Open Access Journal of Surgery
Purpose: Laparoscopic cyst excision and
Roux-en-Y hepaticojejunostomy is gaining popularity as a treatment for
choledochal cyst in children. The aim of this study is to determine the
feasible and safe of the laparoscopic excision with Roux-en-Y
hepaticojejunostomy and evaluate the short-term outcomes after treatment
for children with choledochal cyst.
Methods: A prospectively of 51 consecutive
pediatric patients undergoing laparoscopic choledochal cyst excision and
Roux-en-Y hepaticojejunostomy performed by one surgeon cysts at Hue
Central Hospital from June 2012 to December 2017 was studied.
Results: The mean operative time was
214.7±67.95 minutes (range, 100~360 minutes), including the time for
intraoperative cholangiography. There were two children requiring blood
transfusion. Time to first flatus was 40.35 ± 28.55 hours in average.
The mean time to drain removal was 2.89±1.02 days. Mean postoperative
hospital stay was 9.31 ± 3.43 days. 6/51 cases having early
complications, including 2 cases of pancreatitis and 4 cases of bile
leakage. Most of cases (90.5%) were classified as good after 10 days to 3
months of follow-up.
Conclusion: Laparoscopic choledochal cyst
excision and Roux-en-Y hepaticojejunostomy was feasible and safe in
children. The short-term outcomes were good in most cases.
Keywords: Laparoscopic excision, Roux-en-Y hepaticojejunostomy, choledochal cyst, children.
Introduction
Choledochal cysts are a rare congenital cystic
dilation of the biliary tract, first described by Vater and Ezler in
1723. They present primarily in female infants and young children and
are more prevalent in East Asian populations. although benign,
choledochal cysts can be associated with serious complications including
malignant transformation, cholangitis, pancreatitis, and cholelithiasis
[1,2]. Hence, complete surgical excision of the choledochal cyst and
enterobiliary reconstruction has been recommended as the standard
treatment.
Choledochal cyst excision and biliary enteric
reconstruction constitute the best therapy for choledochal cyst [3].
Comparing with open procedure, laparoscopic procedure has been proven to
have shorter hospital stay and lower morbidity of anastomotic stenosis,
bile leakage, intrahepatic stone formation, cholangitis,
pancreatic leak, intestinal obstruction, and re-operation [4,5]. Thus,
as a safe, efficacious, and minimally invasive procedure, laparoscopic
cyst excision and Roux-en-Y hepaticojejunostomy has become a common
procedure for pediatric choledochal cyst in many medical centers [6].
With increased familiarity with the laparoscopic anatomy of the biliary
tract and advances in minimally invasive techniques, surgeons have
ventured further to operate on technically difficult cases such as
choledochal cyst that were until recently managed by laparotomy [7]. Our
preliminary result shows that laparoscopic excision of choledochal cyst
and Roux-en-Y hepaticojejunostomy is effectiveness in pediatric
patients [8]. The purpose of this study was to determine the feasible
and safe of the laparoscopic excision with Roux-en-Y hepaticojejunostomy
and evaluate the short-term outcomes after treatment for children with
choledochal cyst.
Methods
Patients
A prospective study involving 51 pediatric patients diagnosed
with choledochal cysts at Hue Central Hospital from June
2012 to December 2017. All patients underwent laparoscopic
choledochal cyst excision and Roux-en-Y hepaticojejunostomy.
all procedures were performed by the same surgery team. This
study was approved by the ethics committee review board of
our hospital. The variables investigated were demographic
information of all patients, operative details and outcomes
such as operation time, intraoperative blood transfusion,
postoperative time to first flatus and postoperative hospital stay,
and postoperative complications.
Operative Technique
The procedure of laparoscopic choledochal cyst excision is
summarized below:
i. Under general anesthesia, the patient was intubated
and placed in reverse Trendelenburg position.
ii. Four-site procedure was used as the trocars were
located at middle of the umbilicus, right hypochondrium,
right side of the abdomen, and left hypochondrium,
respectively.
iii. A monopolar electrocautery hook was used to dissect
the choledochal cyst and the gallbladder. The cyst was
dissected down to the distal tapered end of the common
bile duct, and it was then ligated. The upper part of the cyst
was further dissected up to the common hepatic duct and
then removed at this level. When severe adhesion around
the cyst was encountered, bipolar coagulation was used for
dissecting.
iv. A Roux-en-Y anastomosis was constructed by
exteriorization of the small bowel via the enlarged umbilical
trocar port. a retrocolic end-to-side hepaticojejunostomy
was carried out laparoscopically. To minimize the biliary
contamination of peritoneum, our procedure was modified
later in the series by completing the jejunojejunostomy
before the cyst excision.
v. Draining tube was indicated only in selected cases.
vi. When common hepatic duct stenosis was encountered
in the Todani-IV a type cases, the stenosis was resected
or a ductoplasty was performed by a longitudinal
incision on the anterior wall and followed by additional
cholangioenterostomy.
Postoperative Management and Follow-up of Patients
Patients usually started a liquid diet on postoperative
day 1. Jackson-Pratt drains were removed if ultrasound that
were performed on postoperative day 4 showed no evidence
of abnormal fluid collection. Patients revisited the outpatient
department 2 weeks after discharge and were followed up at 3
months to monitor postoperative complications. For follow-up, a
routine complete blood count, liver function test, and ultrasound
or CT were performed to evaluate complications, such as
pancreatitis, cholangitis, choledocholithiasis, or malignancy.
Clinical outcome was determined according to the
Terblanche classification [9] grade I, no biliary symptoms;
grade II, transitory symptoms and no current symptoms; grade
III, biliary symptoms requiring medical therapy; and grade IV,
recurrent biliary symptoms requiring correction or related to
death. Terblanche class IV constituted a poor result. Terblanche
I, II, and III constituted a clinical success with excellent, good,
and fair results, respectively.
Data Analysis
For a descriptive analysis, the frequency or the mean and
standard deviation were calculated for each variable. For other
continuous variables, independent sample t-tests were applied
to compare the data from the children and adult groups. Their
respective p-values and corresponding confidence intervals
were provided by SPSS Version 18.0 (SPSS Inc., Chicago, Illinois,
USA). The statistical significance was set at p<0.05.
Results
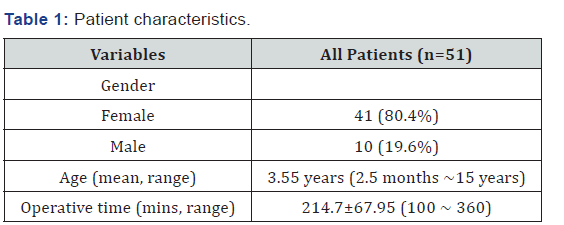
Forty-one patients were females and 10 were males. The
mean age at the time of surgery was 3.55 years (range, 2.5
months~15 years). The mean operative time was 214.7±67.95 minutes (range, 100~360 minutes), including the time for
intraoperative cholangiography. The patient characteristics and
the operative features were seen in Table 1.
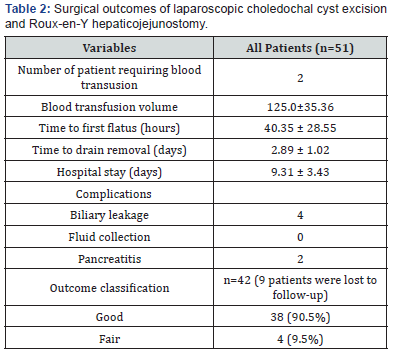
Table 2 shows the surgical outcomes of laparoscopic
choledochal cyst excision and Roux-en-Y hepaticojejunostomy.
There were two children requiring blood transfusion with the
total volume of packed red blood cells of 125.0±35.36 ml. Time
to first flatus was 40.35 ± 28.55 hours in average. The mean
time to drain removal was 2.89±1.02 days. Mean postoperative
hospital stay was 9.31 ± 3.43 days. 6/51 cases having early
complications, including 2 cases of pancreatitis and 4 cases of
bile leakage. Conservative treatment was initially implemented
which resulted in complete resolution in 5 cases. Re operative
was finally required in 1 case with persistent bile leakage. Most
of cases were classified as good after 10 days to 3 months of
follow-up.
Discussion
Choledochal cyst is a rare congenital anomaly of the biliary
system that commonly affects the Asian population [10].
The estimated incidence of choledochal cyst and anomalous
pancreatobiliary ductal union is 0.3% and 4.1%, respectively,
according to a large, multicenter study [11]. The clinical
presentation of choledochal cyst differs from children to
adults. In adults, this disease entity can manifest cholangitis,
pancreatitis, choledocholithiasis, or biliary malignancy, such
as cholangiocarcinoma or gallbladder cancer [11]. Complete
excision of the cyst is mandatory because of the risk of developing
complications or malignancies.
With growing interest in cosmetics, laparoscopic approaches
in hepatobiliary surgery have become inevitable. Laparoscopic
hepaticojejunostomy anastomosis still remains one of the most
sophisticated and challenging surgeries to date [12]. Since the
first report of laparoscopic choledochal cyst excision in 1995 [13]
studies regarding this approach have reported that laparoscopic
surgery is safe and feasible in the treatment of choledochal cysts.
Choledochal cyst is characterized by its remarkably higher
incidence in the female patients together with the regional
preference. In this study also, we found more cases of female
patients, the female/male ratio in our study was 4.0/1. This was
similar to other studies. Sheng Q (2017) showed a female/male
ratio of 15/3 = 5. [14]. In the study of Liu Y et al. [5], the female/
male ratio was 29/6 = 4.83.5 Since choledochal cyst is more
common in female, the aesthetic advantages of laparoscopic
procedure are more relevant. Patient’s age ranged from 2.5
months to 15 years (Table 1). The mean age was 3.55 years. The
results of our study were similar to other studies. Huang CS et al.
[15] reported 101 cases of choledochal cysts in which 42 cases
were children (41.6%) and 59 cases were adults (58.4%). The
mean age was 8.9 years 3.7 years for children [15].
Operative time ranged from 100 to 320 mins. Mean operative
time was 214.7±67.95 mins. Minimizing operative time and
maintaining outcomes at the same time has always been a
challenge to surgeons, especially in young children and infants.
If surgery is too lengthy, comorbidity rate will increase. To
shorten operative time, multiple factors are required including
competent skills of surgeon, assistants and nurses, close
coordination with anesthesiologists and adapted instruments.
Therefore, operative time in the beginning of the learning
curve of laparoscopic procedure is longer. Operative time of
laparoscopic procedure was also longer compared to open
procedure in recent studies. Our operative time was comparable
to the study of Liem NT (2012) with 400 patients, the operative
time in hepatoduodenal anastomosis group was 164.8 mins,
and in hepatojejunal anastomosis group was 220 mins [16].
According to Liu Y et al. [5], mean operative time of laparoscopic
procedure was 249 mins, longer than open procedure with mean
operative time of 132 mins [5].
One of the complications of laparoscopic choledochal cyst
excision is bleeding requiring intraoperative blood transfusion.
Liem NT (2012) reported four cases with bleeding requiring
intraoperative blood transfusion, three cases with transection
of both hepatic ducts and one case with right hepatic duct
perforation [16]. Tang ST et al. [17] noted 8 cases requiring
intraoperative blood transfusion.
Regarding the early postoperative complications, we
noted 6/51 cases having early complications, including 2
cases of pancreatitis and 4 cases of bile leakage. Conservative
treatment was initially implemented which resulted in complete
resolution in 5 cases. Re operative was finally required in 1
case with persistent bile leakage. Re operative was finally
required in 1 case with persistent bile leakage. Ono et al. [18]
reported liver dysfunction, dilatation of intrahepatic bile ducts,
recurrent abdominal pain, and biliary tract malignancy as
long-term complications after choledochal cyst excision and
hepaticojejunostomy. The laparoscopic approach can magnify
the operative view, which may assist in dissecting the whole
choledochal cyst without a remnant duct, and in anastomosis.
Liuming H (2011) reported 1 case of postoperative bile leakage
in a study of 39 patients [19]. In a study of acker SN (2013),
the rate of bile leakage was 1.6%. Pancreatitis was a relatively
rare postoperative complication after choledochal cyst excision.
Preoperative pancreatitis might be an important risk factor
predisposing the patient to postoperative pancreatitis [20].
Compared to other studies, the rates of early complications of
our study was low.
Several tips were suggested by some authors to reduce the
rate of bile leakage. Firstly, electrical dissection should not be
overused and over-dissecting the anterior wall of common
hepatic duct should also be avoided. Secondly, good laparoscopic
suture technique should be practiced. Thirdly, bowel loop with
good arterial arcade with sufficient length should be chosen to
construct a tension free anastomosis. Finally, the anastomosis
should be carefully checked before the end of the operation.
Other reported complication including incisional fluid collection,
pancreatic fistulas and early adhesive intestinal obstruction was
not noted in our study.
Our study contains some limitations. Firstly, the sample
size was small, and the follow-up period was short (within 3
months). Secondly, there was no control group to compare such
as open surgery to see the efficiency of laparoscopic choledochal
cyst excision and Roux-en-Y hepaticojejunostomy in children.
Conclusion
Laparoscopic choledochal cyst excision and Roux-en-Y
hepaticojejunostomy was feasible and safe in children. It
could significantly improve in terms of operative time, overall
postoperative complication rate, and the length of hospital stay.
The short-term outcomes were good in most cases.
To Know More About Open Access Journal of Surgery Please click on:https://juniperpublishers.com/oajs/index.php




Excellent and helpful post… I am so glad to left comment on this. This has been a so interesting read, would love to read more here….IVF Centre in Bangalore | Vaginal Hysterectomy Surgery in Bangalore | Gynaecology Hospitals in Bangalore | Maternity in RRnagar |
ReplyDelete