Open Access Journal of Neurology & Neurosurgery
Massive supratentorial infarct due to large vessel occlusion results death which can be prevented by early decompressive craniectomy rather than delayed. This is a short review of those clues to decide which cases will need early surgery.
Abbrevations: MCA: Middle Cerebral Artery; ICA: Internal Carotid; ICP: Intracranial Pressure
Introduction
Massive brain swelling may occur in 10% of cerebral ischemic strokes. In these patients the clinical presentation usually starts with focal signs (motor weakness, speech disturbances, and hemianopsia) and progresses with a decline of consciousness (drowsiness, stupor). Despite optimal medical management this condition may lead to death in 70-80% of cases Because of the grim prognosis, this condition has been termed “malignant” cerebral infarction. The etiology is the occlusion of a large vessel, primarily the Internal Carotid (ICA) or the Middle Cerebral Artery (MCA).
Decompressive surgery seems to be more effective if performed earlier rather than later. That is why, there is great interest in identifying clinical, laboratory, and imaging findings which is able to predict which patients are going to develop a malignant infarction.
Clues to detect ischemic patients at higher risk for a malignant supratentorial (MCA) infarction who will require surgery [1].
Clinical
Signs of raised intracranial pressure specifically progressive deterioration of consciousness. But, decrease in consciousness level may be due to shift of the ischemic tissue rather than raised Intracranial Pressure (ICP). So, clinical data must be correlated with Imaging findings.
Radiological
CT scan/perfusion-CT
a. Area compromised > 50% MCA territory
b. Perfusion drop > 66% an infarct extending also to the anterior or posterior cerebral artery territories.
c. A midline shift >10 mm, effacement of subarachnoid spaces, and attenuation of corticomedullary differentiation are also related to higher risk of severe deterioration.
MRI/DWI
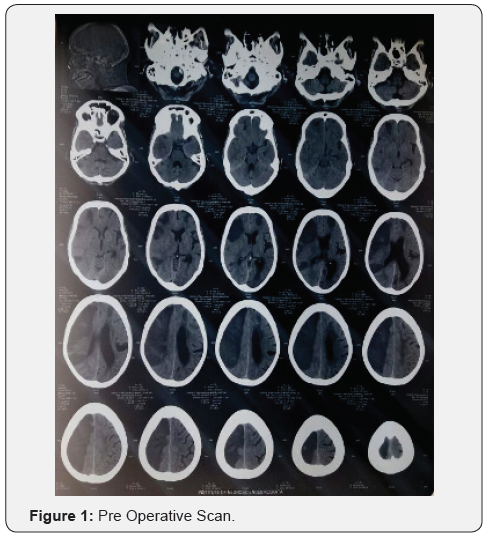
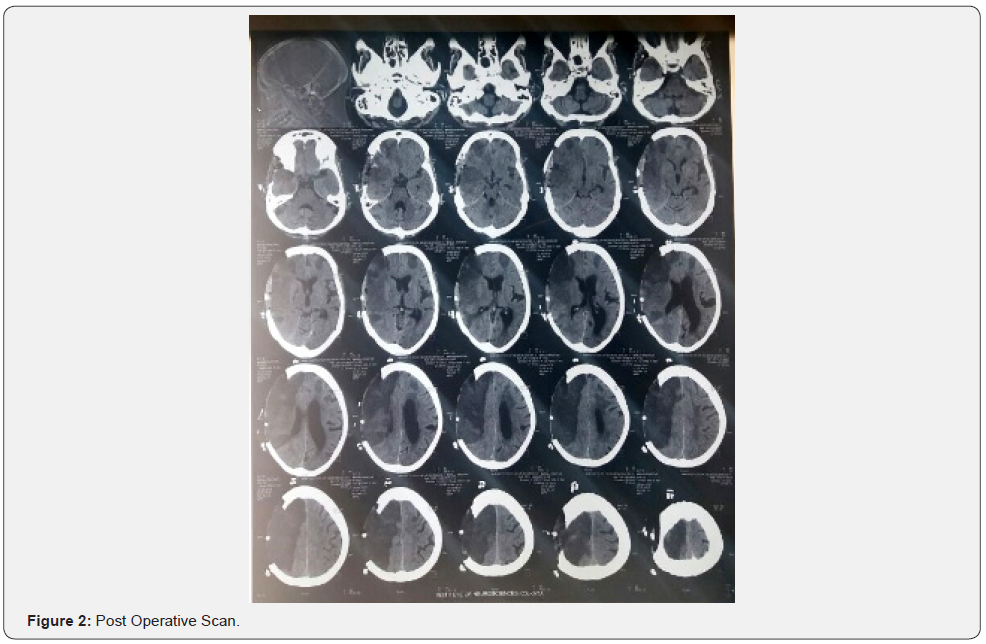
Ischemic area > 145 mL, even at early stages. Moreover, DWI ischemic volumes larger than 210 mL were found related to a 100% mortality in patients without surgical treatment Laboratory data [1] (Figures 1&2).
Serum astroglial protein S100B protein >1.03 mcg/L (Has 94% sensitivity and 83% specificity to predict massive cerebral edema) Unfortunately at this stage, this tool is not available in every hospital.
Intracranial pressure (ICP) monitoring
The role of ICP monitoring in patients with large cerebral infarctions is controversial. There is no absolute recommendation for a routine use of intracranial pressure monitoring. And it is not considered a risk-free procedure. Uncal herniation and anisocoria sometimes occur without an overall increase of ICP. In patients with a malignant MCA infarction, pupillary abnormalities and severe brainstem compression may be present despite normal ICP values. Therefore, continuous ICP monitoring cannot substitute for close clinical and radiological follow-up in the management of these patients. Other facts [2,3].
The side of the stroke does not seem to affect the vital status after surgical decompression, so it should not influence the choice to operate Patients older than 60 years are not ideal candidates for surgical decompression as they possess a lower neuronal plasticity and also frequently have more risk factors and comorbidities. However, older patients with a good antecedent condition hemicraniectomy seems somehow to improve the prognosis Surgery can be safely performed even after intravenous tissue plasminogen activator administration for thrombolysis.
Technical
The craniotomy should include the frontal, parietal, and temporal bones and its antero-posterior length should not be inferior to 12 cm larger openings up to 14 cm or more are thought to allow an even better pressure relieve. Particular attention has to be paid to decompression of the basal temporal area, as it represents a critical compartment with close relationship with the brainstem. In order to gain additional room, the dura mater is commonly opened as well. It can then be enlarged with a biological or synthetic substitute or left patent, just covered by hemostatic material for a faster closure the cerebral tissue itself should be completely preserved at surgery for recovery of the not deadly damaged areas, which may be not distinguishable from the infarction itself (Figure 3).

Conclusion
No absolute criteria for selection of surgical cases in stroke.
a. Clinical and radiological correlation,
b. Co-morbidities
c. Eagerness of family members to accept the disability
d. Cost factor for post-surgical rehabilitation in home.
To Know More About Open Access Journal of Neurology & Neurosurgery Please click on: https://juniperpublishers.com/oajnn/index.php




No comments:
Post a Comment