Abstract
Female infertility is one of the major reproductive health issue affecting majority of women worldwide. Several factors including environmental, hormonal and physical may affect the physiology of ovary to release quality grade oocyte required for fertilization and early embryonic development. The quality of oocyte is dependent on several factors within the follicular microenvironment and even after ovulation. One of the major factors that affect oocyte quality is the induction of apoptosis. Apoptosis plays a major role to eliminate majority of germ cells from the cohort of ovary during various stages of folliculogenesis. Few numbers of oocytes are selectively recruited to get ovulated during entire reproductive life span in female. Prior to ovulation, these oocytes achieve meiotic competency that may last for several months in rodents to several years in human. Inability to achieve meiotic competency within the follicular microenvironment and spontaneous egg activation (SEA) immediately after ovulation may deteriorate oocyte quality. Thus, induction of apoptosis or meiotic arrest at Metaphase-I stage (M-I) or SEA could reduce female fertility and may cause infertility.
Keywords: Apoptosis; Oocyte competency; Spontaneous egg activation; Ovary; Female infertility
Abbreviations: SEA: Spontaneous Egg Activation; M-I: Metaphase-I; M-II: Metaphase-II; M-III: Metaphase-III; PB-I: First Polar Body; PB-II: Second Polar Body; ROS: Reactive Oxygen Species
Introduction
Infertility is a one of the major reproductive health problems that has affected almost 10% of young age group worldwide. The infertility rate remains unchanged over past two decades besides having significant advancement in reproductive health sector [1]. This could be due to environmental, stress, lifestyle factor, hormonal and pathophysiological factors [2]. These factors directly or indirectly affect the physiology of ovary that is responsible for the generation of competent oocytes for fertilization and early embryonic development [3]. The increase of stress hormone induces granulosa cell apoptosis responsible for synthesis of estradiol-17β. Estradiol depletion at the level of ovary affects follicular growth and development [2]. Amelioration in follicular growth and development induces follicular atresia [4]. The increased stress causes oxidative stress and reactive oxygen species (ROS) at the level of ovary trigger germ cell depletion via apoptosis [5]. Several factors and pathways facilitate germ cell depletion at all the stages of oogenesis in mammals [6]. The large number of germ cells is eliminated from the cohort of ovary just before the attainment of puberty [4]. At puberty, less than 1% of germ cells remains in the ovary that are subjected to selective recruitment process during entire reproductive life span [7].
The selective recruitment of oocytes during puberty in response to pituitary gonadotrophin surge induces meiotic resumption from diplotene arrest in follicular oocytes by increasing the level of cyclic nucleotides as well as Mos level in granulosa cells of follicular oocytes [8]. These cyclic nucleotides and MOS/MEK/MAPK signalling pathways disrupt the gap junctions between granulosa cells and oocytes resulting in a transient decrease of oocyte adenosine 3',5'-cyclic monophosphate (cAMP) required to maintain diplotene arrest in follicular microenvironment [9]. A transient decrease of oocyte cAMP activates mitogen-activated protein kinase (MAPK) as well as cyclin dependent kinasel (Cdkl), a catalytic unit of maturation promoting factor (MPF). Further, decrease of cAMP destabilizes MPF [10]. The MPF destabilization causes meiotic resumption from diplotene arrest and oocyte progresses towards to metaphase-I stage (M-I) [11]. The M-I arrest may last for very short period of time in vivo and oocyte progresses to reach metaphase-II stage (M-II) by extruding first polar body (PB-I) at the time of ovulation [12]. However, removal of oocyte from follicular microenvironment and their culture in vitro results in spontaneous resumption of meiosis but they are unable to progress beyond M-I under in vitro culture conditions [13].
These oocytes are unfit for fertilization as they contain diploidset of chromosomes and do not posses PB-I. Further, growing body of evidences suggest that the oocytes after ovulation do not wait for fertilizing spermatozoa and quickly undergo meiotic exit from M-II arrest so called spontaneous activation in several mammalian species [14,15]. The spontaneous activation is possibly due to premature release of calcium (Ca++) from internal stores and increase of cytosolic free calcium. A moderate increase of cytosolic free calcium triggers downstream pathway to destabilize MPF [16]. MPF destabilization results spontaneous activation by initiating the extrusion of second polar body (PB-II). These oocytes are of poor quality and their use limits reproductive outcome and may trigger infertility problems [17].
Apoptosis and oocyte quality
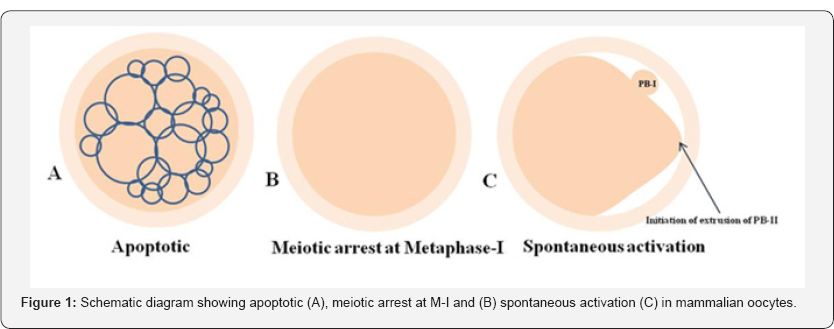
Apoptosis plays a major role in follicular atresia and eliminates majority of defective as well as surplus germ cells from the cohort of ovary [18,19]. By this way, ovary keeps only few numbers of germ cells (less than 1%) for selective recruitment during entire reproductive lifespan. As the aging occurs, decline of number of follicles below threshold level may cause infertility [20,21]. Studies suggest that the good quality of oocyte is ovulated first and as the maternal aging occurs, poor quality oocytes are remained in the ovary. These oocytes are more fragile and susceptible towards apoptosis that reduces reproductive outcome (Figure 1) [22-24]. Women are more frequently exposed to various kinds of stress during their reproductive period [25]. The psychological stress, lifestyle changes and various other factors stimulate the release of stress hormone and reactive oxygen species (ROS) [2]. The increased level of stress hormone and ROS induce apoptosis not only in granulosa cells but also in follicular oocytes [5,26]. There are several players and both as death receptors as well as mitochondria-mediated pathways involved in oocyte apoptosis within the follicle of the ovary [27,28]. Indeed, apoptosis plays a major role in determining the quality of follicular oocytes that directly affects reproductive outcome of a female and induces infertility [4].
Meiotic maturation arrest and oocyte quality
Meiotic maturation is required for the follicular oocytes to achieve developmental competency [29]. The achievement of meiotic competency starts with the resumption from diplotene arrest in follicular oocytes and ends with extrusion of PB-I [16]. Any defect during the achievement of meiotic competency does not allow the follicular oocyte to progress meiosis [30]. These compromised oocytes are arrested at M-I stage and do not progress to extrude PB-I [12,13,31]. Further, M-II arrested oocytes even after insemination do not get activated [32]. These oocytes are of poor quality due to meiotic maturation arrest either at M-I stage or at M-II stage under in vitro culture conditions (Figure 1B) [3,33]. The meiotic maturation failure could be possibly due to maintenance of high level of stabilized MPF. The high level of stabilized MPF is required for the maintenance of meiotic arrest [34,35]. The meiotic maturation arrest may cause infertility in human [3].
Spontaneous activation and oocyte quality
The oocyte after ovulation are generally arrested at M-II stage and posses PB-I in most of the mammalian species [3538]. Growing body evidences suggest that oocyte do not wait for fertilizing spermatozoa and quickly undergo spontaneous exit from M-II arrest in several mammalian species including human [39-42]. The initiation of extrusion of PB-II starts but never gets completely extrude (Figure 1C). Oocytes are further arrested at Metaphase-III (M-III) like stage [43].The SEA could be due to abortive increase of cytosolic free calcium and activation of downstream pathway to destabilize MPF [37,38,44]. A moderate increase of cytosolic free Ca++ is good enough to trigger SEA but not sufficient to induce full activation process [37,44]. These oocytes are not fit for fertilization since the chromosomes are scattered throughout the cytoplasm. A large amount of cytoplasm goes towards the side of polar body formation but PB-II never completely extruded [11]. These oocytes are of poor quality and cannot be used for any assisted reproductive technology (ART) program including somatic cell nuclear transfer program (SCNT) during animal cloning [36,11].
Conclusion
Good quality of oocytes is the right choice for fertilization and early embryonic development. Deterioration in oocyte quality may occur due to the onset of apoptosis in the follicular oocytes. Majority of oocytes are eliminated from ovary via apoptosis during follicular atresia. Only few oocytes remain in the ovary that are selectively recruited for ovulation during entire reproductive life of a female. Prevention of MPF destabilization may cause meiotic maturation arrest in follicular oocytes. After ovulation, oocyte quality undergoes Ca++ mediated MPF destabilization that causes SEA in several mammalian species including human. Thus, apoptosis in oocytes, meiotic maturation arrest and SEA may deteriorate oocyte quality after ovulation. Poor quality oocyte directly impacts the reproductive outcome and causes female infertility.





No comments:
Post a Comment