Gastroenterology & Hepatology - Juniper Publishers
Abstract
Background: Celiac disease (CD), is a chronic
immune-mediated disorder of small intestine that occurs in genetically
predisposed populations due to permanent intolerance to wheat gliadins
and other cereal prolamins. The epidemiology of CD has iceberg
characteristics with more undiagnosed cases. The diagnosis of CD is
currently based on both typical small bowel biopsy findings with
clinical and serological parameters.
Aims: The aim of study was to determine compliance regarding gluten restricted diet in confirmed cases of celiac disease.
Materials and Methods: Two hundred and
twenty-five confirmed cases of celiac disease on basis of clinical
history, physical examination, raised serum IgAttg level and duodenal
biopsies were followed regularly in celiac clinic and telephonically for
one year and then compliance rate regarding strict gluten in diet was
calculated.
Results and Conclusions: The compliance rate
regarding strict gluten restricted diet was Ninety (89.77%). It was more
in females and in older age group in comparison to males and younger
age group
Keywords:
Celiac disease; Duodenal biopsy; Gluten; Compliance; Small intestine;
Transglutaminase; Endomysium; Wheat; Rye; Oat; Barley; Proline content;
Clinical gastrointestinal; Intraepithelial lymphocytes; Crypt
hyperplasia
Abbrevations: CD: Celiac Disease; GI: Gastrointestinal; IHC: Immunohistochemical; IELs: Intraepithelial Lymphocytes
Introduction
Celiac disease (CD) is a chronic immune-mediated
disorder of small intestine that occurs in genetically predisposed
populations [1]. The pathogenesis entails a T cell mediated immune
response with production of auto antibodies directed against tissue
transglutaminase or endomysium. Wheat, rye, oat and barley prolamins are
toxic for celiac patients due to their high glutamine and proline
content [2]. Initially the suspicion of CD was based on clinical
gastrointestinal (GI) symptoms. Subsequently, the disease has been found
with variety of atypical symptoms and even in asymptomatic subjects
[3]. Celiac disease affects people in all parts of the world. The
histologic changes in CD vary from severe villous atrophy to more subtle
changes (with or without increased density of intraepithelial
lymphocytes and crypt hyperplasia). Although villous atrophy is not
specific to CD. Serology has become increasingly relevant to CD
diagnosis. Anti-tissue transglutaminase antibodies are the most
sensitive test for CD [2].
Materials and Methods
Two hundred and twenty-five confirmed cases of celiac
disease on basis of clinical history, physical examination, raised
serum IgAttg level and duodenal biopsies were followed regularly in
celiac clinic and telephonically also for one year and then compliance
rate regarding strict gluten restriction in diet was calculated. The
biopsy was taken from second part of duodenum through
eosophagoduodenoscopy with the assessment of duodenal endoscopic markers
including scalloping of folds, grooving, and nodularity of mucosa.
Histopathological diagnosis was established on routine hematoxylin and
eosin stained sections [4]. Immunohistochemical (IHC) staining [5] with
antihuman CD3 antibody was done for evaluating intraepithelial
lymphocytes (IELs) with positive (tonsillar tissue) and negative
(substituting the primary antibody with an antibody of irrelevant
specificity) controls. The histopathological grading was performed as
per modified Marsh grading [6].
Disscussion
Celiac Disease is also known as intestinal infantilism, idiopathic
steatorrhea, non-tropical sprue, and gluten sensitive enteropathy.
Various etiological factors are considered for CD including
genetic (HLA class II antigen) and environmental risk factors
[7] including GI infections [8]. Gliadin is a glycoprotein extract
from gluten, directly toxic to the enterocytes of individuals with
CD. Transglutaminase enzyme crosslinks gliadin and causes
specific deamination of glutamine into glutamic acid. With such
deamination, the gliadin peptides are able to be more efficiently
presented to gliadin-reactive CD-4 T cells.
Without Transglutaminase, it is believed that gliadin is less
immunogenic. Thus, Transglutaminase auto antibodies play
a role in disease pathogenesis, but lacks sufficient supportive
evidence [9]. The epidemiology of CD has iceberg characteristics
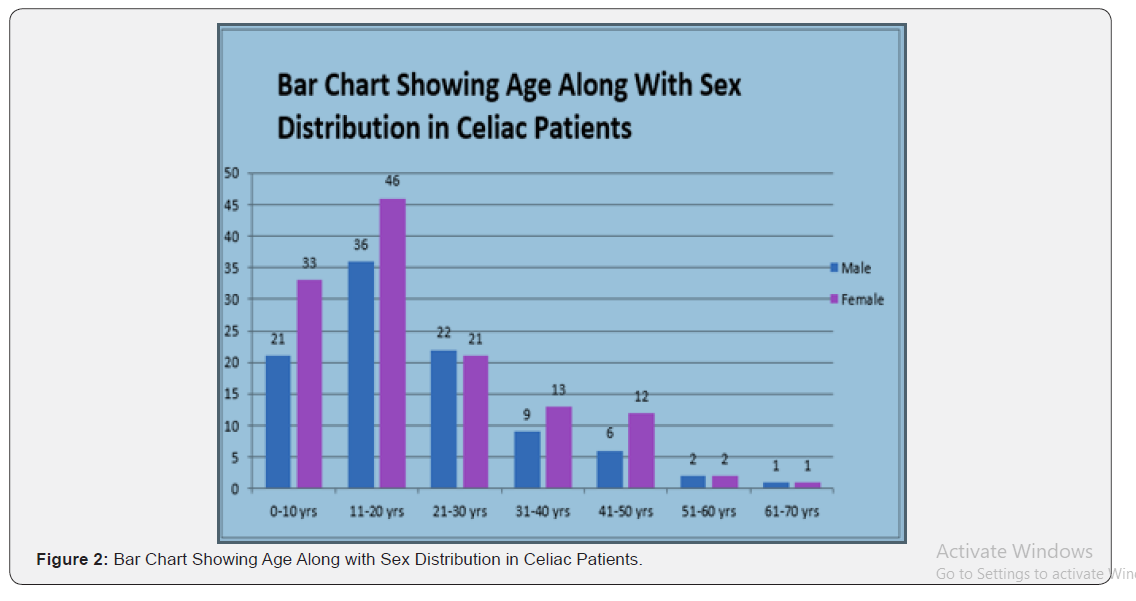
as there are more undiagnosed cases. The female-to male ratio
is 2:1. The prevalence of CD is globally 1%. The prevalence of
CD in India is nearly the same as that in Western Caucasian
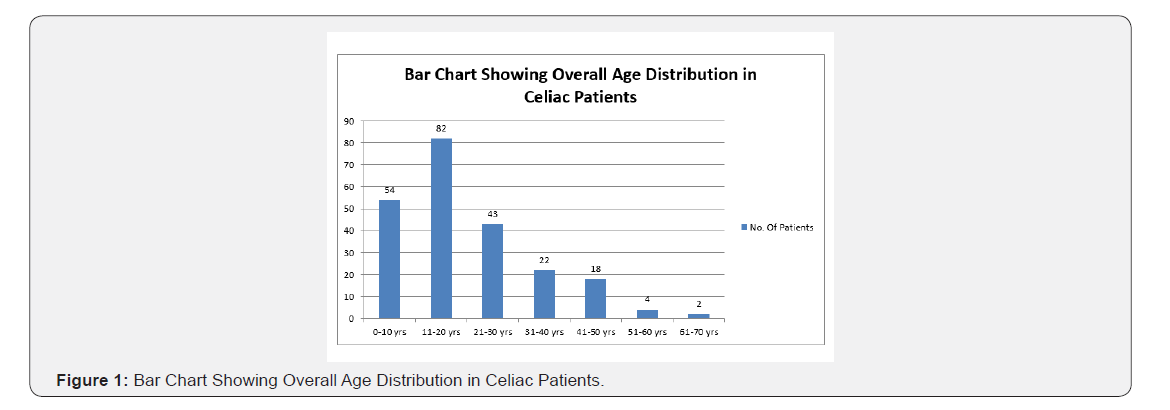
populations [10]. Adult celiac were more than children in our
study. In both groups, females were predominant. Maximum
number of patients presented with GI symptoms than atypical
symptoms in which diarrhea was the most common complaint
as seen in other studies in literature [11-16].
In our study we found compliance rate to be 89.77% i.e. in
202 patients in total group of 225 patients, in comparison to
JC Chauhan et al, [17] who reported compliance rate of 75%.
They found decreased dietary compliance during 10-17 yr of
age (44%, compared to>80% in <9yr age group) but in contrast
in our study we found compliance to be more in adults then
younger age group. Ljungman et al, [18] reported compliance
rates of 93% at 12 years of age decreasing to 76% in 15-17
yrs age group. In the present study, non-compliance was more
common in female patients i.e., 60%. Higher dietary noncompliance
in female patients may be explained by socio-cultural
factors, family pressure and gender bias. Results of study by
Anson et al, [19] also show that maternal education is important
factor affecting compliance, which may be because mother is responsible for preparation of food items and providing GFD and
same fact was found to be totally correct in our study group also.
In our study we concluded that non-compliance was higher in
Joint families and with more numbers of siblings. When dietary
compliant and dietary non-compliant patients were compared,
it was found 90% of dietary compliant patients presented with
typical symptoms and 10% presented with atypical symptoms
because patients presenting with typical symptoms had visible
improvement in their symptoms. Fabiani et al. [20] also reported
higher compliance in symptomatic patients as compared to
asymptomatic screen detected patients. Parents of the dietary
compliant groups had better understanding of Celiac disease
than those of non-compliant group. Butterworth et al have
reported lower compliance in south Asian migrants to UK, who
were less satisfied with the explanation by the physician [21].
In our study higher compliance rate can be attributed to
greater effort on counseling of patients and family members and
highlighting repeatedly the importance of gluten restricted diet
on follow up and even telephonically also. Anson et al [19] study
also showed similar correlation of parental knowledge and
dietary compliance [1]. Thus, results of present study show that
compliance is higher when parents have better knowledge about
celiac disease, understand value of gluten free diet and are able
to handle the menu better. These results highlight importance
of proper counseling and reinforcement during subsequent
visits. Difficulty in maintaining dietary compliance at school and
at family party/marriage, was higher in dietary non-compliant
group compared to the dietary compliant. Gluten containing food
as main dietary item, served at above places, was a problem for
both dietary compliant and non-compliant group. Present study
findings show that dietary non-compliance is more common
when preparing gluten free food items is considered a financial
burden. Similar finding also has been reported from Anson et al
[19]. As more and more patients are being diagnosed from lower
socio-economic status, counseling regarding cheap food items
and easily prepared GF food items will probably help this group
(Figure 1 & 2).
Conclusion
The first and foremost important point in celiac
disease is to
make patient and family members understand the importance
of life-long restriction of gluten in diet. For this onus lies on
shoulders of treating Gastroenterologist/Physician which
requires proper counseling at initial diagnosis and on regular
follow up of patients. This will lead to increasing compliance
in celiac patients in whom the only treatment available at this
point is gluten restriction in diet. For increasing the compliance
among patients, there is also requirement of training of medical
professionals and alternative medicine practitioners, for not
restarting gluten in diet under cover of steroids because they
temporarily mask the development of symptoms due to re-entry
of gluten in body but damage of gluten on intestine goes unabated
and even side effects of immunosuppressant’s like hypertension,
diabetes mellitus, osteoporosis etc. develop. Other important
issue for increasing compliance is to recognize hidden source
of gluten being taken in the diet, of which patient is unaware,
thus there is unsatisfactory clinical, biochemical and histological
recovery. The reasons for it are adulteration of gluten in diet due
to common kitchen practices for preparing food for whole of family,
using same utensils or consumption of market products thinking to be
gluten free but in reality containing minute
amounts of gluten in diet and even frequent and heavy use of lip-stick,
as it contains gluten as a base . In school going children, the reason
came out to be sharing of food with other children.
To know more about Gastroenterology & Hepatology
Click here: https://juniperpublishers.com/argh/index.php
To know more about Juniper Publishers
Click here: https://juniperpublishers.com/index.php




No comments:
Post a Comment