Reproductive Medicine - Juniper Publishers
Abstract
We describe collaboration between obstetrician
leaders in low resource countries and MFM specialists in promoting a
systematic approach to maternal mortality cases reviews and targeting
feasible quality improvement projects. This effort cumulated in the
presentation and reviews of representative cases of maternal mortality
by emerging obstetrician leaders from Ghana, Uganda, India and Haiti at
the Global Health Scientific Forum of Society of Maternal Fetal Medicine
Annual Meeting in 2012. In addition to large-scale initiatives, groups
of maternal healthcare providers can develop similar global partnership
that can facilitate the goal of reducing global maternal mortality.
Abbreviations:
MDG: Millennium Development Goals; ACOG: American college of
Obstetricians and Gynecology; US: United States; MFM:
Maternal-Fetal-Medicine; SMFM: Society of Maternal Fetal Medicine; RCA:
Root Cause Analysis
Introduction
Maternal mortality is defined as the death of a woman
while pregnant or within 365 days of the end of pregnancy, from any
cause related to or aggravated by the pregnancy or its management, but
not from accidental or incidental causes [1,2]. The Millennium
Development Goals (MDG) 5 signed by 189 heads of state, calls for a 75%
reduction in the global maternal mortality 1990 and 2015 [3]. In 2011,
the world maternal mortality was reported to have decreased from 409,100
in 1990 to 256,300 deaths, a 38% decrease, with only 13 countries noted
to be on track to achieve MDG5 [3]. Overall progress in decreasing
maternal mortality has been inadequate and inconsistent, especially in
low resourced countries. This has resulted in urgent efforts to tackle
maternal morality such as the United Nations Global Strategy for Women’s
and Children’s Health; Saving Mothers, which is a partnership between
American college of Obstetricians and Gynecology (ACOG), United States
(US) and Norwegian governments focusing on the critical 24 hours of
labor & delivery [4]. However, more interventions are needed by more
maternal health organizations, institutions and physicians’
stakeholders to decrease maternal mortality and achieve MDG5.
Purpose
The purpose of this report is to describe a
collaborative process between obstetrician leaders in low resource
countries
and US Maternal-Fetal-Medicine (MFM) specialists in promoting a
systematic approach to maternal mortality cases reviews, identifying
system issues that impact safe care, targeting feasible quality
improvement projects that may lead to a reduction of maternal mortality
in developing countries, and the presentation of representative cases of
maternal mortality for discussion and review at the Global Health
Scientific Forum of Society of Maternal Fetal Medicine Annual Meeting in
2012. Our goal was also to suggest feasible educational
programs based on our experiences that can be adopted by physicians in
resource-high countries who are interested in supporting and
collaborating with counterparts in low-resource countries in the effort
to develop a culture of safety, in-depth blame free maternal mortality
reviews and opportunities to improve the health care delivery system in
order to decrease maternal deaths.
Process
This program occurred as a result of the interest
and efforts of the members of the Society of Maternal Fetal Medicine
(SMFM) sub-committee on Global Health. This committee is committed to
improving the health of women and children in underserved international
communities. The purpose was to identify effective strategies to address
maternal mortality in underserved communities using the following
processes.
1) The first step required that MFM specialists interested in
global health identify and develop a professional, collaborative
and mentoring relationship with an emerging physician leader
from a facility in a low resource country.
2) The next step ensured that the MFM specialists sustain
and maintain an ongoing relationship with the low-resource
emerging leader through bilateral visits, consultations and
electronic teleconferences, emails and other communication
methods.
3) Best practice for root cause analysis (RCA) for maternal
mortality review was promoted. Root cause analysis (RCA)
is a structured method used to analyze serious adverse by
identifying underlying problems that increase the likelihood
of errors while avoiding the trap of focusing on mistakes by
individuals. The goal of RCA is to identify both active errors
(errors occurring at the point of interface between humans
and a complex system) and latent errors (the hidden problems
within health care systems that contribute to adverse events).
RCA generally involves a multidisciplinary team follow a
protocol that begins with data collection and reconstruction
of the event in question through record review and participant
interviews. The ultimate goal of RCA is to prevent future harm
by eliminating the latent errors that underlie adverse events
[5, 6].
4) The low-resource leaders were invited to an inaugural
scientific forum on Global Maternal Mortality at the annual
meeting of the Society for Maternal Fetal Medicine in February
2012. Each member presented a case history that was
representative of one of the key drivers of maternal mortality,
followed by root cause analyses with US MFM experts
facilitating discussions in a global context. The cases were
presented using the 3-delay model (delay in making decisions
to seek medical care, delay in reaching an appropriate facility,
delay in receiving appropriate care on reaching facility) [7],
which recognizes that timely and adequate treatment for
obstetric complications are major factors in reducing maternal
deaths.
5) A fishbone analysis was also developed for each case
presented. A fishbone diagram, also called a cause and effect
diagram or Ishikawa diagram, is a visualization tool for
categorizing the potential causes of a problem in order to
identify its root causes [8,9].
6) Post-conference, MFM experts-maintained contact and
support with the low resource countries with continued
support for the confidential review system and a focus on
implementing feasible quality improvement projects that
could improve safe care and decrease maternal mortality.
Cases
The four emerging physician leaders were from Uganda, Ghana,
Haiti, and India. These were the countries that the MFM specialists
were able to develop sustainable professional relationships with
local physician leaders. These relationships had been ongoing for
approximately 2 years prior to the SMFM conference. The cases
presented at the Global Health Scientific Forum of the Society
of Maternal Fetal Medicine reflected the leading direct causes
of maternal death – septic abortion, obstetrical hemorrhage,
obstructed labor and preeclampsia.
Septic abortion, accra, ghana
A thirty-seven-year-old Para 5 with three months amenorrhea
procured herbal preparations from a street vendor to terminate
her pregnancy in secrecy. This was unsuccessful, so she obtained
an illicit pregnancy termination at an unidentified private clinic.
On post-operative day 4, she developed severe abdominal pain
and her husband took her to a district hospital. She did not
reveal any information about a pregnancy nor an unsafe abortion
attempt. She was evaluated, but a pelvic examination was not
done. She was admitted for presumed pneumonia with sepsis
and given antibiotics, fluids, and 1 unit of blood. On hospital day
3, she developed fever, productive cough with vaginal bleeding
and passage of tissue. A diagnosis of pelvic abscess was made;
patient had referred her to the tertiary hospital approximately 30
kilometers away by public transport.
Upon arrival, she was febrile, jaundiced, hypotensive and
anuric. She had bronchial breath sounds, tender and distended
abdomen, 12 weeks sized tender uterus, and dilated cervix with
offensive products of conception. The diagnosis was septicemia
secondary to septic incomplete abortion and pneumonia.
Confronted with the physical findings, patient revealed the
history. She did not volunteer information about her termination
previously because of the presence of her husband. She was
resuscitated with normal saline, oxygen and broad-spectrum
antibiotics. Eight hours later, she was taken to the operating room
for uterine evacuation. The cervix was edematous, friable with a
laceration but no evidence of uterine perforation. Very offensive
and copious placental tissue was removed.
Post-evacuation, she was critically ill with unstable blood
pressure, tachycardia and oliguria. Intravenous antibiotics and
blood transfusion were continued. Ten hours post-evacuation
she had a cardiac arrest but recovered after cardiopulmonary
resuscitation. She deteriorated and was declared clinically dead
about ninety-six minutes after the cardiac arrest. Postmortem
diagnosis was bilateral lobar pneumonia with septic abortion.
Septic abortion fishbone and root cause analysis: A fish
bone diagram Figure 1 highlights the problems identified during
the discussion that were considered potential root causes of her
death. These included unwanted pregnancy, inadequate access to
and knowledge about family planning services. By not disclosing
her attempts at pregnancy termination she contributed to a delay
in diagnosis, although an incomplete assessment was performed
at the district hospital. Once transferred to the referral hospital,
resources were limited. Lack of formal education and male dominance are also major factors in this case of mortality from the
complications of an unsafe abortion. At least one in five Ghanaian
women age 15-49 years have no formal education, compared to
one in eight for Ghanaian men.
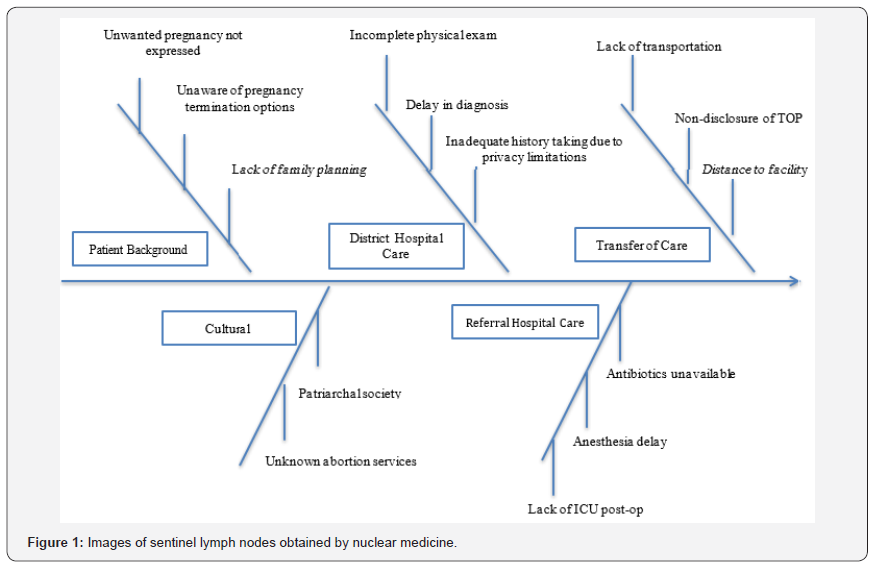
The cultural issue of male dominance in the Ghanaian society
further widens the gap in equitable access to care [10,11].
Preventive processes that have been identified and implemented
include developing a feedback system, improving access to and
awareness of family planning services, and improve awareness of
Ghana’s abortion laws to health providers. Long-term projects that
involve government policy and major funding include increasing
the education of girls, and the empowerment of women politically
and economically. Also required are health care resources such as
ICU, availability of antibiotics and skilled health care providers.
Obstructed labor, Mbarara, Uganda
A 28-year-old primigravid HIV positive Rwandese refuge
was admitted following referral by a primary health facility for
obstructed labor with fetal death at 39 weeks of gestation. She was
not on antiretroviral medications and had an unknown CD4 count
and viral load. She had labored for three days at home. She started
pushing at home under the care of a traditional birth attendant
who sent her to the primary health facility because the baby had
“failed to come.” Subsequently, the primary health facility referred
her to the regional hospital, which was 40 kilometers away, at
which exploratory laparotomy revealed a lower segment uterine
rupture, massive hemo-pyo-peritonium with the placenta in the
abdominal cavity and extensive necrosis of the lower uterine
segment and pelvic fascia. A macerated male stillbirth of 3.9
kilograms was delivered and total hysterectomy with bilateral
internal iliac artery ligation done within 85 minutes of arrival. Four
units of whole blood were transfused during the operation. The
patient remained hypovolemic with tachycardia and poor tissue
perfusion post operatively. She developed signs of pulmonary
edema, had convulsions; deteriorated and expired on the fourth
day of management. Cause of death was cardiopulmonary failure
and septicemia resulting from ruptured uterus following neglected
obstructed labor in the community. No autopsy was done.
Obstructed labor Fishbone and Root Cause Analysis: Figure
2 shows the fish bone diagram that highlights the root causes of this
mortality. There was delay in making the decision to seek medical
care, since the patient labored at home for more than 3 days. There
was a crucial delay in reaching the appropriate facility because
the initial health center was not equipped for critical obstetrical
procedures and she had to be transported 40 kilometers to the
tertiary center. There was also a delay in receiving appropriate
management on arrival at tertiary center. A program implemented
in this institution is a maternal death confidential inquiry audit
which involves tracing all the way back to the deceased’s home
and holding discussions with all concerned.
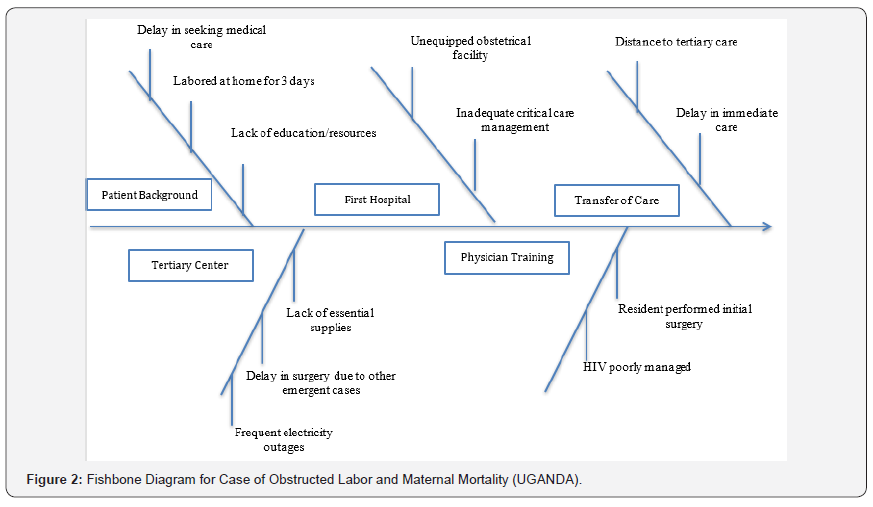
Discussions are arranged with the health workers directly
involved in the management of the deceased mother, immediate
family members, and community leaders. The final audit and review
is utilized to recommend, advocate and implement programs
to reduce maternal mortality. This institution in collaboration
with counterparts from high resource institutions has initiated
achievable quality improvement projects as requirements for the
OBYN residents as a method to target systems deficits in care.
Peripartum hemorrhage, madurai, india
A multiparous 33-year-old, at 40 weeks of gestation with
uneventful antenatal course was admitted at a primary facility
in spontaneous labor and progressed well. She had a second
stage of approximately ninety minutes complicated by maternal
exhaustion and fetal bradycardia. Outlet forceps were applied
and a healthy female baby weighing 3.4kg was delivered. The
episiotomy wound was sutured, and the cervix and vagina explored
and found to be intact. There was no postpartum hemorrhage,
and she was transferred to the post-partum unit. Approximately
two-and-a-half hours later, patient was found unconscious by her
attendant and could not be aroused. Patient was resuscitated and
subsequently was referred to a tertiary care center for further
management. She was received 1-hour later in the Casualty unit of a regional
hospital because transporting taxi-driver felt that the patient was
deteriorating and would not make it to the designated tertiary
center. Her pulse was feeble, blood pressure un-recordable,
and patient was gasping. She was resuscitated with parenteral
fluids and intubated. On abdominal examination, uterus was 24
weeks size and pushed towards the right side by a boggy mass
extending from the bladder on the left side, halfway to the level of
the umbilicus. Vaginal exam revealed normal cervix and minimal
vaginal bleeding with fullness felt in the left fornix.
Ultrasound showed a suspected left side pelvic hematoma
close to the uterus with a possible ruptured uterus. Laboratory
results revealed bleeding coagulopathy with anemia, and
she was appropriately transfused with fresh frozen plasma
and packed red blood cells. Patient was taken for exploratory
laparotomy approximately one hour after arrival. Intraoperative
findings revealed a left broad ligament and a rupture of the left
lateral uterine wall. Total abdominal hysterectomy left salpingooophorectomy
and bilateral internal iliac artery ligation was
performed. Postoperatively, patient was transferred to ICU.
Packed cells, fresh frozen plasma and platelet transfusions were
continued. While the altered coagulation profile was corrected, the
hypotension persisted. Neurological evaluation revealed global
cerebral damage. Patient developed repeated episodes of cardiac
arrest and finally could not be revived. She expired approximately
24 hours after delivery.
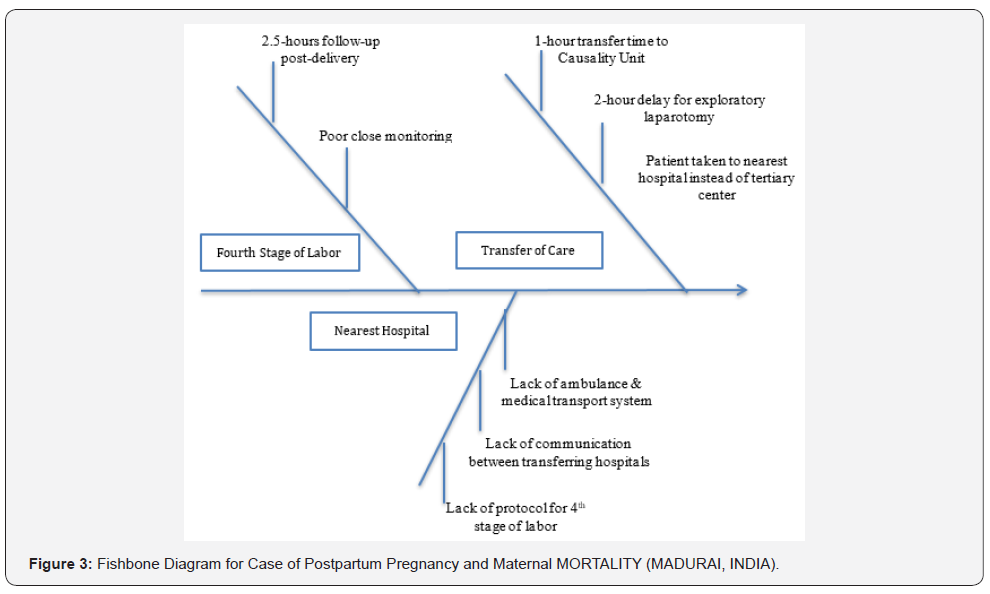
Peripartum hemorrhage fishbone and root cause analysis:
A fish bone diagram Figure 3 highlights the problems identified
during the discussion that are considered potential root causes
of the maternal mortality. In this postpartum hemorrhage case,
there was no obvious external blood loss to alert the healthcare
providers instead a significant volume of blood loss occurred
intra-abdominally, leading to hemorrhagic shock and subsequent disseminated intravascular coagulation. There was inadequate
monitoring of the fourth stage of labor. It is likely that if the
pelvic hematoma was recognized earlier and appropriate surgical
treatment was done immediately, the patient’s life may have been
saved. During transport to a higher referral center, there was
a delay in reaching an appropriate facility, since a taxicab was
transporting the patient to a tertiary center, when she became
“moribund” and she was taken to a nearest hospital.
Preeclampsia, haiti
A 37-year-old, primigravida at 39 weeks of gestation was
referred because of new onset hypertension treated with
methyldopa. Blood pressure was 170/120. Ultrasound showed
a fetus, in cephalic presentation with estimated fetal weight less
than the 10th percentile, normal amniotic fluid, umbilical artery
Doppler with no end diastolic flow and the placenta had multiple
lacuna. Platelets, renal function tests and liver function tests were
not done because of a lack of reagents. A diagnosis of preeclampsia,
intrauterine growth restriction and suspected placenta abruption
was made. Blood pressure was controlled and stabilized with
intravenous Apresoline. An uncomplicated cesarean section was
performed because of the suspected abruption. She delivered
a healthy female baby, birth weight 2580 grams with a normal
placenta noted. Postpartum; her blood pressures stabilized to
140-130/80. She was asymptomatic with no complaints; renal
and liver function tests were not done. On postpartum day 2, her
blood pressure was 140/80, with normal clinical evaluation. She
was discharged home on Methyldopa.
She presented to the Emergency Room the next day
(postpartum day 3) with respiratory distress, epigastric pain,
cough productive of whitish sputum, blood pressure of 220/120
and crackles on both lungs. The differential diagnoses entertained
were pulmonary edema, pulmonary embolism and hepatic
rupture. She was treated with Magnesium sulfate and Apresoline
but died during resuscitation. An autopsy was not performed.
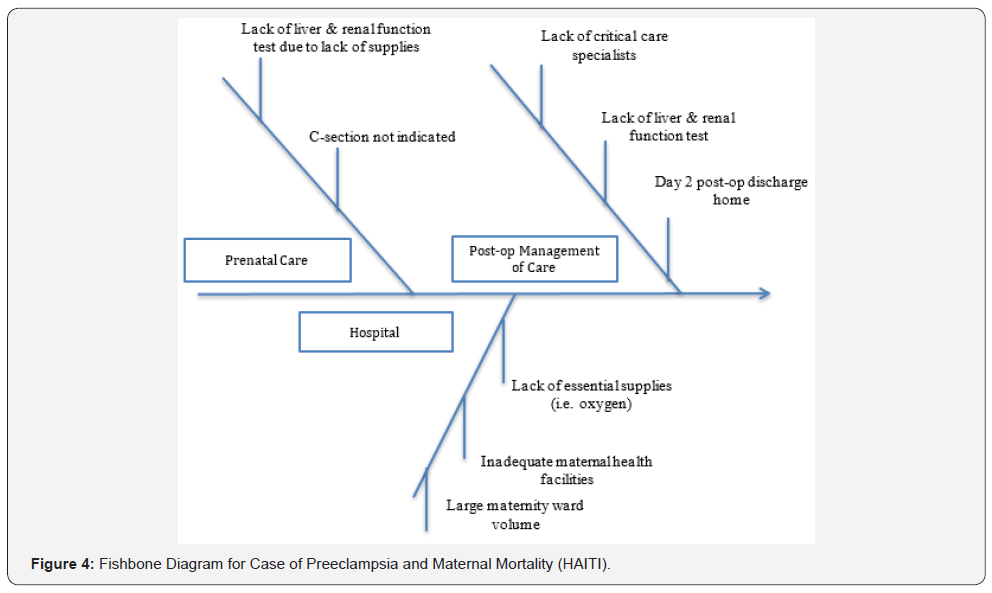
Preeclampsia fishbone and root cause analysis: A fish
bone diagram Figure 4 highlights the problems identified during
the discussion that are considered potential root causes of this
mortality. This case highlights the contribution of inadequate
management on arrival at a health facility to maternal mortality.
The only indication for cesarean delivery was the ultrasonic
abruption diagnosis. In this institution, patients with cesarean
section are discharged on the 3rd post-operative day but because
of high patient load and inadequate maternal care facilities,
this patient was discharge home on the 2nd post-operative day.
Liver and renal function tests that might have demonstrated
severe preeclampsia were not performed prior to discharge. RCA
highlighted lack of resources such as critical care specialists;
oxygen in the emergency room and laboratory test reagents.
Discussion
We have used four illustrative examples of maternal mortality
to make specific points about obstetrical care in different
international settings noting that these cases do not portend to
describe all the common problems at each site or country. The
death from unsafe abortion emphasizes the fact that despite
Ghana’s liberal abortion law, illicit abortion continues because
of lack of public education, and inadequate resources [11].
The death from obstructed labor from Uganda highlights the
pivotal role of traditional birth attendants and inadequate
transportation infrastructure [12]. The case of unapparent postpartum
hemorrhage from India; granted that this case may be
challenging in any high resource country nevertheless emphasizes
the importance of the fourth stage of labor and the need for close
monitoring of the immediate postpartum period. The maternal
mortality from severe preeclampsia from Haiti emphasizes
inadequate maternity health care facilities and lack of ancillary
resources.
Many of the drivers of maternal mortality such as
transportation, facilities, drugs, equipment, skilled health care
workers and cultural taboos are daunting and overwhelming in
scope and enormity. Successful interventions would require major
political will, policy changes, health-care infrastructure, largescale
funding and fundamental cultural changes [13]. Therefore
even though reviewing these maternal mortality cases may seem
to be “hand-wringing”, however our goal was to report feasible
projects that can be undertaken by individual or small groups
of obstetricians, MFM specialists or professional organization
committees in collaboration with physicians in low-resource
communities with the aim to reduce global maternal mortality.
The cases presented were based on professional mentoring
relationships developed over time with specific physician leaders
in the four countries. The MFM specialists were able to provide
training, promote the use of RCA, help categorize risk factors
associated with maternal mortality, and act as a resource. Most
importantly, the low resource physician leaders with support
from the MFM specialists were able to implement feasible and
achievable improvement projects derived from the systematic
maternal mortality review aimed at reducing maternal mortality
in their local environment. For example, the site in Ghana worked
on system to provide feedback to referring health centers, the care
team and the administrative staff. The Uganda site developed an
emergency cupboard for cesarean delivery supplies as a result
of the mortality, the site in India reviewed the process of close
monitoring of the 4th stage of labor and the Haiti site ensured that
wall oxygen was available in the maternity unit. Our experience can
be used to make some suggestions for international collaboration
to reduce maternal mortality as follows:
1) The first step requires that the physicians in high
resource communities interested in global health and maternal
mortality expand their knowledge on all aspects of maternal
mortality including global scope, systematic maternal
mortality reviews, root cause analysis process including fish
bone diagram analysis, standard protocols to obstetrical
emergencies, quality improvement projects implementation
and current initiatives. Maternal mortality is a complex
problem involving complex system problems; the motivated
physician may need to learn the LEAN or Kaizen principles.
The term ‘lean thinking or Kaizen principles’ is based on the
production philosophy, which evolved at Toyota to understand
processes in order to identify and analyze problems. Lean
thinking has been applied successfully in a wide variety of
healthcare settings. The four general components of lean
thinking in use are:
a. methods to understand processes in order to
identify and analyze problems
b. methods to organize more effective and/or
efficient processes
c. methods to improve error detection, relay information
to problem solvers, and prevent errors from causing harm
d. methods to manage change and solve problems
with a scientific approach [13].
2) The trained physicians can then identify a physician
leader in a low resource country to develop a professional
and cooperative relationship. Identifying a compatible global
physician partner can be challenging, and one may have to
access experienced global health researchers, institutional
and national programs.
3) Exchange visits are crucial to implementing a global
health initiative. Ideally this should be bilateral. The high
resource physician visits the low resource institution to get
a scope of the local culture and challenges and thus be in a
position to help train, guide and support maternal mortality
reviews and initiatives. It is also important that the global
health counterpart visit the high resource institution to learn,
experience and be motivated.
4) Professional organizations in high resource countries
should be encouraged to hold more global sessions to which
emerging leaders are invited and sponsored. This will greatly
increase motivation, mentoring and training of low resource
physicians; increase collaborations and the sustainability of
programs.
5) Constant and sustainable communication is the key to
successful global collaboration especially between visits. In
our programs we have used some form of telecommunication
to have a regular conference at regular intervals. Ideally audiovisual
telecommunications such as SKYPE, WEBEX are best,
but because of limited Internet capacities in some countries
we have had to depend on an audio only platform, which are
more stable. The high-resource may need to be on a “on-call”
schedule for access by phone or email in the advent of unusual
or catastrophic obstetrical emergencies in the low resource
country.
6) Finally, we believe that the collaboration should result in
the identification and implementation of “specific, quantifiable
and finite” quality improvement projects that can promote safe
care and reduce maternal morbidity and mortality in the local
region. Evidence shows the more specific the intervention as
compared to broad interventions, the stronger the evidence
that the intervention can help reduce maternal mortality [14].
In conclusion, we have shown that a group of MFM experts
interested in global health, can develop mentoring and professional
relationships with global counterparts that can facilitate systemic
reviews of maternal mortality, lead to an awareness of risk factors
and the implementation of preventive programs that can reduce
maternal morbidity and mortality. We believe that it is possible to
develop a group of specialists with a maternal health focus who
can support local capacity building to facilitate local maternal
mortality reviews and the implementation of appropriate
prevention program.




I like the content which was mentioned above. If any of the final year students are looking for the image processing final year projects
ReplyDelete