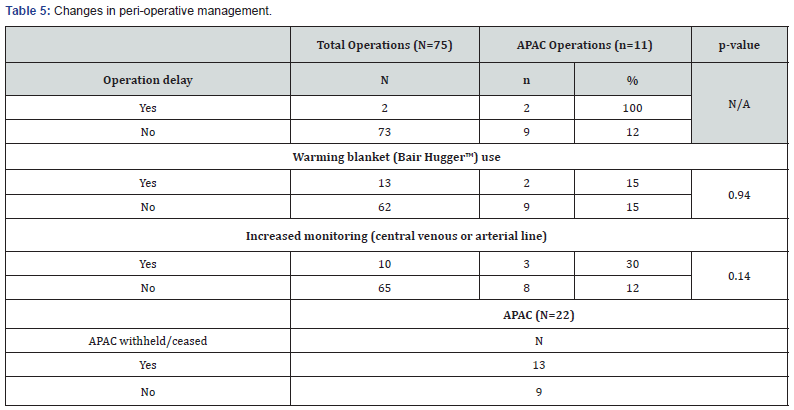
Among the patients suffering from nephrotic syndrome there
has been recorded great positive correlation between the clinical
parameters of the Plaque Index PLI Silness-Lȍe and Gingival
Index GI Lȍe-Silness. The children with diagnosed pyelonephritis
and healthy controls in the study have been characterized with
extremely great positive correlation between the indices of PLI
and GI (Graph 3). The participants with the diagnosis of nephrotic
syndrome have been characterized with moderate negative
correlation between the clinical indicator of PLI Silness-Lȍe
and salivary pH level. In the group of children with established
excretory system disorder of pyelonephritis has been recorded
significant negative correlation between the Plaque Index PLI
and the para-clinical parameter of salivary pH. Among the healthy
representatives in the investigation has been registered extremely
great negative correlation between both of the indicators of PLI
and salivary pH (Graph 4). Great negative correlation between
the clinical indicator of GI Lȍe-Silness and salivary pH value
has been ascertained among the representatives of the three
groups included in the study, namely in the group of patients
with pyelonephritis, in the group of participants with nephrotic
syndrome and among the healthy controls (Graph 5).
The results obtained in the context of our study are based
on the explicitly manifested interrelations between the local
immunity factor of salivary secretory Ig A and the specifics of
common health status on individual and group level. There are
definite, considerable correlations between local immunity
into oral cavity and basic clinical parameters of the state of
gingival tissue complex. A scientific investigation accentuates
upon the interrelations between the salivary secretory Ig A in
its role for physiological, functional and clinical manifestation
of local acquired immunity in oral cavity, from one side, and
effectors on systemic and local level, on the other side [37]. The
secretory Ig A is characterized as a fundamental indicator for
proper assessment of the level of risk of alteration of hard teeth
tissues and periodontal structures in condition of pathological
processes [27,28]. Among some of the participants in our study
with the diagnosis of nephrotic syndrome is verified moderate
negative correlation between sIg A and the Plaque Index PLI.
Simultaneously, there is negative moderate correlation between
the parameters of sIg A and the Gingival Index GI. Immunesuppressive
activities of corticosteroids perform inhibiting effect
upon the protective mechanisms of local immunity in oral cavity.
This is related to suppression of the synthesis and secretion of
salivary immunoglobulins, including immunoglobulin A (Ig A)
[17,18,33]. In parallel, the common health disorder of renal failure
is associated with a definite increase of blood and salivary urea
level with risk of establishment of the pathological state of uremic
stomatitis. The elevated rate of urea in blood and saliva is related
to considerably lower distribution of non-cavitated and cavitated
carious lesions, but to enhanced risk of gingival and periodontal
disease [38-42]. We confirm the key role of secretory Ig A in
non-stimulated mixed saliva as a plaque-inhibiting indicator,
with suppressive activity against progression of the gingival
inflammatory process.
In the context of a study performed by Rashkova et al.
[26] a number of thirty (30) children without common health
disorders and with clinically healthy gingiva are compared with
thirty (30) children also without somatic deviations, but with
clinically manifested plaque-induced gingivitis. In the group of 30
children with diagnosed gingivitis the average value of salivary
sIg A amounts to sIgA= 41,07±32,14 μg/ml. The group of 30
healthy participants at child’s age with no symptoms of gingival
inflammation are characterized with higher average value equal to
sIgA=48,3±32,41 μg/ml. There has been established a statistically
significant correlation between sIgA and the plaque index PLI
Silness & Lȍe (p< 0,05). There has been ascertained no correlation
between salivary sIg A and the degree of bleeding on probing
(BoP). The parameter of sIgA is evaluated as a variable with
considerable significance of assessment of the risk of pathological
processes with impact upon oral cavity tissues. Secretory Ig A
in the medium of non-stimulated mixed saliva performs plaqueinhibiting
activity with key control function against advancing of
the gingival inflammatory process [27]. In our study the children
suffering from nephrotic syndrome are treated by application of
corticosteroids [34-36]. In the specific therapy-related conditions
of that excretory system disorder salivary sIg A is characterized
with caries-protective activity against initial carious lesions and
indirect impact upon the levels of plaque and gingival indices.
Based on the principles determined into the researches by
Kiselova [17] and Dencheva et al. concerning the behavioral
patterns of dental medicine doctors towards patients suffering
from urinary tract infections, we accentuate on the explicit
necessity of regular visits at dentist’ s office on each three
months. The purpose of these appointments is associated to the
performance of professional complex oral-hygiene procedures in
combination with programs for motivation and re-motivation of
patients [17]. The infections affecting hard teeth structures and
periodontal tissues have to be adequately and radically treated
[43-48].
The specifics of clinical manifestation and therapeutic
protocols of the excretory system disease of pyelonephritis
correlate to numerous factors with negative influence on the
processes of formation of enamel, respectively on its qualitative
and quantitative traits. There have been investigated the adverse
effects of wide spectrum antibiotics [49-52], limitation of proteins’
consumption in condition of modified dietary regime, with
prevailing frequency of intake of cariogenic foods [53], recurrent
episodes of sub-febrile and febrile body temperature [54]. These
variables combined with the need of application of steroid antiinflammatory
drugs concern the disease of nephrotic syndrome.
All of these factors serve as definite prerequisites for impingement
of oral-dental health and disturbance of the periodontal status of
the patients with excretory system disorders of pyelonephritis
and nephrotic syndrome [55].
In the context of profound, thorough investigations of
the salivary marker of pH is ascertained its essential role of a
considerable factor for initiation and progression of the carious
process [56-58]. In our study we accentuate on the interelations
between dynamics of salivary pH levels and gingival health status in
children with diagnosed nephrotic syndrome and pyelonephritis.
In parallel, the researchers A. Ivanova, A. Krusteva and Z. Krustev
evaluate the average value of pH in mixed saliva equal to 7,2 [17].
The limited consumption of foods rich in proteins, with respect
to protection of the renal system from functional overload, is
compensated with considerable amounts and high frequency
of intake of sugar-containing products among the participants
with established nephrotic syndrome and pyelonephritis. As a
consequence of performance of this explicitly modified dietary
regime there is a considerable number of episodes of reduction
of salivary pH level, facilitating the inflammatory process of the
gingival tissue [56,59].
1. The lowest level of secretory Ig A in saliva is registered
among the participants suffering from nephrotic syndrome.
2. The increased concentration of salivary secretory Ig A
correlates to the lower levels of the Plaque Index PLI and the
Gingival Index GI.
3. The reduced level of secretory Ig A in saliva predisposes
to initiation and progression of inflammatory reactions of the
gingival tissue.
To Know more about Dentistry & Oral Health