Pulmonary & Respiratory Sciences - Juniper Publishers
Abstract
Objective: Diabetic feet and toe deformities
is commonly associated with diabetes mellitus and neuropathy is the
causative factor combined with vasculopathy. In this study we list out
various morphological changes which occur in Diabetic foot lesions, the
pathophysiology and the management of the deformed toes and feet.
Materials and Methods:A prospective study was
carried out in patients presenting to the Diabetic Clinic at a tertiary
care hospital in Delhi. 70 patients who were labelled as diabetics
formed the study group.
Results: The most common age group affected
belonged to 51-60 age bracket which included 41 patients (58.5%). The
male to female ratio was approximately 3:1. Majority of patients 32
(45.71%) had diabetes of >10 years duration. Foot and toe deformities
affected majorly diabetics with moderately controlled diabetes mellitus
and the study revealed that 40 patients (57.2%) had moderately
controlled diabetes with blood sugar levels ranging from 160-200 mg/dl.
The highest number of patients i.e. 29 patients (41.4%) who had foot/
toe deformities were on oral hypoglycaemic agents. Clawing of the toes
(26 patients, 37.14% of patients), was the commonest morphological
change in the architecture of the foot followed by Varus deformities (17
patients, 24.28% of patients). Nail changes in the form of
hypertrophied and brittle nails affected 37 patients (52.85%).
Conclusion: We concluded that team approach,
adequate diabetic control combined with patient education about foot
care and footwear will help prevent complications and improved quality
of life of the patients suffering from diabetic foot and toe
deformities.
Keywords: Diabetic foot; Toe deformities; Hammer toes; Hallux valgus; Bunion; Claw toes; Charcot’s foot
Introduction
Foot problems are common in patients with diabetes,
often requiring prolonged and costly hospital stay and eventually
leading to lower extremity amputation [1]. Motor neuropathy affects the
function of the intrinsic and extrinsic musculature of the foot, thus
upsetting the delicate balance between flexors and extensors of the toes
[2]. Atrophy of the small muscles responsible for metatarsophalangeal
plantar flexion is thought to lead to the development of hammertoes,
claw toes and prominent metatarsal heads [3]. The prevalence of all
diabetic foot complications increased clearly with age and diabetes
duration [4]. Clinical recommendations for people with diabetes include
provision of special footwear to individuals with foot risk factors [5].
Aim
To study the morphological changes in the form of
foot and toe deformities occurring in diabetic patients presenting to a
tertiary care centre in New Delhi, India.
Materials and Methods
A prospective study was carried out in patients
presenting to the Diabetic Clinic at a tertiary care hospital in Delhi.
The patient profile comprised of patients who were known Diabetics or
recently detected diabetics under treatment and follow up and had
obvious foot and/or toe deformities. A detailed history regarding foot
and toe deformities was followed by a thorough physical examination and
the following were noted: -
1) Age and sex of the patient
2) Duration and severity of Diabetes.
3) Treatment by Oral Hypoglycaemic agents and / or Insulin/p>
4) Evidence of Neuropathy -loss of touch,
vibration, temperature sensation, using a 10gm monofilament, 128 Hz
tuning fork, deep tendon reflexes were examined using percussion hammer.
5) Evidence of ischaemia – thinning of skin, loss of
subcutaneous fat, hair loss, brittle hypertrophied nails,
callous formation, ulceration, peripheral pulses and venous
filling time were noted.
6) Foot and/or toe deformities
7) Nail changes
Results
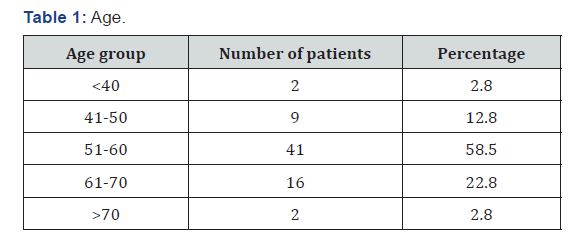
Out of the 70 patients, 2.8% were below 40 years of age, 9
patients (12.8%) were in the group between 41-50. 41 patients
(58.5%) belonged to the 51-60 age group, 16 patients (22.8%)
were in the 61-70 age group and only 2 patients were in the age
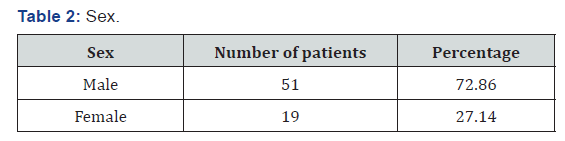
group above 70 years (Table 1). Out of 70 patients, 51 patients
(72.86%) were males and 19 patients (27.14%) were females
who presented with various foot and toe deformities (Table
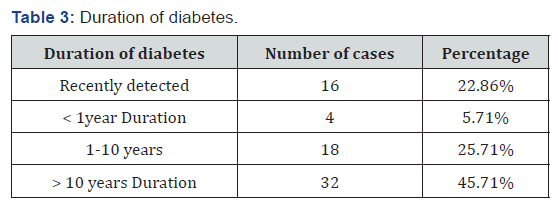
2). Of the 70 patient, 16 patients (22.86%) were detected to
have diabetes during their first presentation to the hospital. 4
patients (5.71%) had foot lesion with diabetes of less than 1year
duration, while 18 patients (25.71%) had diabetes of <10 years
duration (Table 2). Majority of patients 32 (45.71%) had diabetes
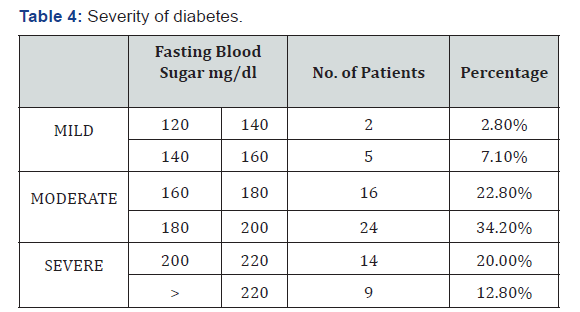
of >10 years duration (Table 3). Only seven patients (10%) had
well controlled blood sugar levels, 40 patients (57.2%) had
moderately controlled diabetes with blood sugar levels ranging
from 160-200mg/dl.23 patients (32.8%) had poorly controlled
diabetes (Table 4). 16 patients (22.8%) were unaware about
their disease hence were taking no treatment (Table 3). 29
patients (41.4%) were only on oral hypoglycaemic agents, 14
patients (20%) were being managed with insulin, 11 patients
(15.7%) were being treated with both oral hypoglycaemic agent
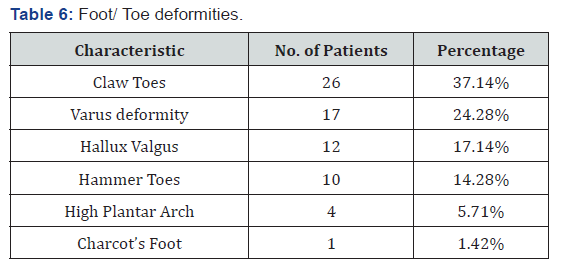
and insulin (Table 5). Clawing of the toes (26 patients, 37.14%
of patients), was the commonest morphological change in
the architecture of the foot followed by Varus deformities (17
patients, 24.28% of patients) . Hallux valgus (17.14%), Hammer
toes (14.28%), high plantar arch (5.71%) and Charcot’s foot was
seen only in two (1.42%) patients (Table 6).

Nail Changes
Hypertrophy with brittle nails (52.85%) were seen in 37
patients.
Follow Up
All patients were followed up at monthly intervals whenever
they used to come to collect their medicines for diabetes. They
were given specific advice about foot care and footwear.
Discussion
Normal foot
The skin of the healthy foot is elastic but resilient. It should
not show signs of scaliness, dryness or brittleness, nor should it
be thin and shiny. Plantar skin is about twice as thick as that on
the dorsum, is tougher and moves less readily over the deeper
structures.
Gait cycle
During walking the weight is taken first on the point of the
heel (“heel strike”). It is then transferred smoothly to the outer
aspect of the sole and the metatarsal heads of the second to fifth
toes. It then shifts medially to the foot (first metatarsal head) and
the body is propelled forward by flexion of all the metatarsals,
and of the big toe (“toe off”). This smooth transfer of forces is
lost when the foot loses its normal plantar arch, or the ligaments
and soft tissues become less elastic. The result is that some parts
of the sole take increased pressure and therefore become liable
to neuropathic ulceration. This is most likely to occur over the
second and third metatarsal heads, and the big toe.
Diabetic foot
Diabetic foot
Peripheral neuropathy
Sensory Neuropathy: Diabetes leads to abnormal function of
peripheral nerves due to Metabolic causes –due to accumulation
of sorbitol. Ischaemia - the nerves dependent on the vasa nervous
for their nutrient supply which suffer ischaemic damage from
microvascular disease.
Motor neuropathyy
The integrity of the arch of the foot is preserved by muscles,
ligaments and connective tissue. The muscles become weak
and atrophic when affected by motor neuropathy. This causes
loss of normal balance between the toe flexors and extensors;
hence the persons may develop either a flat foot or one which is
excessively clawed.
Autonomic neuropathy
Vasomotor: The fine control of distribution of blood is
dependent on the action of Vasomotor nerves. These are
responsible for opening and closing of arterioles and venules
such that blood is shunted to the areas where it is most needed.
The foot affected by autonomic neuropathy may have abnormal
distribution of blood even though the macrovascular supply is
good. The altered blood flow due to arterio-venous shunting
leads to increased bone turnover, resorption and destruction
of bones and joints called the Charcot’s joint. Charcot joint
was considered when bones, joints, and soft tissues of the foot
and ankle are inflamed in the presence of neuropathy with or
without history of trauma leading to variable degrees of bone
destruction, subluxation, dislocation, and deformity [8].
Sweating
Autonomic neuropathy may result in sudomotor dysfunction
leading to abnormal sweating and dry skin with cracking
and fissuring facilitating the bacterial infection of the foot
[9]. The risk for diabetic foot ulceration increases by sevenfold
in patients with peripheral diabetic neuropathy [10].
45% to 60% of all ulcerations in patients with diabetes are
mainly due to neuropathy, while 45% of the ulcers are due to
combined neuropathic and ischemic factors [10]. Distal bilateral
symmetrical neuropathy is the commonest presentation and
usually starts in the lower limbs, has a progressive course. It
usually presents in a glove and stocking pattern of abnormal
sensations [11]. “Burning feet syndrome.” is a form of neuropathy
which arises at night and is accompanied by high sensation of
pain [12]. Peripheral neuropathy is accompanied by autonomic
neuropathy in 30% to 50% of cases [13]. The foot skin affected by
autonomic neuropathy is dry and fissured with the consequence
of finding a reduced protective skin function and thus increased
risk of injury.
Lesions of neuropathic foot
a) The foot is typically pale and puffy, with clawing of toes.
The skin is dry and fissured and the planter arch may be
exaggerated. Clawed toes are defined as toes with extension
of the metatarsophalangeal joint and flexion of the proximal
and distal interphalangeal joints. Claw toes is caused by an
imbalance between the extrinsic and intrinsic foot muscles
[14].
b) Hammer toes: The metatarsophalangeal joint of the
first digit is extended, and the proximal interphalangeal
joint is flexed. Atrophy of the small muscles responsible for
metatarsophalangeal plantar flexion is thought to lead to the
development of hammer toes [15].
c) Varus deformities: The third, fourth and fifth toes drift
medically due to muscle imbalance, to gouge adjacent toes
producing ulcers.
d) Hallux Valgus: Hallux valgus is defined as a lateral
angulation of the first MTP joint of the great toe [16].
e) Tailor’s Bunion: It is an exostosis of the lateral part
of the fifth metatarsal head which is associated with Varus
deformity.
f) Charcot’s foot: It is a rare but serious complication of
the diabetic foot. It occurs in less than 1% of people with
diabetes, most commonly during the fifth and sixth decade
in insulin dependent patients.
The duration of diabetes is usually greater than 12 years.
Normally it develops unilaterally, but in 20% of patients
it develops bilaterally. It is defined as a chronic, painless
degenerative process affecting the weight bearing joints of the
foot. The ethology is thought to be repeated minor trauma in a
neuropathic foot and due to arterio- venous shunting. Charcot’s foot develops through 3 stages, described by Eichholtz in
1966. Eichholtz stage 1 is characterized by acute inflammation
associated with hyperaemia and erythema. During this stage,
the bone softens and fragments, fracture dislocations occur,
with pure dislocations more common. Stage 2 is characterized
by bony coalescence, reduction in swelling of the foot, and
periosteal new bone formation. In stage 3 bony consolidation
and healing occurs. Normally, this whole process lasts about 2 to
3 years, although progress through the stages can be quite rapid.
Limited joint mobility
Diabetes causes abnormalities of the connective tissue due
to glycosylation of proteins like collagen which renders it stiff
and inflexible. These changes restrict foot mobility, which while
walking leads to trauma and ulceration.
Management of Foot and toe deformities in Diabetes Mellitus
Multidisciplinary foot care team consisting of diabetologist,
surgeon, diabetic nurse, chiropodist and orthotist forms the foot
care team.
Skin care
The feet are often dry and scaly as a result of anhidrosis
secondary to autonomic neuropathy. Regular applications of
moisturizing creams will help soften the skin and prevent skin
fissures which might get infected.
Nail care
Obesity and poor eyesight prevent elderly patients to cut
their nails properly which may lead to damage of the adjacent
skin or may leave a portion of nail uncut, resulting in an
ingrowing toenail (Figure 1). The toenails should be cut short
with no remaining sharp edges. Mycological infections should be
diagnosed early and be treated. A grossly deformed mycotic nail
should be treated by nail excision.
Use of proper footwear
Proper footwear help reduce points of high pressures. In
most of the cases, the problem is caused by arching of the foot
resulting in high pressure at the metatarsal heads. Custom Fitted
Shoes should have generous instep support to re-distribute the
weight more evenly (Figure 2). The problem of clawing is that
there is an increased requirement of a deep shoe. The principle
of good footwear is to provide a shoe which is deep, broad but
not floppy. The material should be soft with good in step support.
Bespoke footwear may be needed for feet which are grossly
deformed following Charcot’s arthropathy.
Conclusion
Diabetes affects the foot in various ways including lesions
affecting the skin, nails, bones and connective tissues. Team
approach, adequate diabetic control combined with patient
education about foot care and footwear will help prevent
complications and improved quality of life of the patients
suffering from diabetic foot and toe deformities. Studies have
confirmed that inappropriate footwear is the most common
source of trauma and cause of ulceration in patients with
diabetes [17] and hence patients with diabetes should be
educated regarding use of proper footwear.
To Know more about Pulmonary & Respiratory Sciences
Click here: https://juniperpublishers.com/ijoprs/index.php
Click here: https://juniperpublishers.com/ijoprs/index.php
To Know more about our Juniper Publishers
Click here: https://juniperpublishers.com/index.php




Because of US estrangement from Cuba most diabetic foot ulcer patients may be unaware that Cuban medication called Heberprot-P (www.doctorcuba.com) has cured thousands of people from toe amputation.
ReplyDelete